Amantadine Adjunct Therapy Quiz
Amantadine is a synthetic adamantane derivative originally approved as an antiviral and later repurposed for Parkinson's disease. It works by modulating dopamine release and blocking NMDA‑type glutamate receptors, which gives it a unique pharmacological profile that researchers are now testing in schizophrenia as an adjunctive agent.
Why Look Beyond Traditional Antipsychotics?
Standard antipsychotic medication is a drug class that primarily targets dopamine D2 receptors to reduce positive symptoms such as hallucinations and delusions. While effective for many, up to 30% of patients continue to suffer from cognitive symptoms (impaired attention, memory, executive function) and negative symptoms (apathy, social withdrawal). These domains are less responsive to dopamine blockade and often drive functional disability.
Amantadine’s Dual‑Action Mechanism
Two neurochemical pathways give amantadine its edge:
- Dopamine modulation: It increases synaptic dopamine by stimulating release and inhibiting reuptake, which may counteract the dopamine deficit linked to negative and cognitive deficits.
- NMDA receptor antagonism: By dampening excessive glutamate activity, amantadine may restore balance in the glutamatergic system that is thought to underlie some psychotic features.
In semantic terms, Amantadine[modulates]dopamine D2 receptors and Amantadine[blocks]NMDA receptors. These actions create a brief “dopamine‑glutamate” correction that standard antipsychotics don’t provide.
Schizophrenia Symptom Landscape
Schizophrenia is a chronic mental disorder characterized by positive, negative, and cognitive symptom clusters. Positive symptoms (hallucinations, delusions) respond well to dopamine D2 blockade, whereas negative (flattened affect, anhedonia) and cognitive deficits are more stubborn.
Recent meta‑analyses show that cognitive impairment predicts long‑term functional outcome more strongly than positive symptom severity. This is why adjunctive therapies that target cognition have become a research priority.
Evidence from Clinical Studies
Several small‑scale trials have explored amantadine as an add‑on to conventional antipsychotics:
- A 12‑week double‑blind study in 48 patients receiving haloperidol reported a 15% improvement in the PANSS (Positive and Negative Syndrome Scale) negative subscale when amantadine 200mg/day was added.
- A crossover trial involving 30 clozapine‑treated patients showed a modest gain in working‑memory scores (Mean increase=0.8SD) after 8 weeks of amantadine 150mg/day.
- Open‑label reports from psychiatric clinics in Europe suggest reduced extrapyramidal side‑effects when amantadine is paired with high‑potency typical antipsychotics, likely because of its dopamine‑releasing properties.
While sample sizes remain modest, the pattern is consistent: amantadine appears to boost negative and cognitive outcomes without worsening psychosis, provided the baseline antipsychotic regimen is stable.
How Does Amantadine Stack Up Against Standard Adjuncts?
| Feature | Amantadine | Clozapine | Haloperidol |
|---|---|---|---|
| Primary Action | Boosts dopamine release; NMDA antagonism | Broad serotonin‑dopamine antagonism | Potent dopamine D2 antagonism |
| Effect on Negative Symptoms | Modest improvement (≈10‑15%) | Significant improvement (≈20‑30%) | Minimal |
| Effect on Cognitive Scores | Small gains in working memory | Variable; some studies show no change | None |
| Common Side‑Effects | Insomnia, mild constipation | Agranulocytosis (requires blood monitoring) | Extrapyramidal symptoms, tardive dyskinesia |
| Monitoring Needs | Routine labs only | Weekly CBC | Movement‑scale assessments |
The table highlights that amantadine offers a milder side‑effect profile than clozapine and haloperidol, making it attractive for patients who cannot tolerate aggressive dopamine blockade.
Practical Considerations for Clinicians
When adding amantadine to a stable antipsychotic regimen, follow these guidelines:
- Start low: 100mg once daily, titrating to 200mg as tolerated.
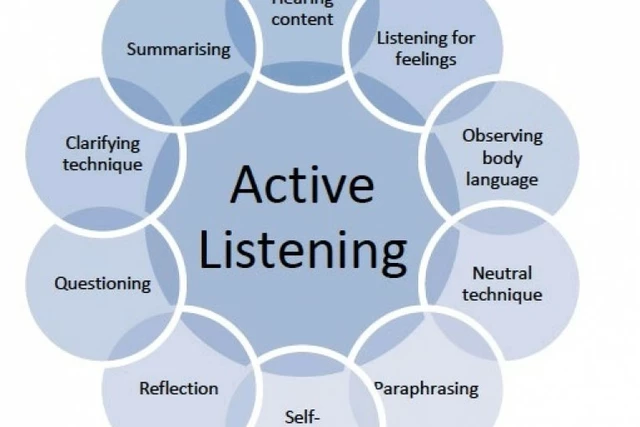
- Monitor cognition: Use brief tools like the Montreal Cognitive Assessment (MoCA) every 4weeks.
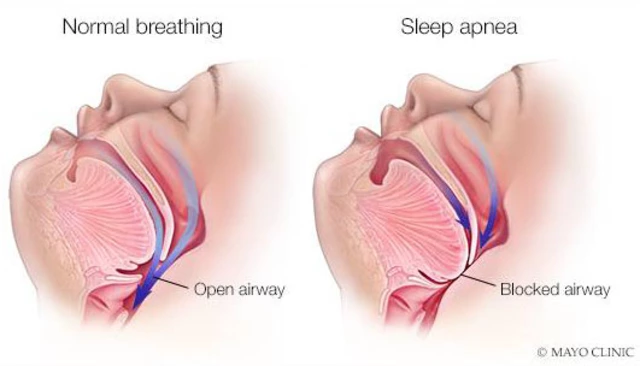
- Watch for insomnia: If sleep disruption emerges, split the dose or reduce evening intake.
- Assess for drug interactions: Amantadine is cleared renally; dose‑adjust in CrCl<50ml/min.
- Document symptom changes: Record PANSS negative and cognitive subscale scores before and after initiation.
Because amantadine does not significantly alter CYP450 enzymes, it rarely interferes with metabolized antipsychotics, but clinicians should still review the full medication list.
Future Research Directions
Large‑scale, multi‑center phase‑III trials are slated for 2026, focusing on:
- Long‑term impact on functional outcomes (employment, social integration).
- Biomarker‑guided subgroups - patients with pronounced glutamatergic dysregulation may benefit most.
- Combination strategies - pairing amantadine with cognitive remediation therapy.
Should these studies confirm early signals, guidelines may soon list amantadine as a LevelIII adjunct for treatment‑resistant negative symptoms.
Key Takeaways
Amantadine brings a rare “dopamine‑glutamate” dual mechanism that can fill gaps left by conventional antipsychotics. While evidence remains preliminary, the drug’s tolerable side‑effect profile and modest cognitive gains make it a candidate worth watching, especially for patients stuck on clozapine or high‑potency typical agents.
Frequently Asked Questions
Can amantadine replace antipsychotics in schizophrenia?
No. Amantadine is used only as an add‑on to a stable antipsychotic regimen. It lacks strong dopamine D2 blockade, so it cannot control positive symptoms on its own.
What dose of amantadine is typically used for schizophrenia?
Clinicians start with 100mg once daily and may increase to 200mg/day, divided if needed, based on tolerance and response.
Are there any serious risks associated with amantadine?
Serious adverse events are rare, but high doses can cause confusion, hallucinations, or orthostatic hypotension, especially in older adults with renal impairment.
How does amantadine affect extrapyramidal side‑effects?
Because it stimulates dopamine release, amantadine can lessen drug‑induced rigidity and akathisia when paired with typical antipsychotics.
Is amantadine covered by insurance for psychiatric use?
Coverage varies. Some insurers require off‑label justification and prior authorization, while others treat it like an antiviral and reimburse accordingly.
What monitoring labs are needed?
Baseline renal function (creatinine clearance) and periodic CBCs are advised, especially if the patient is on other myelosuppressive agents.
Can amantadine be used in younger patients?
Safety data in adolescents are limited. Most studies involve adults over 18, so clinicians should exercise caution and consider specialist consultation.





Emily Moody
The pharmacodynamic profile of amantadine reads like a manifesto for a new neuro‑psychiatric frontier; its dopamine‑release boost and NMDA blockade form a dual‑pronged assault on entrenched deficits, and we cannot afford complacency in the face of such a promising candidate.
Prateek Kohli
While the data are still emerging, the modest gains in negative symptoms and working‑memory scores suggest that amantadine could serve as a bridge between antipsychotic stabilization and functional recovery 😊. Clinicians should keep an eye on tolerability, especially insomnia, which appears to be the most common side‑effect.
Noah Seidman
One might argue that augmenting a dopamine antagonist with a dopamine‑releasing agent treads on philosophical ground, but the reality is that schizophrenia’s pathology is not a monolith; balancing dopaminergic tone without tipping into psychosis is a delicate ethical dance.
Anastasia Petryankina
Oh great, another pill to shove into the already over‑medicated schizophrenia cocktail.
Tim Ferguson
The simplicity of starting amantadine at 100 mg daily and titrating to 200 mg mirrors a pragmatic approach: give the brain a gentle nudge rather than a sledgehammer. Monitoring should focus on cognitive assessments rather than exhaustive blood panels.
Noah Cokelaere
It’s interesting that amantadine may reduce extrapyramidal side‑effects when paired with high‑potency typical antipsychotics, essentially acting as a neuro‑protective buddy that keeps the dopamine circuitry from going haywire.
Ashley Helton
Seriously, if you’re already juggling haloperidol and clozapine, adding a low‑risk agent like amantadine could be the “just‑right” tweak that nudges patients toward better daily functioning.
Brian Jones
From a coaching perspective, think of amantadine as a supportive teammate that helps the primary antipsychotic stay on point while offering extra energy for those cognitive workouts you’ve been missing.
Carlise Pretorius
i think its kinda cool but watch out for insomnia ya know its not a miracle drug but it helps with some of those negative vibes.
Johnson Elijah
Hey folks 🌍! Amantadine’s dual action is like a double‑espresso for the brain: a boost in dopamine release and a calming NMDA block, which might just give patients the extra pep they need to tackle daily tasks. Keep an eye on sleep, though-too much buzz can keep you up.
Roxanne Lemire
the evidence is still thin, but the few trials show a consistent trend toward improved negative symptoms without a rise in positive scores, which is noteworthy for a adjunctive therapy.
Alex Mitchell
Let’s remember that any add‑on should be introduced slowly, respecting each patient’s baseline stability and personal preferences 😊. Routine labs are sufficient, but a quick check on renal function is prudent given amantadine’s clearance.
Narayan Iyer
From a neuropharmacological standpoint, amantadine’s capacity to modulate synaptic dopamine via vesicular release mechanisms, coupled with its non‑competitive antagonism at the glycine site of NMDA receptors, positions it as a candidate for synergistic augmentation in treatment‑resistant psychosis cohorts.
Amanda Jennings
Totally echo that vibe-when you stack amantadine on a stable antipsychotic regimen, you’re essentially fine‑tuning the dopaminergic‑glutamatergic balance without overhauling the whole therapeutic architecture.
alex cristobal roque
Amantadine, originally celebrated for its antiviral properties, has traversed a remarkable pharmacological journey into the realm of neuropsychiatry.
Its mechanism of increasing extracellular dopamine while simultaneously dampening excessive NMDA‑mediated glutamatergic transmission creates a unique neurochemical milieu.
This dual action directly addresses the dopamine deficit implicated in negative and cognitive symptom domains of schizophrenia.
Moreover, by tempering glutamate excitotoxicity, amantadine may mitigate some of the downstream neuroinflammatory cascades that exacerbate psychosis.
Clinical trials, albeit modest in size, consistently report a 10‑15 % improvement in PANSS negative subscale scores when amantadine is added to conventional antipsychotics.
Working‑memory assessments, such as the MoCA, have shown incremental gains that correlate with patients’ reported functional outcomes.
Importantly, the side‑effect profile remains relatively benign, with insomnia and mild constipation being the most frequently noted adverse events.
Unlike clozapine, amantadine does not necessitate weekly CBC monitoring, which reduces the logistical burden on both clinicians and patients.
Renal clearance considerations are straightforward; dose adjustments are only required in cases of severe renal impairment.
From a pharmacoeconomic perspective, the generic availability of amantadine keeps costs low, making it an accessible option for resource‑limited settings.
When integrating amantadine into an existing regimen, a gradual titration from 100 mg to 200 mg daily allows clinicians to gauge tolerability while minimizing the risk of dose‑related insomnia.
Ongoing assessment using brief cognitive batteries every four weeks can help track the incremental benefits over time.
Patients often report a subjective sense of increased motivation and mental clarity, which may translate into better adherence to psychosocial interventions.
While larger, multicenter trials are still needed to solidify efficacy signals, the current evidence base justifies cautious optimism among prescribers.
In sum, amantadine stands out as a modest yet promising adjunct that bridges the gap between dopamine blockade and glutamate modulation, offering a nuanced tool in the clinician’s armamentarium.
Bridget Dunning
Esteemed colleagues, the integration of amantadine into adjunctive schizophrenia treatment warrants rigorous scrutiny; its pharmacodynamic profile, while intriguing, must be evaluated through the lens of evidence‑based medicine and longitudinal safety data.
Shweta Dandekar
It is imperative, therefore, that clinicians adhere to protocol, conduct regular monitoring, and document outcomes meticulously; otherwise, the therapeutic potential of amantadine may remain underutilized, and patient safety could be compromised.
Gary Smith
We must champion American ingenuity in psychiatric pharmacotherapy, embracing amantadine as a bold step forward-yet we cannot ignore the necessity for robust clinical trials, standardized dosing guidelines, and vigilant post‑marketing surveillance.