Why Your Blood Sugar Spikes Every Morning
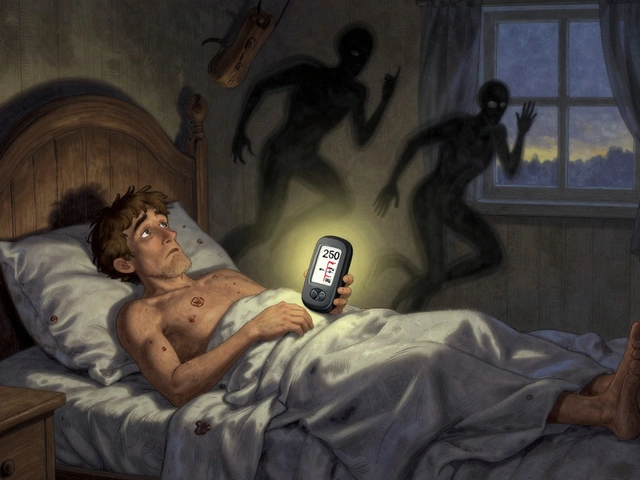
You wake up, check your meter, and your blood sugar is sky-high-180, 220, even 250 mg/dL. You didn’t eat anything late. You took your insulin. You didn’t snack. So why is it happening? If this is your daily routine, you’re not alone. About half of all people with Type 1 and Type 2 diabetes deal with the same thing: the dawn phenomenon.
This isn’t about poor discipline. It’s not because you ate too many carbs the night before. It’s your body’s natural biology kicking in at the wrong time. Between 3 a.m. and 8 a.m., your body releases hormones like cortisol, growth hormone, and glucagon to prepare you for the day. These hormones tell your liver to pump out glucose-your body’s way of giving you energy to wake up. In someone without diabetes, the pancreas responds by releasing insulin to keep things balanced. But if you have diabetes, your body either can’t make enough insulin or can’t use it well. That’s when your blood sugar rises instead of staying steady.
Dawn Phenomenon vs. Somogyi Effect: Don’t Mix Them Up
Many people assume high morning blood sugar means they didn’t take enough insulin the night before. But there’s another possibility: the Somogyi effect. It sounds similar, but it’s completely different.
The Somogyi effect happens when your blood sugar drops too low overnight-below 70 mg/dL. Your body panics, releases stress hormones, and your liver dumps glucose to rescue you. The result? A rebound high in the morning. But here’s the key difference: with the Somogyi effect, your blood sugar dips first. With the dawn phenomenon, it just climbs steadily from 3 a.m. onward, with no low point in between.
How do you tell them apart? Check your blood sugar at 3 a.m. for three nights in a row. If it’s below 70 mg/dL, it’s likely Somogyi. If it’s above 100 mg/dL and climbing, it’s the dawn phenomenon. Continuous glucose monitors (CGMs) make this easy-they show you the trend line. A steady upward arrow from 3 a.m. to 7 a.m. is the classic sign.
What Happens in Your Body During the Dawn Phenomenon
It’s not random. Your body follows a clock. Around 3 a.m., cortisol levels jump by 50-100%. Growth hormone spikes 300-500%. Glucagon tells your liver to break down stored sugar (glycogen) and make new sugar from scratch (gluconeogenesis). Your liver starts pumping out 20-30% more glucose than usual. In a person without diabetes, insulin rises by 40-50% to match it. But if you have Type 1 diabetes, your body doesn’t make insulin at all. In Type 2, your cells ignore insulin, and your pancreas is worn out.
The result? Your blood sugar climbs 10-15 mg/dL per hour during those early hours. By 7 a.m., you’re already at 180-250 mg/dL. Studies show this isn’t rare. Nearly 50% of adults with Type 1 and Type 2 diabetes experience it regularly. Even kids and seniors are affected. One study found 48.7% of children with Type 1 diabetes had morning spikes. It doesn’t care about your age-it just follows biology.

Why It Matters: More Than Just a Bad Morning
High morning glucose isn’t just annoying. It’s dangerous. If your blood sugar stays high every day, your HbA1c rises. Each 1% increase in HbA1c raises your risk of complications-like nerve damage, kidney problems, and vision loss-by 21%. A study showed that uncontrolled dawn phenomenon can bump your HbA1c up by 0.5 to 1.2 points. That’s the difference between 7.2% and 8.4%. One point might seem small, but it’s the difference between good control and real risk.
And it’s not just long-term. If your morning sugar hits 250 mg/dL or higher, you could be heading toward diabetic ketoacidosis (DKA), especially if you have Type 1 diabetes. One study found that people with uncontrolled dawn phenomenon had 3.2 DKA episodes per 100 patient-years. That’s not something to ignore.
Plus, it messes with your mental health. People report anxiety, frustration, and even shame. They feel like they’re failing-even when they’re doing everything right. One survey found 57% of people said the dawn phenomenon hurt their quality of life. They dreaded checking their meter. They felt like their whole day was ruined before it even started.
How to Manage the Dawn Phenomenon
There’s no magic fix, but there are proven ways to bring it under control. The key is to match your treatment to your body’s rhythm.
For People Using Insulin Pumps or CGMs
If you’re on an insulin pump, adjusting your basal rate is the most effective move. Most people need to increase their overnight insulin by 20-30% between 3 a.m. and 7 a.m. Studies show this cuts morning highs by 45-60 mg/dL. Automated insulin delivery systems like Control-IQ or t:slim X2 with Control-IQ 3.0 are even better-they start adjusting insulin as early as 2 a.m. based on trends. One trial showed a 63% drop in morning spikes.
For People on Multiple Daily Injections
Switching your long-acting insulin to bedtime can help. Some people get better results with glargine or degludec taken at night instead of in the morning. Your doctor might also suggest adding a small dose of rapid-acting insulin before bed-but only if your overnight sugar isn’t already low. Never guess. Use your CGM data.
Diet and Timing
What you eat at dinner matters. A study from Joslin Diabetes Center found that cutting evening carbs to under 45 grams reduced morning spikes by 27%. Avoid pasta, rice, bread, or sugary desserts after 7 p.m. Instead, focus on protein and healthy fats: grilled chicken, fish, eggs, avocado, nuts, or a small portion of cheese.
Some people benefit from a bedtime snack-but not just any snack. A small portion with 15g protein and 5g fat (like a hard-boiled egg with a tablespoon of peanut butter) can help stabilize blood sugar overnight. Avoid carbs in the snack. Sugar will make it worse.
Sleep and Stress
Bad sleep makes the dawn phenomenon worse. If you’re getting less than 7 hours or your sleep is interrupted, your morning sugar can rise 15-20 mg/dL. Try to keep a regular sleep schedule. Avoid screens an hour before bed. If you’re stressed, cortisol rises-and so does your blood sugar. Meditation, deep breathing, or even a warm bath before bed can help.
What Doesn’t Work
Don’t just increase your insulin dose at night without checking your 3 a.m. levels. You might cause a dangerous low. One study found that 34% of people who adjusted insulin based only on morning highs ended up with more nighttime lows. That’s riskier than the high itself.
Also, don’t blame yourself. The dawn phenomenon isn’t your fault. It’s not laziness, poor diet, or lack of willpower. It’s your biology. Many people have been told their morning spikes are because they “ate too much last night.” That’s not true. It’s the hormones. You’re not failing-you’re fighting a natural process that your body can’t regulate on its own.
When to See Your Doctor
If you’ve been checking your blood sugar at 3 a.m. for three nights and it’s consistently rising, talk to your diabetes care team. Bring your CGM data. Show them the trend. Ask about:
- Adjusting your basal insulin timing or dose
- Switching to a different long-acting insulin
- Using an automated insulin delivery system
- Adding a GLP-1 agonist like semaglutide or liraglutide at night
Some newer medications, like once-weekly insulin icodec, are showing better morning control in trials. Your doctor might not know about them yet-so bring the info. Be your own advocate.
Tools That Help
You don’t need to guess anymore. These tools make managing the dawn phenomenon possible:
- Continuous Glucose Monitors (CGMs): Dexcom G7, Abbott FreeStyle Libre 3, Medtronic Guardian 4. These show real-time trends and alerts. 85% of endocrinologists say CGM is essential for dawn phenomenon.
- Insulin pumps with predictive tech: Tandem t:slim X2 with Control-IQ 3.0, Insulet Omnipod 5. They adjust insulin before the spike hits.
- Diabetes apps: Log your meals, sleep, and trends. Look for patterns over weeks, not just one bad morning.
The Future Is Personalized
Scientists are already finding genetic markers linked to stronger dawn phenomenon responses. In the next 5-7 years, blood tests might tell you if you’re genetically prone to this. That means treatments could be tailored to your biology-not just trial and error.
Right now, the best thing you can do is get data. Use your CGM. Check at 3 a.m. if you can. Track your sleep. Adjust your dinner. Talk to your doctor. You don’t have to live with high mornings forever. The dawn phenomenon is real-but it’s not unbeatable.




Eddie Bennett
I used to think I was failing until I learned about the dawn phenomenon. Now I know it's not my fault. My CGM shows that spike every day like clockwork. I just adjust my basal a bit and call it a win.
Feels good to stop blaming myself.
Ben Greening
The distinction between the dawn phenomenon and the Somogyi effect is critical and often misunderstood. Clinical guidelines consistently recommend nocturnal glucose monitoring to differentiate the two, as mismanagement can lead to iatrogenic hypoglycemia. Data-driven adjustments are paramount.
David Palmer
lol so my body’s just being a jerk at 3am? thanks for the science lecture but i’m just gonna eat a donut and sleep through it 😴
Paul Dixon
This is the most helpful thing I’ve read all year. I’ve been so frustrated with my morning numbers, but now I get it. I started doing that egg + peanut butter snack and my 7am readings dropped 40 points. Small changes, big difference.
Thanks for writing this.
Vivian Amadi
You’re all just making excuses. I’ve been diabetic for 15 years and I never had this problem. You’re just lazy and don’t check your carbs. Stop blaming your hormones and start blaming yourself.
Jimmy Kärnfeldt
It’s wild how biology just does its thing regardless of how hard we try. I used to feel like a failure every morning. Now I see it as my body trying to protect me-even if it’s overdoing it.
Kinda beautiful in a weird, frustrating way. We’re not broken. We’re just working with a system that wasn’t built for insulin resistance. We’re adapting. That’s strength.
john damon
I just got my libre 3 and holy 🤯 the graph at 4am looks like a rocket 🚀. I’m gonna try that basal tweak. Also, anyone else sleep like a rock and wake up feeling like a zombie? 😴💔
matthew dendle
dawn phenomenon my ass. you just ate pizza at midnight. everyone knows that. stop making up science to feel better about your choices. you dont need a cgm you need discipline
Monica Evan
I’m from Nigeria and we don’t have CGMs here but I track with fingersticks and I swear this dawn thing is real. My cousin in Lagos has it too. I started giving him a tiny bit of peanut butter before bed and his numbers dropped like magic.
It’s not just Westerners. This is global. Your body doesn’t care where you live.
Jim Irish
The article correctly identifies the dawn phenomenon as a physiological, not behavioral, issue. Management requires individualized insulin timing and data validation. Self-blame is counterproductive and undermines patient autonomy.