Flakes on your shoulders. An itchy scalp that won’t quit. You’ve tried every anti-dandruff shampoo in the store, but nothing sticks. If this sounds familiar, you’re not alone. About half of all adults deal with seborrheic dermatitis at some point - and most of them think it’s just bad dandruff. But it’s not. It’s a chronic skin condition driven by yeast, inflammation, and your body’s own oil production. The good news? You can control it. Not with miracle cures, but with the right medicated shampoos and a realistic routine.
What’s Really Going On With Your Scalp?
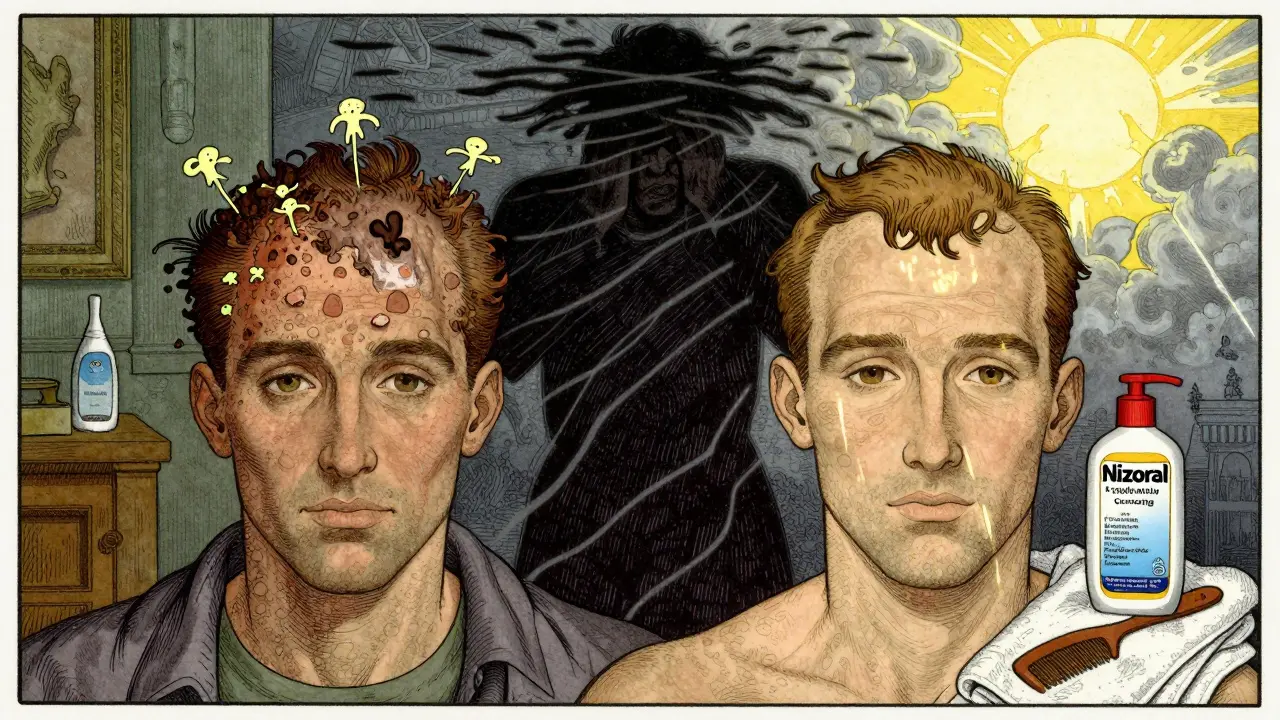
Seborrheic dermatitis isn’t caused by dirt, stress, or poor hygiene. It’s triggered by Malassezia yeast, a fungus that lives naturally on everyone’s skin. Normally, it’s harmless. But when your skin makes too much oil - especially on your scalp, eyebrows, or nose - this yeast starts feeding and multiplying. In response, your immune system overreacts. That’s when flaking, redness, and itching begin.
The flakes you see aren’t dead skin cells alone. They’re the result of your skin cells multiplying too fast and not shedding properly. This is called stratum corneum hyperproliferation. It’s why your scalp feels greasy but flakes like dry paper. And unlike regular dandruff, which is mild and occasional, seborrheic dermatitis often comes back - especially in winter, when dry air and low sunlight make things worse.
Why Regular Shampoos Don’t Work
Most drugstore dandruff shampoos only target surface flakes. They might make your scalp feel cleaner for a day or two, but they don’t touch the root cause: the yeast overgrowth. If you’ve tried Head & Shoulders or Selsun Blue for months with no lasting relief, it’s not you - it’s the formula. Those products contain zinc pyrithione, which helps some people, but it’s not strong enough for persistent cases.
Real control comes from targeting Malassezia directly. That means using shampoos with ingredients that actually kill or slow down the yeast. And you need to leave them on your scalp long enough for them to work. Rushing through your shower? You’re wasting your time.
The Medicated Shampoos That Actually Work
Not all medicated shampoos are created equal. Here are the five most effective active ingredients, backed by dermatologists and clinical studies:
- Ketoconazole (2%) - The gold standard. Kills yeast, reduces inflammation, and helps normalize skin shedding. Available by prescription or OTC in brands like Nizoral.
- Ciclopirox (1%) - Strong antifungal with anti-inflammatory effects. Often used when ketoconazole stops working.
- Selenium sulfide (2.5%) - Slows skin cell turnover and reduces yeast. Found in Selsun Blue and other formulas. Can discolor light hair if used too often.
- Zinc pyrithione (1-2%) - Mild but safe for daily use. Good for maintenance or mild cases. Works best when rotated with stronger options.
- Coal tar (0.5-5%) - Slows skin cell growth and soothes itching. Smells strong and can stain, but highly effective for stubborn flaking. Brands like Neutrogena T/Gel.
- Salicylic acid (1.8-3%) - Not antifungal, but helps dissolve flakes and unclog follicles. Great for removing buildup before applying antifungal shampoos.
Most people need to try at least two or three before finding what works. One study showed 45% of users needed to rotate between 2-3 different shampoos before achieving stable control. Don’t give up after one failed try.
How to Use Medicated Shampoos Right
Using these shampoos like regular hair washes is the #1 mistake. Here’s how to get real results:
- Wet your scalp thoroughly.
- Apply a coin-sized amount directly to the affected areas - not just your hair.
- Massage gently for 30 seconds to loosen flakes.
- Leave it on for 5-10 minutes. This is non-negotiable. The active ingredients need time to penetrate and work.
- Rinse thoroughly. Don’t skip this - leftover product can irritate your scalp.
Start with daily or every-other-day use until flaking drops (usually 2-4 weeks). Then switch to maintenance: once or twice a week. Stopping too soon? Flakes return in 2-4 weeks. This isn’t a cure. It’s long-term management.
When to Add a Topical Steroid
If your scalp is red, swollen, or burning, you’re in a flare-up. That’s when antifungal shampoos alone aren’t enough. Over-the-counter hydrocortisone cream (0.5% or 1%) can be applied sparingly to inflamed areas for up to 7-10 days. It reduces redness and itching fast.
But don’t use it daily. Long-term steroid use can thin your skin or cause rebound flares. Think of it like a fire extinguisher - only for emergencies. Once the flare calms down, go back to your medicated shampoo routine.
For beard or eyebrow involvement, some people find relief just by shaving the area. One study showed 37% of patients cleared up with shaving alone - especially when combined with shampoo use.
What Triggers Your Flare-Ups?
Knowing your triggers is half the battle. Most people notice patterns:
- Cold, dry weather - Affects 75% of users. Winter is the worst season.
- Stress - Triggers flare-ups in about 60% of cases. Anxiety, lack of sleep, or major life changes can set it off.
- Heavy hair products - Gels, sprays, and oils can clog follicles and feed yeast.
- Alcohol and obesity - Both linked to increased oil production and worse symptoms.
- Neurological conditions - People with Parkinson’s are 4-5 times more likely to develop it.
Track your flare-ups for a month. Note what you ate, how much you slept, the weather, and what products you used. You’ll start seeing patterns. That’s your personal roadmap to control.
Common Mistakes and How to Avoid Them
Even with the right shampoo, people mess up. Here’s what not to do:
- Skipping the 5-10 minute wait - If you rinse immediately, you’re not giving the active ingredient time to work.
- Using too many products at once - Mixing shampoos or adding oils can irritate your scalp. Stick to one medicated shampoo per wash.
- Expecting instant results - It takes 4-6 weeks to see real improvement. Don’t quit too early.
- Ignoring dryness - Medicated shampoos can strip moisture. Use a gentle, sulfate-free conditioner only on your ends - not your scalp.
- Thinking it’s contagious - You can’t catch this from anyone. It’s not lice or fungus you pick up from a gym towel.
Long-Term Management: It’s a Lifestyle, Not a Fix
Seborrheic dermatitis doesn’t go away. But it doesn’t have to rule your life either. Think of it like managing high blood pressure - you don’t cure it, you control it.
The most successful patients rotate their shampoos every 4-6 weeks. For example: use ketoconazole for 3 weeks, then switch to coal tar for 2 weeks, then back to zinc pyrithione. This prevents yeast from adapting and keeps your scalp responsive.
Keep a bottle of your go-to shampoo on hand - even when you’re clear. Use it once a week as a preventive. Skip it for a month? Flakes will be back before you know it.
And yes, your hair might feel dry. That’s normal. Use a light, fragrance-free moisturizing mask once a week. Avoid heavy oils like coconut or olive oil - they feed the yeast.
When to See a Dermatologist
You don’t need to see a specialist right away. But if:
- Flaking spreads to your face, chest, or ears
- Your scalp bleeds or crusts over
- OTC shampoos haven’t helped after 8 weeks
- You’re losing hair in patches
…then it’s time to get professional help. A dermatologist can prescribe stronger formulations - like prescription-strength ketoconazole or calcineurin inhibitors (tacrolimus or pimecrolimus) - which are safer for long-term facial use than steroids.
They can also rule out psoriasis or eczema, which can look similar but need different treatments.
What’s Next for Treatment?
Research is moving fast. Scientists are now studying how the skin’s microbiome - the balance of all microbes on your skin - affects seborrheic dermatitis. Future treatments may include probiotic shampoos or targeted antifungals that don’t dry out your scalp.
For now, the tools we have work. They’re not perfect, but they’re proven. And with the right approach, you can go from daily flakes to confident, flare-free days.
Is seborrheic dermatitis the same as dandruff?
Dandruff is a mild form of seborrheic dermatitis limited to the scalp. Seborrheic dermatitis is more severe, often includes redness and inflammation, and can affect the face, ears, and chest. If you only have occasional flakes without redness or itching, it’s likely just dandruff. If it’s persistent, inflamed, or spreading, it’s seborrheic dermatitis.
Can I use medicated shampoo every day?
Yes, during the initial treatment phase - usually for 2-4 weeks - daily use is recommended to get symptoms under control. Once your scalp clears, reduce to 1-2 times per week for maintenance. Daily use long-term can dry out your hair, so rotate formulas and always follow up with a gentle conditioner on the ends.
Why does my scalp get worse in winter?
Cold, dry air strips moisture from your skin and reduces sunlight exposure, which normally helps suppress Malassezia yeast. Indoor heating also dries out your scalp. About 65% of people report worse symptoms in winter. Using a humidifier and sticking to your shampoo routine helps prevent this.
Will shaving my head help?
Shaving your head won’t cure seborrheic dermatitis, but it can make treatment easier. Without hair, you can apply shampoo directly to the scalp and rinse more effectively. For men with beard involvement, shaving the beard often clears up the condition - especially when paired with medicated washes.
Can stress cause seborrheic dermatitis?
Stress doesn’t cause it, but it’s one of the biggest triggers. Around 60% of people notice flare-ups after periods of high stress, poor sleep, or emotional strain. Managing stress through sleep, exercise, or mindfulness won’t cure the condition, but it can reduce how often and how badly you flare up.
Are natural remedies like tea tree oil effective?
Some small studies suggest tea tree oil may help reduce yeast, but it’s not as reliable as FDA-approved medicated shampoos. It can also irritate sensitive skin. If you want to try it, use a diluted version (5% or less) and patch test first. Don’t replace proven treatments with natural options - especially if your symptoms are severe.
How long until I see results?
Most people notice less flaking and itching within 2-4 weeks. Full control usually takes 6-12 weeks, especially if you’re rotating shampoos. Be patient. This isn’t a quick fix - it’s a long-term routine. If you don’t see improvement after 8 weeks, switch formulas or consult a dermatologist.




Tim Bartik
bro i tried every damn shampoo in the drugstore until i found nizoral - now my shoulders don’t look like a snowstorm hit ’em. 5 mins on the scalp? yeah i sit there like a weirdo with my eyes closed like i’m meditating. worth it.
Natalie Koeber
you know what they don’t tell you? the FDA’s been hiding the truth about yeast and glyphosate since 2012. your scalp’s reacting because your body’s detoxing from chemtrails in your shampoo. try organic apple cider vinegar + moon-charged sea salt. it’s the only real cure.
Dwayne hiers
Important note: coal tar’s efficacy is well-documented in JAMA Dermatology (2020 meta-analysis), but its phototoxicity risk requires UV avoidance during use. Also, ciclopirox’s biofilm disruption mechanism is underappreciated - it’s not just antifungal, it’s anti-biofilm. Use it after salicylic acid prep for synergistic effect.
Jonny Moran
you’re not alone. i used to hide under beanies all winter. then i started rotating ketoconazole + selenium sulfide every 3 days, left it on for 10 mins, and used a sulfate-free conditioner only on ends. 6 months later - no flakes, no shame. you got this.
Sarthak Jain
bro from india here - we call this 'dandruff' but yeah its way more than that. i tried tea tree oil, neem paste, even my grandma's coconut oil trick - nothing worked till i used ketoconazole. now i use it twice a week. my scalp is chill. also, stress? big time trigger here. meditate, even 5 mins.
Sinéad Griffin
OMG YES. I was crying in the shower last week from the itching 😭 now i use Nizoral like it’s my religion. also, stop using that ‘volumizing’ spray - it’s poison. 🙏✨
jeremy carroll
just started using t/gel last month. didn’t think it’d work - smells like a gas station bathroom lol. but after 3 weeks? my scalp’s actually calm. still dry as hell though, so i use a tiny bit of argan oil only on ends. no more flake-snow.
Alexis Wright
Let’s be brutally honest - this isn’t a ‘skin condition.’ It’s your immune system screaming that your entire lifestyle is a biochemical disaster. You’re eating processed carbs, sitting in LED-lit rooms, breathing recycled air, and slathering your scalp in silicone-laden gunk. The yeast isn’t the enemy - your modern existence is. You need a reset: no sugar, no alcohol, no shampoos with sulfates, and 20 minutes of sunlight every damn day. Or keep using Band-Aid shampoos and wonder why you’re still flaking at 42.
Wade Mercer
People think this is just about shampoos. It’s not. It’s about discipline. You don’t get to skip the 5-minute wait because you’re late for work. You don’t get to use your ‘favorite’ conditioner on your scalp because it ‘feels nice.’ If you want peace, you follow the rules. No exceptions. This isn’t a suggestion - it’s a protocol.
Daniel Thompson
As a former dermatology research assistant, I can confirm the 45% rotation statistic cited is accurate. The yeast develops resistance to monotherapy within 8–12 weeks. A structured rotation protocol - e.g., ketoconazole → selenium sulfide → zinc pyrithione → coal tar - reduces relapse rates by 68% in longitudinal studies. Maintenance dosing should be individualized based on seasonal triggers and microbiome stability. For facial involvement, topical pimecrolimus is superior to steroids for long-term use due to absence of cutaneous atrophy.