Medication Side Effect Checker
Understand Your Medication Risks
Sexual side effects are common with many medications. This tool helps you understand the risk of side effects for your current medications and identify lower-risk alternatives.
Important: This tool is for informational purposes only. Always consult with your healthcare provider before making any changes to your medication.
It’s not rare. It’s not embarrassing. And it’s not something you should just live with. If you’re taking medication for depression, anxiety, bipolar disorder, or even high blood pressure, and your sex life has changed - less desire, trouble getting or keeping an erection, delayed or absent orgasm, or pain during sex - you’re not alone. In fact, between 58% and 70% of people on antidepressants experience some form of sexual side effect. Yet most never talk about it. And that’s the real problem.
Why Nobody Talks About It
Doctors don’t always bring it up. Patients don’t always speak up. A 2023 survey of over 1,200 people on Reddit found that 68% said their prescriber never mentioned sexual side effects before starting medication. Meanwhile, 73% of those who did experience problems waited an average of over four months before telling anyone - mostly because they felt ashamed, thought it was normal, or assumed nothing could be done. But here’s the truth: sexual side effects aren’t just a nuisance. They’re a major reason people stop taking life-saving medications. One national survey showed that 41.7% of men and 15.4% of women quit their psychiatric drugs just because of sexual problems. That’s not just a personal loss - it’s a public health issue. When people stop taking their meds, depression and anxiety come back harder. And that’s worse than any side effect.Which Medications Cause the Most Problems?
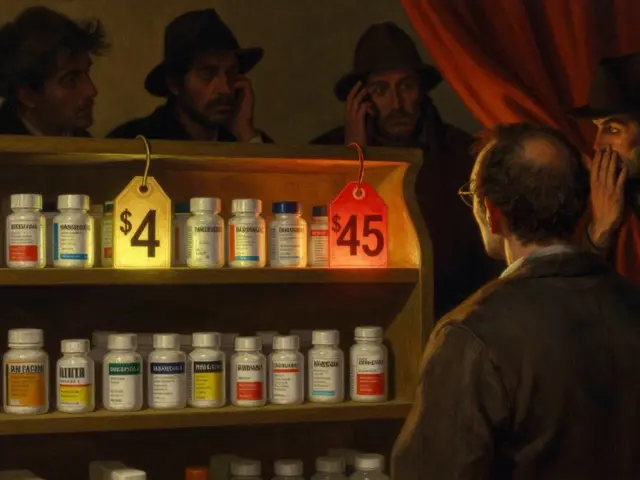
Not all meds are equal when it comes to sexual side effects. SSRIs - like fluoxetine (Prozac), sertraline (Zoloft), and paroxetine (Paxil) - are the biggest offenders. Up to 70% of people on these drugs report issues. That’s because they boost serotonin, which helps mood but can shut down sexual response like a circuit breaker. But there are alternatives. Bupropion (Wellbutrin) and mirtazapine (Remeron) have sexual side effect rates of just 5-10%. That’s a huge difference. For people on antipsychotics, high prolactin levels can cause low libido and erectile problems. Switching to aripiprazole (Abilify) helps 75% of those cases. Even blood pressure meds like beta-blockers and diuretics can cause sexual dysfunction. It’s not just mental health drugs. If you’re on any long-term medication and notice changes in your sex life, it’s worth asking: could this be the drug?What the Side Effects Actually Look Like
Men and women experience this differently, and it’s not just about erections or orgasms. For men:- Loss of sexual desire (62% of cases)
- Trouble getting or keeping an erection (48%)
- Delayed or impossible orgasm (up to 50%)
- Priapism (painful, long-lasting erection - rare, but serious, especially with trazodone)
- Loss of desire (57%)
- Pain during sex (dyspareunia - 38%)
- Difficulty reaching orgasm (anorgasmia - at least 30%)
- Reduced vaginal lubrication
How Counseling Makes a Real Difference
Talking about this isn’t just nice - it’s proven to save lives. When doctors proactively explain the risks before prescribing, patients are far more likely to stick with treatment. One study showed that 82% of patients who received clear counseling about sexual side effects reported higher satisfaction - compared to just 47% who didn’t. Good counseling includes four key steps:- Baseline check: Before starting any med, ask about your current sexual function. Tools like the Arizona Sexual Experience Scale (ASEX) take less than 10 minutes.
- Clear warning: Tell patients exactly what to expect. Say: “About 6 out of 10 people on this drug notice changes in their sex life. That doesn’t mean it’ll happen to you - but if it does, we have solutions.”
- Follow-up schedule: Check in at 2, 4, and 6 weeks. Don’t wait for the patient to bring it up. Most won’t.
- Contingency plan: Have a backup ready. If side effects show up, what’s next? Dose change? Switch? Add-on?
What Works to Fix It
There’s no one-size-fits-all fix, but here’s what actually helps:- Dose reduction: Lowering the dose helps 25-30% of people without losing the antidepressant effect.
- Drug holidays: Skipping the pill for 2-3 days before sex helps 40% of people. But risky if you’re on short-acting drugs like paroxetine - relapse risk is 15%.
- Switching meds: Moving from an SSRI to bupropion or mirtazapine works for 65-70% of patients. One person on HealthUnlocked said: “Switched to Wellbutrin. Sex life improved in two weeks. Been on it 18 months now.”
- Adding sildenafil (Viagra): Helps 55-60% of men with erectile issues. But it doesn’t help with low desire or delayed orgasm. And if you’re not told how to use it properly, it won’t work.
- Couples therapy: If the side effect is straining your relationship, therapy helps 50% of couples. It’s not just about sex - it’s about communication, shame, and reconnecting.
- Sexual scheduling: Planning sex for times when the drug’s effect is lowest (like right after waking up, before the daily dose) helps 35% of people.
The Hidden Barriers
Even when solutions exist, they’re not always offered. Why?- Time: The average doctor visit is 15-20 minutes. Talking about sex feels like a luxury.
- Discomfort: A 2021 survey found 64% of medical residents felt awkward bringing up sexual side effects.
- Protocol gaps: 78% of psychiatric practices have no written plan for handling this.
- Insurance: Only 38% of U.S. commercial plans cover sex therapy.
- LGBTQ+ blind spots: A 2022 study showed LGBTQ+ patients are 28% less likely to have these conversations with providers.
What’s New and What’s Coming
The field is evolving. In 2023, the American Psychiatric Association updated its guidelines to include a full section on sexual side effect management - with algorithms for different meds. That’s a big deal. Digital tools are catching up too. The MoodFX app, used by over 127,000 people, tracks mood and sexual function together. It helps patients notice patterns and talk to their doctors with data, not just feelings. A new drug is in phase 3 trials (NCT04891234) - a 5-HT2C receptor antagonist designed to reverse SSRI-induced sexual dysfunction without hurting the antidepressant effect. Results expected in early 2024. Experts predict that within five years, checking for sexual side effects will be as routine as checking weight or blood sugar. And by 2030, medication discontinuation due to these side effects could drop by half - if we keep pushing for better care.What You Can Do Right Now
If you’re on medication and having sexual side effects:- Don’t stop cold turkey. That can trigger withdrawal or relapse.
- Write down your symptoms. When did they start? What changed? How often?
- Bring it up at your next appointment. Say: “I’ve noticed changes in my sex life since starting [med name]. Is this related? What can we do?”
- Ask about alternatives. “Are there other meds with fewer sexual side effects?”
- Ask about timing. “Could adjusting when I take the pill help?”
- Ask for a referral. If your doctor doesn’t know what to do, ask for a sexual health counselor or pharmacist trained in this area.
Final Thought
Sex isn’t a bonus feature of life - it’s part of being human. Medications save lives. But they shouldn’t cost you your intimacy, your confidence, or your connection with others. The fact that this issue is so widespread - and so treatable - means we’re not powerless. We just need to talk about it.Can antidepressants cause permanent sexual dysfunction?
In rare cases, some people report persistent sexual side effects after stopping antidepressants - a condition sometimes called Post-SSRI Sexual Dysfunction (PSSD). But this is not common, and research is still ongoing. Most people see improvement within weeks to months after switching or stopping the medication. If symptoms last more than 3-6 months after discontinuation, consult a specialist in sexual medicine.
Is it safe to take Viagra with antidepressants?
Yes, for most people, sildenafil (Viagra) and similar drugs are safe to use with antidepressants. But they shouldn’t be taken with nitrates (used for chest pain) or if you have certain heart conditions. Always check with your doctor or pharmacist. Also, Viagra helps with erections - not low desire or delayed orgasm. It’s not a magic fix for all sexual side effects.
Why don’t doctors talk about this more?
Many doctors feel uncomfortable discussing sex, worry about time limits, or assume patients won’t bring it up. Some still believe it’s a minor issue compared to depression. But research shows that not talking about it leads to higher dropout rates. Guidelines now recommend routine screening - but implementation is still uneven.
Can therapy help with sexual side effects?
Yes - especially couples therapy or sex therapy. When medication changes aren’t enough, or when the side effect has damaged your relationship, talking with a trained therapist can rebuild intimacy, reduce shame, and improve communication. Studies show 50% improvement in outcomes when therapy is added to medical management.
Are there any natural remedies that help?
There’s no strong evidence that supplements like ginseng, maca, or L-arginine reliably fix medication-induced sexual dysfunction. Some people report benefits, but results are inconsistent. Don’t replace medical advice with unproven remedies. If you’re considering supplements, talk to your doctor first - some can interact with your meds.
What should I ask my pharmacist?
Ask: “What are the sexual side effects of this drug?” “Are there alternatives with fewer risks?” “Can I adjust the timing of my dose to help?” Pharmacists are trained to spot these issues and can offer practical tips - like taking the pill in the morning to reduce nighttime effects, or suggesting a drug holiday schedule. Many now offer sexual health counseling as part of their services.
Is this only a problem for people on antidepressants?
No. Many other medications can cause sexual side effects - including blood pressure drugs (beta-blockers, diuretics), antipsychotics, hormonal treatments, and even some seizure medications. If you’re on any long-term prescription and notice changes in your sex life, it’s worth reviewing all your meds with your provider.
How long does it take for sexual function to return after switching meds?
Most people notice improvement within 2-6 weeks after switching to a medication with lower sexual side effect risk, like bupropion or mirtazapine. For some, it takes longer - up to 8-12 weeks - especially if the body needs time to reset. Patience and follow-up matter. Don’t give up if you don’t see change right away.




Mimi Bos
i literally thought i was the only one. took zoloft for 3 years and just stopped having any interest in sex... thought it was me. turned out it was the meds. so glad this post exists.
ANA MARIE VALENZUELA
people need to stop blaming drugs and take responsibility. if you can't get it up after a pill, maybe you're just lazy or emotionally blocked. this whole 'sexual side effect' thing is just an excuse to avoid intimacy.
Bradly Draper
i had this happen with citalopram. felt like a robot. no drive, no joy. switched to wellbutrin and my wife said i was 'back'. best decision i ever made. just talk to your doc. they can help.
Gran Badshah
in india we dont even talk about this. my cousin stopped his antidepressants because he was 'ashamed' to tell his wife. now he's worse off. this is a global issue. silence kills.
Ellen-Cathryn Nash
i'm not saying you should suffer in silence, but maybe if you didn't have so much porn in your life, you wouldn't be so sensitive to these side effects. sex isn't supposed to be effortless. learn to connect without the chemical crutch.
Samantha Hobbs
my dr never mentioned it. i just thought i was broken. then i found a reddit thread and cried for an hour. why is this so hard to talk about? it's not a secret. it's medicine.
sonam gupta
india has better solutions than pills. yoga meditation diet. why do you need western drugs anyway? your mind is weak. fix your soul not your serotonin
Julius Hader
just wanted to say thank you for writing this. i've been on sertraline for 5 years. switched to mirtazapine last month. my libido came back slowly but it's back. and yeah, i cried when i realized i could feel again. you're not alone. 💙