When you're pregnant or breastfeeding, even a mild headache can feel like a crisis. You’re not just thinking about yourself anymore-you’re thinking about your baby. That’s why so many women with migraines hold off on treatment, hoping it’ll pass. But untreated migraines aren’t harmless. They raise your risk of preterm birth, preeclampsia, and low birth weight. They also wreck your sleep, spike your stress hormones, and make postpartum depression more likely. The truth? Migraine treatment during pregnancy and breastfeeding isn’t about avoiding all meds-it’s about choosing the right ones.
Why Migraines Change During Pregnancy
Many women notice their migraines improve during pregnancy, especially in the second and third trimesters. That’s because estrogen levels stay high and steady. But for others, migraines get worse-especially in the first trimester when hormones are swinging wildly. After delivery, estrogen drops fast. That’s when a lot of new moms get hit with their worst migraines yet. It’s not just bad luck-it’s biology.Non-Drug Treatments: Your First Line of Defense
Before you reach for a pill, try these proven, zero-risk methods. They work better than most people think.- Sleep 7-9 hours a night. Even one night of poor sleep can trigger a migraine. Use blackout curtains, white noise, and a consistent bedtime-even if your baby is awake.
- Move daily. Thirty minutes of walking, swimming, or prenatal yoga five days a week cuts migraine frequency by up to 40%. No need to push hard-just keep moving.
- Stay hydrated. Drink 2-3 liters of water daily. Dehydration is one of the top migraine triggers. Carry a bottle with you and sip constantly.
- Eat small meals every 3-4 hours. Skipping meals drops blood sugar and sparks migraines. Keep nuts, fruit, and cheese on hand.
- Try acupuncture. A 2021 study of 120 pregnant women found that weekly acupuncture sessions reduced migraine frequency by 50% in nearly 7 out of 10 women.
- Use massage. Two 30-minute massages a week during the second and third trimesters lowered migraine frequency by 35% in one 2020 study.
- Try biofeedback. This technique teaches you to control stress responses. With 3-5 sessions a week, it reduces migraine days by 40-60%.
- Consider Cefaly. This FDA-cleared headband stimulates nerves through the skin. In studies, 68% of users saw at least half fewer migraines. It’s safe during pregnancy and breastfeeding.
Acute Treatment: What You Can Take When a Migraine Hits
When non-drug methods aren’t enough, you need relief. Here’s what’s safe.Acetaminophen (Tylenol)
This is the gold standard. No known birth defects. No risk to breastfeeding babies. The maximum daily dose is 3,000 mg-so stick to 650 mg every 6 hours as needed. It’s the go-to for most OB-GYNs.Ibuprofen (Advil, Motrin)
Safe in the first and second trimesters. Avoid after 30 weeks-it can affect fetal circulation. During breastfeeding, it’s one of the safest NSAIDs. Less than 1% of the dose passes into breast milk. The Relative Infant Dose (RID) is just 0.65%.Sumatriptan (Imitrex)
The most studied triptan in pregnancy. No increase in birth defects compared to the normal 3% baseline. But it does carry a small risk of longer labor and more blood loss during delivery-so use it only when needed. During breastfeeding, only 3% of the dose enters milk. Experts say it’s safe if you take it right after nursing and wait 3-4 hours before the next feed.Rizatriptan (Maxalt)
Less data than sumatriptan, but early studies show even lower transfer into breast milk-only 1.2%. A good option if sumatriptan doesn’t work for you.Other Options
- Diphenhydramine (Benadryl): RID 3.5%. Safe for occasional use, but can make your baby drowsy.
- Metoclopramide (Reglan): RID 0.5%. Helps nausea and can ease migraine pain.
- Ondansetron (Zofran): RID 0.7%. Safe for nausea with migraine.
What to Avoid Completely
Some meds are dangerous at any stage.- Ergots (DHE, Cafergot): Can cause severe uterine contractions and fetal harm. Never use.
- Valproic acid (Depakote): Raises risk of neural tube defects by 11%. Absolutely contraindicated.
- Feverfew: Herbal remedy linked to 38% higher risk of miscarriage. Skip it.
- Aspirin (high dose): Can cause bleeding complications in pregnancy and infants.

Preventive Treatments: Stopping Migraines Before They Start
If you’re getting migraines more than twice a week, prevention matters.Magnesium
Take 400-600 mg daily. A 2021 Cochrane Review of 550 pregnant women found it reduced migraine frequency by 35%. No side effects. It’s safe, cheap, and effective.Propranolol
A beta-blocker used for prevention. It works-but it’s linked to slower fetal growth and smaller placentas. Only use if migraines are severe and other options fail. Monitor fetal growth closely.Cyclobenzaprine
A muscle relaxant. Limited data, but no major birth defects reported in 127 cases. Might help if tension is part of your migraine trigger.Memantine
An Alzheimer’s drug repurposed for migraine. Theoretical risk is low because it binds tightly to proteins and doesn’t cross the placenta easily. But evidence is still thin.Migraine Prevention While Breastfeeding
Your options open up a bit after birth. The key is choosing meds with low Relative Infant Dose (RID)-below 10% is ideal.- Propranolol: RID 0.3-0.5%. Safe, but watch your baby for drowsiness or slow heart rate. Rare, but possible.
- Verapamil: RID just 0.15-0.2%. One of the safest calcium channel blockers for nursing moms.
- Amitriptyline: RID 1.9-2.8%. An old-school antidepressant that helps with chronic pain. Well-studied in breastfeeding.
- Sertraline (Zoloft): RID 0.4-2.2%. Also helps with postpartum mood. Often preferred over other SSRIs.
- Riboflavin (B2): 400 mg daily. Safe, natural, and shows promise in small studies. No known side effects for babies.
- Magnesium sulfate: L1 classification-safest possible. Use if you’re still supplementing.
Timing Matters: How to Take Meds Without Hurting Your Baby
If you’re breastfeeding and taking a migraine med, timing is everything. Take your dose right after you nurse. Then wait 3-4 hours before the next feed. That gives your body time to clear most of the drug. This simple trick cuts infant exposure by up to 80%.What Real Moms Are Doing
A 2023 survey of 1,247 breastfeeding mothers found:- 78% managed migraines with acetaminophen and ibuprofen alone-no issues.
- 15% used triptans. Of those, 92% saw no changes in their babies.
- 63% used non-drug methods like yoga, massage, or Cefaly-and said they worked.
- Those who tried ergots or valproic acid mostly stopped because of scary side effects.

The Bigger Picture: Why Treatment Is Safer Than You Think
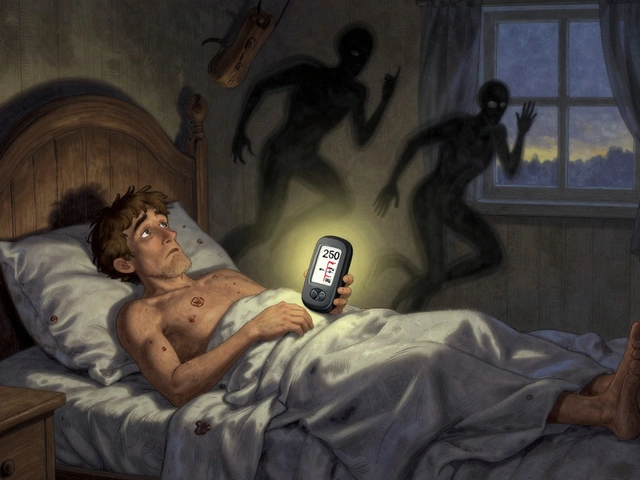
Many women fear meds more than migraines. But untreated migraines are worse. High stress raises cortisol by 45-60%. Poor sleep cuts REM sleep by 30-40%. That directly affects your baby’s development and your mental health. The American Headache Society says: “Properly managed migraine poses less risk than uncontrolled migraine.” That’s not just a slogan-it’s backed by data.When to See a Specialist
Only 42% of OB-GYNs and 68% of neurologists feel confident managing migraines in pregnancy. If your doctor says, “Just tough it out,” or “Don’t take anything,” ask for a referral. Look for:- A headache specialist with experience in pregnancy
- An obstetrician who works with a lactation consultant
- A pharmacist trained in medications and breastfeeding
What’s New in 2025
Rimegepant (Nurtec ODT), approved by the FDA in 2023, is now an option for acute and preventive treatment during breastfeeding (L2 classification). It’s not yet well-studied in pregnancy, so use with caution. New research on CGRP blockers (like erenumab) is coming. Early data looks promising for breastfeeding, but pregnancy data is still missing. Watch for updated guidelines in 2024.Your Action Plan
1. Start with lifestyle. Sleep, water, food, movement-fix these first.Migraines don’t have to rule your pregnancy or your motherhood. With the right tools, you can protect your health-and your baby’s-without fear.






Raja P
Just wanted to say thanks for this. I had my first migraine during my second trimester and was terrified to take anything. Ended up using acetaminophen and Cefaly-worked like a charm. No guilt, no panic. Just peace.
Also, hydration was a game-changer. I started carrying a 1L bottle everywhere. Sipping all day, not chugging. My headaches dropped from 5x/week to once every 10 days. Simple stuff, but nobody tells you that.
Austin LeBlanc
Ugh, why do people treat migraines like they’re just ‘bad headaches’? This is a neurological disorder. If you’re not taking triptans when you need them, you’re basically torturing yourself and your baby with stress hormones. Wake up.
Also, ‘just sleep more’? Nice try. Try sleeping when your newborn screams every 90 minutes. That’s not a lifestyle fix-that’s a cruel joke.
niharika hardikar
While the pragmatic approach outlined herein is commendable, one must critically evaluate the epistemological validity of anecdotal evidence presented under the rubric of ‘real moms.’ The 2023 survey, though numerically robust, lacks methodological transparency regarding selection bias, confounding variables, and longitudinal follow-up.
Furthermore, the normalization of acetaminophen use without reference to emerging concerns regarding endocrine disruption in utero-per the 2022 JAMA Pediatrics meta-analysis-constitutes a dangerous oversimplification of pharmacovigilance principles.
Christine Détraz
Someone said ‘just sleep more’ and I cried. Not because it’s bad advice, but because it’s impossible. I’ve tried blackout curtains, white noise, even a sleep coach. Nothing works when your baby’s awake every two hours.
But Cefaly? I used it for 15 minutes while nursing at 3 a.m. and didn’t have a migraine for 48 hours. That’s the miracle I didn’t know I needed. No pills. No guilt. Just a little headband and a lot of hope.
Also, magnesium. 600 mg. Every night. My legs stopped cramping. My headaches stopped screaming. It’s not glamorous. But it’s real.
Aurora Daisy
Oh wow, an entire article about how to not die from a headache while being a woman. How novel. Next up: ‘How to Not Cry During Breastfeeding Without Taking a Pill.’
Meanwhile, in the UK, we just say ‘get over it’ and hand you a cup of tea. No Cefaly. No triptans. Just tea and silence. Maybe that’s why we’re all so calm.
Paula Villete
So… you’re telling me the thing that’s been wrecking my life for 12 years is treatable… and I just didn’t know because doctors are terrified of saying ‘it’s fine’?
Also, I took Zofran for nausea and it accidentally stopped my migraine. I thought it was just for throwing up. Turns out, my body was like ‘oh hey, you’re in pain? Let me fix that too.’
Also also, I typed ‘acataminophen’ twice. I’m tired. And my brain is foggy. But I’m alive. And that’s enough for today.
Georgia Brach
Let’s examine the data: 78% used acetaminophen and ibuprofen. That’s 973 women. But what’s the sample size of those who developed liver toxicity? Or neonatal thrombocytopenia? Where’s the adverse event reporting?
And triptans? ‘Safe’ based on what? A 2019 cohort study with 87 subjects? That’s not safety-it’s optimism dressed as science.
Also, ‘avoid ergots’-yes. But why not mention that even acetaminophen crosses the placenta? You’re not avoiding risk-you’re just swapping one for another. And calling it ‘safe’ is irresponsible.
Bhargav Patel
The human body is not a machine to be optimized with pills and protocols. It is a living system, shaped by millennia of adaptation. Migraines, in this light, are not merely symptoms-they are signals. A cry for balance.
When we reduce pregnancy to a list of approved medications, we forget that healing often resides not in intervention, but in stillness. In rhythm. In the quiet act of breathing through pain, holding your child, and trusting your body’s wisdom-even when it aches.
That said, magnesium is indeed a gift. And hydration? A sacred practice. These are not ‘tips.’ They are rituals of reverence.
Perhaps the real treatment is not what we take, but how we hold ourselves-gentle, patient, and unashamed-amidst the storm.
Steven Mayer
Based on the pharmacokinetic profiles of CGRP monoclonal antibodies, the absence of robust placental transfer data precludes any recommendation for use during pregnancy. The L2 classification for rimegepant is provisional and derived from extrapolated animal models with limited translational validity.
The cited survey of 1,247 breastfeeding mothers lacks stratification by gestational age at exposure, parity, or comorbid psychiatric conditions-critical confounders in neuropharmacological outcomes.
Moreover, the normalization of non-pharmacological interventions without quantification of efficacy thresholds (e.g., what constitutes ‘significant reduction’ in migraine frequency?) constitutes methodological laxity.
While the intent is commendable, the presentation of this information as clinical guidance risks enabling therapeutic nihilism under the guise of safety.