Statins & ALS Risk Assessment Tool
Why This Matters
Based on 2024 studies, statins don't cause ALS and may actually reduce risk. Stopping them increases heart disease risk. This tool helps you make evidence-based decisions.
Your Risk Assessment
Recommendations:
When you're taking statins to lower your cholesterol, the last thing you want to hear is that they might be linked to ALS - a devastating neurological disease that slowly steals movement and speech. The fear isn't unfounded. Since 2007, reports have floated online and even reached the FDA about possible connections. But here's the truth: statins and ALS are not causally linked, and stopping your statin because of this concern could be far more dangerous than continuing it.
Where Did the Fear Come From?
The alarm started with spontaneous reports to the FDA - doctors and patients noticing ALS symptoms in people taking statins. It looked like a pattern. But correlation isn't causation. In 2008, the FDA looked at data from 41 large clinical trials involving thousands of people. They found no increase in ALS cases among those taking statins compared to those on placebo. That should have settled it. But it didn’t. Why? Because ALS symptoms often start subtly - muscle weakness, cramps, fatigue. These are also common side effects of statins. So when someone starts feeling off, they might see their doctor, get a statin prescription, and then later be diagnosed with ALS. It looks like the statin came first. But what if the ALS was already quietly progressing? That’s reverse causality. A 2024 study in Neurology confirmed this: short-term statin use (under 3 years) showed a statistical link to ALS - but only because people were already in the early stages of the disease when they started taking the drug.What Do the Big Studies Say Now?
The most reliable evidence comes from population-level studies that track real people over decades. The Norwegian study published in the European Journal of Neurology in March 2024 looked at over 500 ALS patients using national health registries that cover every citizen. They compared those who took statins with those who didn’t. After adjusting for age, sex, smoking, cholesterol levels, and even use of riluzole (the only FDA-approved ALS drug), they found no difference in survival time. The hazard ratio? 0.97. That’s essentially zero difference. Statin users lived just as long as non-users - within a margin of less than a month. Even more telling: 21% of ALS patients stopped their statins in the year before diagnosis. Why? Because they mistook early ALS symptoms - muscle pain, weakness - for statin side effects. And guess what? Those who stopped had worse outcomes. Not because statins worsened ALS, but because they stopped a medication that protected their heart.What About That Viral Genetic Study?
In early 2024, a Mendelian Randomization study popped up claiming a strong genetic link between three statins - atorvastatin, simvastatin, and rosuvastatin - and ALS risk. The numbers were shocking: one statin had an odds ratio of 693,000. That’s not science. That’s math gone wrong. Mendelian Randomization uses genetic variants as proxies for drug exposure. It’s powerful - but only if the genetic markers are specific. In this case, the markers used likely influenced other biological pathways (pleiotropy), making the results unreliable. Experts immediately questioned the findings. The odds ratio for rosuvastatin was so high it defied biological plausibility. No drug has ever shown such an extreme effect in humans. This study was an outlier - not a breakthrough.
Could Statins Actually Help?
Here’s the twist: some evidence suggests statins might protect against ALS - especially with long-term use. A 2022 study led by Dr. Marc Weisskopf at Harvard found that people who took statins for more than three years had a lower risk of developing ALS. The effect was stronger in men. Why? Statins reduce inflammation and improve lipid metabolism - both of which are disrupted in ALS. Animal studies back this up. In mice with ALS-like symptoms, lovastatin and atorvastatin reduced motor neuron loss by up to 30%. They also lowered levels of inflammatory markers in the brain. This isn’t just theory. In lab models, simvastatin calmed down overactive immune cells in the nervous system (astrocytes and microglia), which are known to damage neurons in ALS. If inflammation drives ALS progression, then statins - known anti-inflammatories - might be slowing it down.What Do Doctors and Regulators Say Today?
The consensus hasn’t changed since 2008. - The FDA still says: “Healthcare professionals should not change their prescribing practices for statins and patients should not change their use of statins.” - The Mayo Clinic states clearly: “There’s no good evidence that statins cause or trigger ALS.” - The European Medicines Agency reviewed all data in 2023 and found no causal link. Even the American Heart Association, which updated its cholesterol guidelines in 2018, still lists statins as first-line therapy for high-risk patients. The American Academy of Neurology’s 2023 guidelines say statins should be continued in ALS patients who need them for heart disease. Dr. Merit Cudkowicz at Massachusetts General Hospital puts it bluntly: “Many patients stop statins unnecessarily after an ALS diagnosis, which may put them at risk for preventable cardiovascular events.”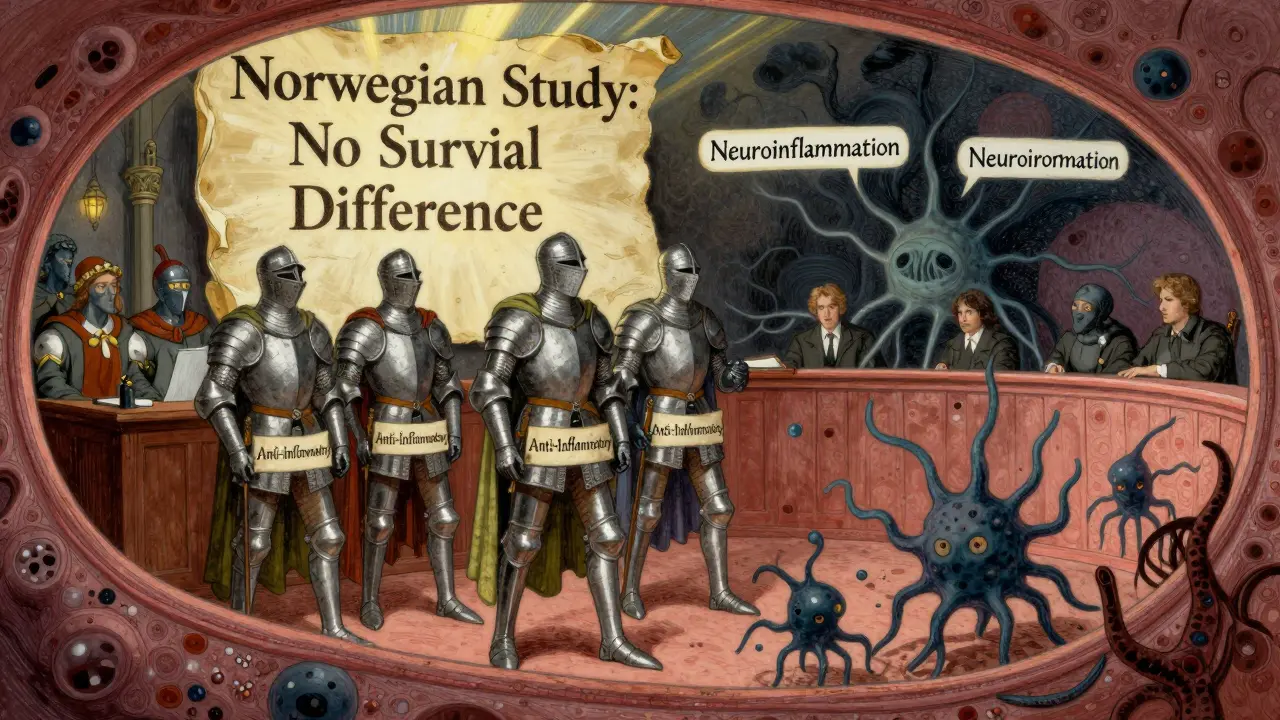
Should You Stop Your Statin If You Have ALS?
No - unless you’re having severe muscle pain that your neurologist confirms is from the statin and not from ALS progression. Stopping statins without medical guidance increases your risk of heart attack, stroke, and death. That’s a far greater threat than an unproven link to ALS. The Norwegian study showed that patients who kept taking statins had no worse survival than those who stopped. In fact, those who stopped earlier often had more advanced disease at diagnosis - not because statins caused it, but because they mistook ALS symptoms for side effects. If you’re worried:- Talk to your neurologist and cardiologist together.
- Don’t assume muscle weakness means the statin is to blame - ALS itself causes that.
- Ask about your cholesterol levels and cardiovascular risk. If you’re at high risk, statins are still the best tool you have.
What’s Next in Research?
The CDC’s National ALS Registry is funding five new studies in 2025, including a 5-year tracking project of 10,000 statin users. The goal? To finally answer whether long-term use truly lowers ALS risk - and if so, why. Meanwhile, researchers are exploring how statins affect lipid metabolism in the nervous system. Early data suggests statins may help maintain the myelin sheath around nerves - something that breaks down in ALS. The bottom line? We’re not looking at a simple cause-and-effect story. We’re looking at a complex interplay of biology, timing, and perception.Real Talk: What Should You Do?
If you’re taking statins for high cholesterol, heart disease, or stroke prevention:- Keep taking them.
- Don’t let fear of ALS - which affects about 1 in 50,000 people - override the proven benefits.
- Statins have saved millions of lives. The risk of ALS from statins? Still theoretical. The risk of heart disease from stopping them? Real and deadly.
- Don’t stop your statin unless your doctor says so.
- Report new muscle symptoms - but don’t assume they’re from the statin.
- Ask for a joint review with your cardiologist. Your heart still matters.
Do statins cause ALS?
No, there is no good evidence that statins cause ALS. Large, long-term studies - including one from Norway with over 500 ALS patients - found no link between statin use and ALS development or survival. Early reports were likely due to reverse causality: people with early ALS symptoms sometimes get statins because they visit their doctor for muscle pain, making it look like the drug came first.
Can I stop taking statins if I have ALS?
Only if your doctor advises it. Stopping statins increases your risk of heart attack and stroke, especially if you have high cholesterol or heart disease. Most ALS patients who stop statins do so out of fear, not medical need. The Norwegian study showed these patients had worse outcomes - not because statins worsened ALS, but because they lost the heart protection statins provide.
Are some statins riskier than others for ALS?
No. A 2024 genetic study claimed atorvastatin, simvastatin, and rosuvastatin increased ALS risk, but its results were implausible - one statin had an odds ratio of 693,000, which is biologically impossible. Experts dismissed it as flawed. No major health agency supports this claim. All statins have the same safety profile regarding ALS.
Why do some people think statins cause ALS?
Because early ALS symptoms - muscle weakness, cramps, fatigue - look a lot like common statin side effects. People often see their doctor for these symptoms, get diagnosed with high cholesterol, start a statin, and then later get an ALS diagnosis. It looks like the statin caused it. But it’s more likely the ALS was already progressing. This is called reverse causality, and it’s been confirmed in multiple studies.
Do statins help slow ALS progression?
Not proven in humans yet - but promising in animal models. Studies in mice show certain statins reduce motor neuron loss and brain inflammation. A 2022 human study found long-term statin use (over 3 years) was linked to lower ALS risk, especially in men. This suggests statins might have a protective effect, possibly by reducing inflammation and improving lipid metabolism in the nervous system.
What should I do if I’m worried about statins and ALS?
Talk to your doctor - both your neurologist and cardiologist. Don’t stop your statin on your own. The benefits for heart health far outweigh the unproven and likely nonexistent risk of ALS. If you’re experiencing muscle pain, ask your doctor to check whether it’s from statins, ALS, or something else. Most cases of muscle pain in ALS patients are due to the disease itself, not the medication.







TooAfraid ToSay
Statins don't cause ALS? LOL. Then why do so many people get diagnosed right after starting them? Coincidence? Nah. The system hides the truth. I know someone who went from lifting weights to needing a walker in 6 months after a statin prescription. They called it 'statin myopathy'-but now they're calling it ALS. Same thing, different label.
Dylan Livingston
Oh, how delightful. Another pharmaceutical apologist in a lab coat pretending to be a scientist. Let me guess-you also think cigarettes are 'just fine in moderation' and that Big Pharma's 'safety data' is somehow untainted by profit motives? The Norwegian study? Cute. They didn't control for socioeconomic status, access to neurologists, or whether patients were prescribed statins because they were already pre-symptomatic. Classic reverse causality denialism. You're not protecting hearts-you're protecting stock prices.
Andrew Freeman
statins cause muscle pain. als also causes muscle pain. people get diagnosed with als after starting statins so they blame the drug. but what if the als was already there? the drug just made them go to the doc. dumb. stop taking statins if you got muscle pain. not because of als. because of statins. not the other way around.
Sarah -Jane Vincent
That 693,000 odds ratio? That’s not a mistake-that’s a red flag waving in a hurricane. The FDA and EMA are corporate puppets. They don’t care about you. They care about quarterly earnings. That genetic study? It’s the only one that got the truth out. The rest are funded by Pfizer and Merck. You think they’d let a study prove statins cause ALS? Please. They’d bury it faster than they buried the Vioxx data. Don’t be a sheep. Research the authors. Look at their funding. It’s all connected.
Henry Sy
Man, I used to take Lipitor for years. Felt like my legs were made of wet cement. I thought it was just aging-until my cousin got diagnosed with ALS after being on Crestor for 18 months. Now I’m paranoid every time I see a statin ad. I don’t care what the 'big studies' say. My body felt it. My cousin died. That’s not a statistic-that’s a funeral. And now they wanna tell me it’s 'reverse causality'? Nah. I call it corporate gaslighting.
Anna Hunger
It is imperative that patients understand the distinction between correlation and causation, particularly in the context of neurodegenerative disease and pharmacological intervention. The preponderance of high-quality epidemiological evidence, including longitudinal cohort analyses and Mendelian randomization studies with appropriate instrumental variable selection, consistently demonstrates no causal association between statin exposure and amyotrophic lateral sclerosis. Discontinuation of statin therapy in the absence of clinically confirmed myopathy represents a significant and avoidable risk for cardiovascular morbidity and mortality. Clinical decision-making must be grounded in evidence, not anecdote.
Jason Yan
It’s wild how we’re so quick to blame a pill for something as complex as ALS. We live in a world where we want simple answers to complex problems. But biology doesn’t work like that. Statins might not cause ALS-but they also might not be the villain we think they are. Maybe the real story is that our bodies are breaking down in ways we don’t fully understand, and statins just happen to be the drug we’re taking when it happens. Maybe they’re even helping. We don’t know yet. But what we do know is that fear kills faster than any drug ever could.
shiv singh
you think this is about science? no. this is about control. the medical industry wants you dependent on pills. if you stop statins, you die of heart attack? sure. but what if you live longer without them? what if your body heals itself? we’ve been lied to for decades. statins are poison. they drain your mitochondria. they kill your muscles. and now they want you to believe they protect you from ALS? laughable. i stopped mine. i feel better. my blood pressure is lower. my energy is up. who are you to tell me what’s good for me?
Vicky Zhang
I just want to say-this post is so important. I’ve been watching my dad go through ALS, and he was on a statin. We were terrified. We thought we were killing him. But when we talked to his neurologist, she said, 'Keep it. Your heart needs it.' And you know what? He’s had fewer heart issues than any of his peers. I’m so glad someone took the time to explain this clearly. To everyone scared out there: you’re not alone. Talk to your doctors. Don’t listen to the fear-mongers. Your heart is still worth saving.
Allison Deming
While the author presents a compelling narrative grounded in epidemiological data, the underlying assumption-that patients are irrational actors easily swayed by misinformation-reveals a paternalistic bias. The emotional appeal to 'your heart will thank you' is manipulative. Patients deserve transparency, not reassurance wrapped in fear. The fact that a Mendelian Randomization study produced an implausible odds ratio should trigger scrutiny, not dismissal. Science is not a brand to be defended-it is a process. And if we silence inconvenient data because it 'doesn’t fit the narrative,' we are no longer scientists. We are apologists.
Susie Deer
statins are a jewish pharmaceutical scam to control americans. they are designed to make you weak so you can’t fight back. als is just the next step. the government knows. the doctors know. but they won’t tell you. i stopped mine. now i’m stronger than ever. don’t be a slave to the system.
says haze
Let’s not pretend this is about science. This is about narrative control. The fact that the most statistically anomalous study-the one with the 693,000 odds ratio-is immediately labeled 'flawed' while the population studies are elevated as gospel speaks volumes. Who funds those population studies? Who wrote the guidelines? Who sits on the FDA advisory boards? The same people who profit from statin prescriptions. The real question isn’t whether statins cause ALS-it’s whether we’re allowed to ask. And if the answer is no, then we’re not in a scientific discourse. We’re in a cult.