Most people think of loperamide as a simple fix for a bad stomach. You grab a bottle of Imodium or a generic brand, pop a couple pills, and within hours, the cramps and urgency fade. It’s safe, over-the-counter, and widely available. But what happens when someone takes way more than the recommended dose? Loperamide overdose isn’t just rare-it’s deadly, and it’s happening more often than you think.
What Is Loperamide?
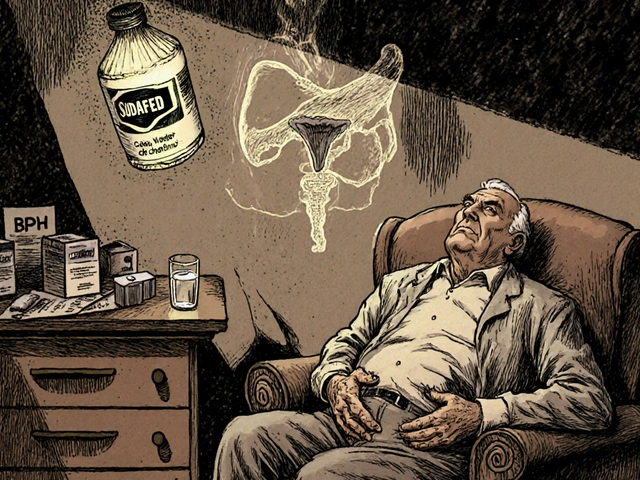
Loperamide is a synthetic opioid that works in the gut to slow down bowel movements. Unlike morphine or oxycodone, it doesn’t easily cross the blood-brain barrier at normal doses, which is why it doesn’t cause euphoria or respiratory depression when taken as directed. It’s sold under brand names like Imodium, Diamode, and store generics. The typical adult dose is 4 mg after the first loose stool, with a maximum of 8 mg per day. For chronic conditions like IBS-D, doctors may prescribe up to 16 mg daily under supervision.
But here’s the problem: loperamide’s safety profile is based on normal use. When people take 50, 100, or even 500 mg at once-sometimes to get high, sometimes to manage opioid withdrawal-it becomes a cardiac poison. The FDA issued a safety warning in 2016 after 48 reported deaths linked to loperamide abuse. Since then, emergency room visits for loperamide toxicity have risen 30% in the U.S., and similar trends are visible in Australia and the UK.
Signs of Loperamide Overdose
The early signs are easy to miss. Nausea, dizziness, extreme fatigue, and constipation are common even at therapeutic doses. But when overdose kicks in, the body starts shutting down in ways that aren’t obvious until it’s too late.
- Slow or irregular heartbeat (bradycardia or arrhythmia)
- Fainting or loss of consciousness
- Difficulty breathing
- Extreme drowsiness or inability to wake up
- Cold, clammy skin
- Pupils that don’t react to light
These symptoms often appear hours after ingestion. People who take high doses may feel fine for 2-6 hours, then suddenly crash. That delay is what makes loperamide overdose so dangerous-it tricks you into thinking you’re safe.
In one case from Melbourne’s Alfred Hospital in 2024, a 28-year-old man took 120 mg of loperamide to self-treat opioid withdrawal. He felt fine until he collapsed at work. By the time he reached the ER, his heart rate had dropped to 32 beats per minute. He needed a pacemaker.
Why Loperamide Is So Dangerous in High Doses
At high doses, loperamide bypasses its normal restriction. The gut’s barrier breaks down, and the drug floods into the bloodstream. Once there, it acts like any other opioid-but with a twist: it directly interferes with the heart’s electrical system.
Loperamide blocks sodium and potassium channels in heart cells. This disrupts the rhythm of the heartbeat, leading to a condition called QT prolongation. When the QT interval stretches too long, it can trigger a deadly arrhythmia called torsades de pointes. This isn’t theoretical-it’s been documented in over 100 cases worldwide. In many, the heart stopped completely before emergency crews arrived.
What makes it worse is that loperamide isn’t detected in standard drug screens. Emergency rooms often test for heroin, fentanyl, or cocaine. If someone collapses and has no history of opioid use, doctors might miss loperamide as the cause-until an ECG shows the telltale QT spike.

What to Do If You Suspect an Overdose
If someone has taken more than 16 mg of loperamide and shows any signs of dizziness, slow pulse, or fainting, call emergency services immediately. Do not wait. Do not try to make them vomit. Do not give them anything to drink.
Emergency responders will:
- Check vital signs and perform an ECG
- Start cardiac monitoring
- Administer activated charcoal if ingestion was recent (within 1-2 hours)
- Give intravenous fluids and electrolytes to stabilize heart function
- Use medications like magnesium sulfate or isoproterenol to correct arrhythmias
- In severe cases, insert a temporary pacemaker
There is no antidote for loperamide overdose like naloxone for other opioids. Naloxone doesn’t work well here because loperamide doesn’t bind strongly to brain receptors. Even high doses of naloxone have failed to reverse cardiac effects in multiple case studies.
Long-Term Effects and Recovery
People who survive a loperamide overdose often need weeks to recover. Some suffer permanent heart damage. Others develop chronic arrhythmias requiring ongoing medication or devices like implantable defibrillators.
Recovery isn’t just physical. Many who overdose on loperamide are struggling with opioid dependence. They use it to avoid withdrawal symptoms because it’s legal, cheap, and easy to get. But it doesn’t fix the root problem-it just replaces one risk with another. Counseling and medically supervised detox programs are essential for long-term safety.
How to Prevent Loperamide Overdose
Here’s what actually works:
- Never take more than 8 mg in 24 hours unless under direct medical supervision
- Don’t combine it with other drugs that slow your heart-like benzodiazepines, alcohol, or certain antidepressants
- Store it out of reach of teens and people with substance use disorders
- If you’re using it to manage opioid withdrawal, talk to a doctor. There are safer, FDA-approved options like buprenorphine
- Check the label. Some combination products (like those with simethicone) have lower loperamide doses, but people still overdose by taking multiple bottles
Pharmacies in Australia have started limiting sales to 24 tablets per transaction in some states. That’s a small step-but it’s helping. In the U.S., some states now require ID for purchase. These aren’t perfect solutions, but they reduce access for those who want to abuse it.

When to See a Doctor
If you’ve taken more than 16 mg of loperamide in a day-even if you feel fine-get checked out. An ECG takes 5 minutes. It could save your life.
Same goes if you’re using loperamide regularly for more than two days. Diarrhea that lasts longer than 48 hours needs medical evaluation. It could be an infection, IBD, or something else entirely. Relying on loperamide to mask symptoms delays diagnosis and increases overdose risk.
Common Misconceptions
Many believe loperamide is harmless because it’s sold without a prescription. That’s not true. Just because a drug is available over the counter doesn’t mean it’s safe in large amounts. Aspirin can kill you too if you take 50 tablets.
Another myth: “I’ve taken 50 mg before and nothing happened.” That’s luck-not safety. Each time you push the dose higher, you’re playing Russian roulette with your heart. One time, it could be the last.
And no, drinking coffee or taking stimulants won’t “counteract” the overdose. That only adds more strain on your heart.
Can loperamide overdose be fatal?
Yes. Loperamide overdose can cause life-threatening heart rhythm disturbances, including cardiac arrest. Over 100 deaths have been documented worldwide since 2010, mostly from doses exceeding 100 mg. The risk increases dramatically above 50 mg.
Does naloxone reverse loperamide overdose?
Usually not. Naloxone works on brain opioid receptors, but loperamide overdose primarily affects the heart, not the brain. Even high doses of naloxone have failed to reverse cardiac toxicity in clinical cases. Emergency care focuses on heart support, not reversal.
How much loperamide is considered dangerous?
The maximum safe daily dose is 8 mg for over-the-counter use. Doses above 16 mg per day carry increased risk. Over 50 mg is considered a medical emergency. Cases of overdose have been reported with doses as low as 20 mg in people with liver problems or those taking other heart-affecting drugs.
Can you get addicted to loperamide?
Yes. While it doesn’t produce strong euphoria, people who take high doses regularly develop physical dependence. Stopping suddenly can cause withdrawal symptoms like anxiety, sweating, nausea, and muscle aches. Many use it to manage opioid withdrawal, creating a dangerous cycle.
What should I do if someone I know is abusing loperamide?
Talk to them calmly. Don’t shame or panic. Encourage them to speak with a doctor or addiction specialist. Offer to help them find resources like the National Drug and Alcohol Research Centre (NDARC) in Australia or a local opioid treatment program. If they’re in immediate danger, call emergency services.
Final Thoughts
Loperamide isn’t the villain. It’s a useful tool when used correctly. But treating it like candy because it’s on the shelf next to painkillers is deadly. People don’t realize that the same drug that stops diarrhea can also stop their heart.
If you’re using it for more than a few days, you’re not treating the problem-you’re hiding it. And if you’re taking more than the label says, you’re risking your life. No one should die because they thought a little extra pill wouldn’t hurt.





Paige Basford
I used to think Imodium was just for travel stomach bugs, but my cousin took 80mg to get off oxycodone and ended up in the ICU with a pacemaker. No one warned her it could kill you. It’s terrifying how easy it is to get, and how little people know.
My mom’s a nurse, and she says ER docs are seeing this more often now-especially with the opioid crisis pushing people toward anything that ‘works.’
It’s not just about the dose. It’s about the myth that ‘it’s OTC, so it’s safe.’ That’s like saying aspirin can’t overdose you. It can. And it does.
Why isn’t this on every pharmacy shelf? Why isn’t there a warning label bigger than the expiration date?
Ankita Sinha
OMG I had no idea!! I’ve given this to my little cousin when she had food poisoning and felt so guilty thinking I was helping.
But now I’m scared-I didn’t even know the max dose was 8mg! I gave her 4 pills (2mg each) and thought I was being extra careful.
Y’all, let’s spread this info. Share this post. Someone’s life could depend on it.
Also-why is this still sold like candy??
Danielle Mazur
Let me ask you this: who benefits from loperamide being so easily accessible? The pharmaceutical companies? The FDA? Or perhaps the shadow networks pushing opioid substitution therapies under the guise of ‘harm reduction’?
I’ve seen the data-ER visits spiked right after the 2016 warning. Coincidence? Or a controlled rollout to normalize high-dose opioid use under a legal disguise?
And don’t get me started on how naloxone doesn’t work. Why? Because they don’t want you to know it’s not a typical opioid. It’s engineered to bypass detection. It’s a Trojan horse.
They’re testing population-level cardiac vulnerability. And we’re the lab rats.
Margaret Wilson
So let me get this straight… we have a drug that can stop your heart… sold next to Tums… and people are still like ‘eh, I took 50 before and lived’?
Y’all are out here playing Russian roulette with your EKGs and calling it ‘self-care.’
I’m not mad, I’m just disappointed. And also, someone please put this on a billboard next to ‘Don’t Text and Drive.’
💔❤️🩹 #LoperamideIsNotYourBFF
william volcoff
As someone who’s worked in ER for 12 years, I’ve seen 7 loperamide overdoses. All of them were young men trying to self-treat opioid withdrawal. None of them knew the cardiac risks. One guy took 150mg because he ‘read online it was better than methadone.’
Here’s the truth: naloxone doesn’t work because loperamide’s not acting on your brain. It’s wrecking your heart’s electrical grid. You need a pacemaker, not a shot.
And yes, the 8mg limit is real. The 16mg ‘prescription’ limit? That’s for supervised IBS-D patients-not people doing 50mg in one go.
Don’t be the guy who thinks ‘I’m fine’ is a medical diagnosis.
Freddy Lopez
There’s a deeper irony here. We’ve built a society where the most dangerous substances are the ones we’ve made easiest to access. We fear heroin, yet hand out loperamide like candy.
It speaks to our collective denial: if it’s legal, it’s safe. If it’s cheap, it’s harmless.
But safety isn’t defined by regulation-it’s defined by consequence. And loperamide’s consequence is silent, slow, and cardiac.
Perhaps the real question isn’t ‘how do we stop overdoses?’ but ‘why do we keep treating pain with Band-Aids and poison?’
Mary Follero
My brother used to take 20mg daily to ‘calm his nerves’ after his divorce. He didn’t even know he was at risk. I found his empty bottle under the sink and freaked out.
He didn’t want to go to a doctor-he thought it was ‘weak.’ So I took him to a counselor instead. We started talking about grief, not gut issues.
He’s been clean for 14 months now. No loperamide. No opioids. Just therapy, walks, and bad 90s sitcoms.
If you’re using this to cope with anything other than diarrhea… please, reach out. You don’t have to do it alone. I’ve been there. I get it.
And if you’re reading this and thinking ‘I’m fine’… you’re not. Not really.
Arun Mohan
You all sound like amateurs. Loperamide abuse isn’t a ‘public health crisis’-it’s a predictable outcome of deregulated pharmacology and the collapse of clinical oversight.
People think they’re ‘self-medicating’ but they’re just demonstrating their ignorance of pharmacokinetics. The gut-blood barrier saturation threshold is well-documented since the 90s.
And let’s not pretend naloxone should work. It’s not designed for peripheral opioid receptors. That’s basic med school stuff.
If you’re taking more than 8mg without a cardiologist’s approval, you’re not a patient-you’re a walking case study in clinical negligence.
prasad gali
Bottom line: if you’re taking more than 8mg, you’re an idiot. Period.
It’s not ‘addiction.’ It’s stupidity with a side of cardiac arrest.
Stop blaming the system. Start blaming yourself.