Before you start a new medication, especially one with serious risks, you need to know if it’s covered by a REMS program. REMS stands for Risk Evaluation and Mitigation Strategy. It’s not just paperwork-it’s a safety net designed by the U.S. Food and Drug Administration (FDA) to make sure the benefits of a drug outweigh its dangers. If you skip checking REMS requirements, you could face delays, denied prescriptions, or worse-serious side effects that could have been prevented.
What Is a REMS Program and Why Does It Matter?
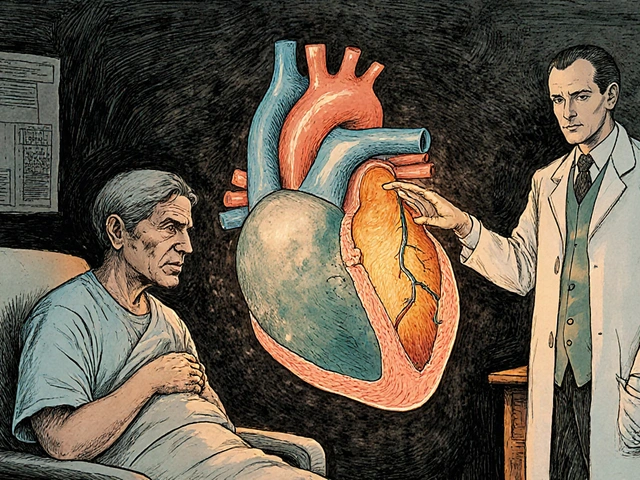
REMS programs were created in 2007 after Congress passed the Food and Drug Administration Amendments Act. They’re required for medications that carry serious risks-like birth defects, life-threatening infections, addiction, or sudden death. The FDA doesn’t use REMS to block access. It uses them to allow access safely. Without REMS, drugs like isotretinoin (for severe acne) or thalidomide (for multiple myeloma) wouldn’t be available at all. There are 76 active REMS programs as of 2025. Some are simple-like giving patients a printed Medication Guide. Others are complex. For example, Zyprexa Relprevv can only be given in certified clinics because it can cause sudden drowsiness or confusion after injection. Patients must be monitored for at least three hours. That’s not optional. That’s the law.How to Find Out If Your Medication Has a REMS Program
You can’t rely on your doctor or pharmacist to remember every REMS rule. You need to check yourself. Here’s how:- Look at the prescribing information. Every FDA-approved drug has a detailed document called the Prescribing Information (or “package insert”). It’s usually available on the manufacturer’s website or through DailyMed. If the drug has a REMS, it’s listed under Section 17-“Patient Counseling Information.”
- Use the FDA REMS Public Dashboard. Go to fda.gov/drugs/rems. You can search by drug name, company, or condition. The dashboard shows you exactly what’s required: prescriber certification? Patient registry? Lab tests? Facility restrictions?
- Check the manufacturer’s REMS website. Many drugs have their own dedicated REMS site. For isotretinoin, it’s ipleDGEprogram.com. For mycophenolate, it’s mycophenolaterems.com. These sites have enrollment forms, training videos, and FAQs.
- Ask your pharmacy. Pharmacists are on the front lines. If they can’t fill your prescription, it’s often because REMS requirements weren’t met. Call them before you go in. Ask: “Does this drug need a REMS program? What do I need to do?”
Common REMS Requirements You Might Encounter
Not all REMS are the same. Here’s what you might run into:- Medication Guides: A paper handout you must receive every time you fill the prescription. It explains the risks in plain language. Don’t throw it away. Read it.
- Prescriber Certification: Your doctor must complete training and register in the REMS system. For drugs like thalidomide or lenalidomide, this takes about an hour. If your doctor hasn’t done it, you won’t get the drug.
- Patient Enrollment: You might need to sign up in a registry. For isotretinoin, both you and your doctor must register in iPLEDGE. You’ll need to pass monthly pregnancy tests if you’re a woman of childbearing age.
- Lab Monitoring: Some drugs require blood tests before and during treatment. For example, clozapine requires weekly white blood cell counts for the first six months because it can cause a deadly drop in white blood cells.
- Restricted Distribution: The drug can only be dispensed by certain pharmacies or given in specific clinics. This applies to drugs like Zyprexa Relprevv or Opioid Analgesics under the Opioid REMS program.
What Happens If You Skip REMS Steps?
It’s not just about getting your prescription filled. Skipping REMS requirements puts you at risk. If you take isotretinoin without registering in iPLEDGE, you could become pregnant and have a baby with severe birth defects. If you get thalidomide without proper training, you might not know how to handle it safely or recognize early signs of nerve damage. And if you take an opioid without completing the required education, you might not understand the risks of addiction or overdose. Pharmacies are required to refuse dispensing if REMS steps aren’t completed. That means even if your doctor writes the script, the pharmacy won’t fill it. You’ll waste time, miss doses, and risk your health.How Long Does REMS Verification Take?
It varies. For a simple Medication Guide, it’s a few minutes. For something like iPLEDGE, it can take days. The average time to complete REMS steps is 6-12 business days, according to a 2022 survey by the National Organization for Rare Disorders. Here’s a realistic timeline:- Day 1: Doctor checks REMS status and decides to prescribe.
- Day 2-3: Doctor completes certification (if needed). This might involve logging into a website, watching a video, and answering quiz questions.
- Day 3-5: You enroll in the patient registry. You may need to sign forms, provide ID, or schedule a pregnancy test.
- Day 5-7: Pharmacy receives the prescription and verifies your enrollment.
- Day 7-10: You pick up the medication.
Who’s Responsible for REMS Compliance?
Everyone plays a role:- Doctors: Must be certified, complete training, and document compliance.
- Pharmacists: Must verify enrollment, check lab results, and refuse to dispense if requirements aren’t met.
- Patients: Must enroll, complete required tests, and follow safety rules.
- Manufacturers: Must maintain the REMS system, update training materials, and report compliance data to the FDA.

Recent Changes to REMS Programs (2023-2025)
REMS isn’t static. The FDA is actively improving them. In March 2023, the FDA launched a new version of the REMS Public Dashboard with real-time updates and mobile-friendly design. In April 2023, they required all new REMS programs to include smartphone tools-like apps that send reminders for lab tests or pregnancy screenings. Eight of the top 10 pharmacy benefit managers now integrate REMS checks directly into e-prescribing systems. That means your doctor’s electronic system might flag a REMS requirement before the prescription even leaves the office. The FDA also started modifying existing REMS to reduce burden. In 2022 alone, 14 REMS programs were simplified-cutting paperwork, reducing lab frequency, or allowing telehealth for training. The goal: keep patients safe without making access impossible.What to Do If You’re Facing a REMS Delay
If your medication is stuck because of REMS, don’t give up. Here’s what to do:- Ask your doctor for help. They might not realize how long REMS takes. Ask them to call the manufacturer’s REMS support line. Most have dedicated staff to help providers.
- Call the REMS program directly. For example, iPLEDGE has a 24/7 helpline. Mycophenolate REMS has live chat. Don’t wait for email.
- Ask for a temporary alternative. If your drug has a similar alternative without REMS, ask your doctor. Sometimes, switching for a few weeks avoids a months-long delay.
- Document everything. Keep copies of all forms, emails, and call logs. If you’re denied care, this helps you appeal.
Bottom Line: Don’t Guess. Check.
REMS isn’t bureaucracy-it’s protection. But it only works if you know it’s there. Always check REMS requirements before starting any new medication, especially if it’s for cancer, mental health, autoimmune disease, or pregnancy-related risks. Use the FDA dashboard. Talk to your pharmacist. Read the Medication Guide. Don’t assume your doctor already handled it. And never skip steps-even if it’s inconvenient. The risks aren’t theoretical. They’re real. And they’re preventable.What happens if I don’t complete my REMS requirements?
If you don’t complete REMS requirements, your pharmacy will not dispense the medication. This is not optional. For drugs like isotretinoin or thalidomide, skipping steps can lead to serious harm-such as birth defects or life-threatening side effects. Even if your doctor writes the prescription, the pharmacy is legally required to refuse it until all REMS steps are verified.
Do I need to do REMS training every time I refill my prescription?
No. Once you’re enrolled in a REMS program (like iPLEDGE or Mycophenolate REMS), you typically only need to complete training or certification once. However, you may need to renew your enrollment annually or complete lab tests monthly. Always check the specific rules for your drug-some require yearly re-certification for prescribers, and patients may need to re-enroll if they stop taking the drug for more than 30 days.
Can my pharmacist help me with REMS enrollment?
Yes. Pharmacists are trained to help with REMS verification. They can confirm if your doctor is certified, check your patient registry status, and even guide you to the right website. Many pharmacies now have REMS specialists on staff. Don’t hesitate to ask them for help-you’re not alone in this process.
Are REMS programs only for brand-name drugs?
No. REMS programs apply to both brand-name and generic drugs. If the original drug had a REMS, the generic version must follow the same rules. For example, if you’re prescribed generic isotretinoin, you still need to enroll in iPLEDGE. The FDA requires this to ensure consistent safety across all versions of the medication.
How do I know if a REMS program has changed?
The FDA updates the REMS Public Dashboard regularly, but changes can take up to two weeks to appear. To stay current, sign up for email alerts from the manufacturer’s REMS website. Also, check your Medication Guide each time you refill-it’s updated if requirements change. If you’re unsure, call the REMS program’s helpline or ask your pharmacist.







Ibrahim Yakubu
I’ve been through this with isotretinoin. iPLEDGE is a nightmare. Took me three weeks just to get my first blood test scheduled. My doctor didn’t even know the system updated last month. You think you’re getting a prescription, but you’re signing up for a government-sponsored obstacle course.
And don’t get me started on the pharmacy. I showed up with all my paperwork, and they said, ‘Oh, your prescriber hasn’t synced yet.’ Like, what? I’m the patient. Why am I the one chasing paperwork?
Meanwhile, my acne is screaming. I’m not asking for luxury-I’m asking for basic access. But no. We’ve turned medical care into a bureaucratic performance art piece.
And yes, I read the Medication Guide. I signed the forms. I watched the videos. But none of it matters if the system is broken. REMS isn’t safety-it’s a delay tactic disguised as care.
Brooke Evers
I just want to say how much I appreciate this post. I’ve been a nurse for 18 years and I’ve seen too many patients get stuck because no one explained REMS clearly. It’s not that people are lazy-it’s that the system is confusing, fragmented, and overwhelming.
I had a 19-year-old girl last month who was terrified of starting her medication because she didn’t know what ‘iPLEDGE’ even meant. We sat together for 45 minutes and walked through every step. She cried when she finally got her script. Not from sadness-from relief.
Doctors are overworked. Pharmacists are understaffed. Patients are left in the middle. But when someone takes the time to explain it in plain language, like this post does? It changes everything.
Please keep sharing this. People need to know they’re not alone in this mess. And they need to know it’s okay to ask for help. You’re not being difficult-you’re being responsible.
Chris Park
Let’s be real. REMS isn’t about safety-it’s about corporate liability. The FDA doesn’t care if you get your medicine. They care that if you die, the manufacturer won’t get sued.
Thalidomide? Was banned in the 60s because babies were born with flipper limbs. Now it’s back, with a $2000/year compliance fee, and we’re calling it ‘progress’?
Meanwhile, the same FDA approved opioids with zero REMS for decades. Thousands died. Now they’re slapping REMS on drugs that treat cancer and autoimmune disease? Coincidence?
Also, the ‘Medication Guide’? It’s printed in 5pt font on recycled paper. You need a magnifying glass and a PhD in legalese to read it.
This isn’t protection. It’s a smoke screen. And the people who benefit? The lawyers, the pharmaceutical lobbyists, and the bureaucrats who get paid to ‘manage risk.’ Not you.
Saketh Sai Rachapudi
REMS is just american way of controling poor people. In india we dont need all this paper work. We just take medicine and live. This is why america is sick. You make everything hard for no reason. My cousin died because he couldnt get his drug on time because of REMS. This is not healthcare. This is bureaucracy terrorism.
joanne humphreys
I think the real issue here isn’t the REMS system itself-it’s how little communication happens between the people who need it and the people who run it.
I’ve been on a drug with REMS for two years now. I’ve learned to check the dashboard every month. I’ve memorized the helpline number. I know which pharmacy in my city actually has a REMS specialist on staff.
But I didn’t learn any of that from my doctor. I learned it from a Reddit thread three years ago. That’s the problem. This information should be handed to you at the time of prescription-not found by accident in a comment section.
Maybe the solution isn’t to remove REMS, but to make it more visible. Like a pop-up in the e-prescribing system that says, ‘This drug requires REMS. Here’s what to do next.’
Simple. Direct. Human.
Nigel ntini
This is exactly the kind of post that should be mandatory reading for every new patient. I wish I’d had this when I started my first REMS drug. I thought the pharmacist was just being difficult when they refused to fill it.
Turns out, I was the one who didn’t know the rules.
Now I’m the guy who helps my friends navigate this stuff. I’ve walked three people through iPLEDGE. One of them was 72 and had never used a computer before. We did it together-phone in one hand, laptop in the other.
It’s not perfect. But if we treat REMS like a team sport instead of a trap, it works.
And honestly? If you’re willing to do the steps, you’re already ahead of 90% of people. Don’t let the frustration make you give up.
Priya Ranjan
You people are making such a fuss over something that should be obvious. If a drug can kill you or cause birth defects, then of course you need rules. This isn’t a privilege-it’s a responsibility.
I work in pharma compliance. I’ve seen the files. People die because they skip steps. Not because the system is broken. Because they think they’re too smart for it.
My sister took isotretinoin without registering. Her baby had a cleft palate. Do you think she wanted that? No. But she didn’t read the guide. She didn’t ask. She assumed.
So don’t complain about paperwork. Complain about arrogance.
And yes, generics are included. If you don’t know that, you shouldn’t be taking the drug at all.
Gwyneth Agnes
Stop whining. REMS saves lives. Read the guide. Do the test. Get the script. It’s not that hard.
Ashish Vazirani
Let me tell you what REALLY happens behind the scenes. The FDA doesn’t care about you. They care about lawsuits. The pharmaceutical companies? They love REMS. Why? Because it creates artificial scarcity. Fewer people get the drug → higher prices → bigger profits.
I’ve seen it. My uncle got prescribed a REMS drug for psoriasis. The cost? $12,000 a month. But the generic? $800. Except the generic is blocked by REMS because the brand-name company paid to keep it locked down.
And the ‘Medication Guide’? It’s written by lawyers. Not doctors. Not patients. Lawyers.
So yes, I’ll check the dashboard. But I’m not fooled. This isn’t safety. It’s capitalism with a stethoscope.
Mansi Bansal
It is with profound gravity that I address the current discourse surrounding REMS protocols. The structural integrity of pharmaceutical risk mitigation frameworks is not merely a procedural formality; it is a solemn covenant between the regulatory apparatus and the citizenry.
One cannot, in good conscience, dismiss the exigencies of compliance as bureaucratic inertia. The historical precedent of thalidomide, as documented in the annals of medical jurisprudence, remains an indelible testament to the catastrophic consequences of negligence.
Moreover, the assertion that REMS impedes access is, in my estimation, a mischaracterization born of impatience rather than principle. The system is not designed to obstruct-it is engineered to safeguard.
One must approach such matters with the solemnity befitting a life-or-death calculus. To treat REMS as an inconvenience is to trivialize the sanctity of human physiology.
Kindly consult the manufacturer’s portal. Submit all documentation. Adhere to timelines. There is no room for cavalier attitudes when the stakes are biological integrity.
Kay Jolie
Okay, but let’s be honest-REMS is the ultimate influencer marketing for Big Pharma. They’ve turned ‘patient safety’ into a brand. ‘iPLEDGE’? That’s not a program. That’s a lifestyle.
And the fact that they now require smartphone apps for pregnancy reminders? That’s not healthcare. That’s a wellness startup with a FDA stamp.
I mean, I get it. I’m all for not having babies with deformities. But do we really need a 12-step verification process to get a drug that’s been around since 1982?
Also, why does the Medication Guide look like it was designed by a 1998 AOL user? The fonts. The colors. The spacing. It’s like they’re trying to scare you off.
It’s not safety. It’s brand experience.
pallavi khushwani
I used to think REMS was just red tape. Then I got prescribed clozapine. I didn’t know what a WBC count was. I thought my doctor just wanted to ‘check on me.’
Turns out, if that number drops too low, you can die overnight. No warning. No symptoms. Just… gone.
So now I get my blood drawn every week. I log into the portal. I answer the same quiz every time. It’s annoying. But I don’t mind. Because I’m still here.
And honestly? I’m grateful. Not because the system is perfect. But because someone, somewhere, decided it was better to be safe than sorry.
Maybe we don’t need to fix REMS. Maybe we just need to stop treating it like a burden-and start treating it like a lifeline.
Billy Schimmel
So let me get this straight. You’re telling me I have to register, get tested, watch a video, and wait 10 days just to get a pill that could’ve been handed to me in 2005?
Meanwhile, I can buy fentanyl online in 3 clicks.
That’s not safety. That’s irony with a prescription pad.
Shayne Smith
I just started a REMS drug last month. Didn’t know what I was getting into. Thought my doctor handled it.
Turns out? I had to call the REMS line myself. They put me on hold for 22 minutes. Then a woman named Linda talked me through everything. She was sweet. Patient. Didn’t judge me for not knowing.
Now I’m the one telling my friends how to do it.
It’s not perfect. But people like Linda? They make it bearable.
Kumar Shubhranshu
REMS is mandatory. If you skip it you're asking for trouble. End of story.
Brooke Evers
Just wanted to reply to @5660-you’re right that the system is flawed. But blaming the FDA for corporate greed misses the point. The FDA doesn’t own the REMS portals. The manufacturers do. They’re the ones who design the websites, the quizzes, the enrollment forms.
And honestly? Some of them are terrible. iPLEDGE is a mess. But Mycophenolate REMS? Clean, simple, mobile-friendly.
The problem isn’t the idea. It’s the execution. And the only way to fix that is to demand better. Not to give up on the whole system.
Maybe we need a public petition. Or a Reddit thread that gets shared with Congress.
Because if we don’t speak up, nothing changes.