Antibiotic Sun Safety Calculator
Your results will appear here
When you're prescribed doxycycline or TMP-SMX (Bactrim, Septra), your doctor focuses on fighting infection. But there’s another side effect that doesn’t always get mentioned-your skin becomes dangerously sensitive to sunlight. You might think a quick walk to the mailbox or sitting by a window won’t hurt. That’s a mistake. These antibiotics can turn a normal day outside into a painful sunburn in under an hour-even on cloudy days or through glass.
Why Doxycycline and Bactrim Make Your Skin Burn So Easily
Doxycycline and TMP-SMX don’t just kill bacteria-they react with sunlight in a way that damages your skin cells. This isn’t just a mild rash. It’s phototoxicity: a chemical reaction triggered when UV light hits the drug molecules in your skin. About 20% of people taking doxycycline at standard doses (200 mg daily) experience this. For TMP-SMX, the risk is similar, and the reaction can stick around for weeks after you stop taking it.
The science is clear: tetracyclines like doxycycline absorb UVA rays (320-400 nm), which penetrate deep into the skin and create free radicals. These molecules wreck cell membranes, leading to redness, blistering, and peeling. TMP-SMX works differently but hits the same target. Studies show it can cut your skin’s natural sun protection in half. That means if you normally burn after 20 minutes in the sun, you might burn in 10-or less-while on these drugs.
And here’s what most people don’t realize: you don’t need to be at the beach. Sitting near a window at home, driving in the car, or walking to your car in the morning can be enough. UVA rays pass right through glass. So even if you’re indoors, your skin is still at risk.
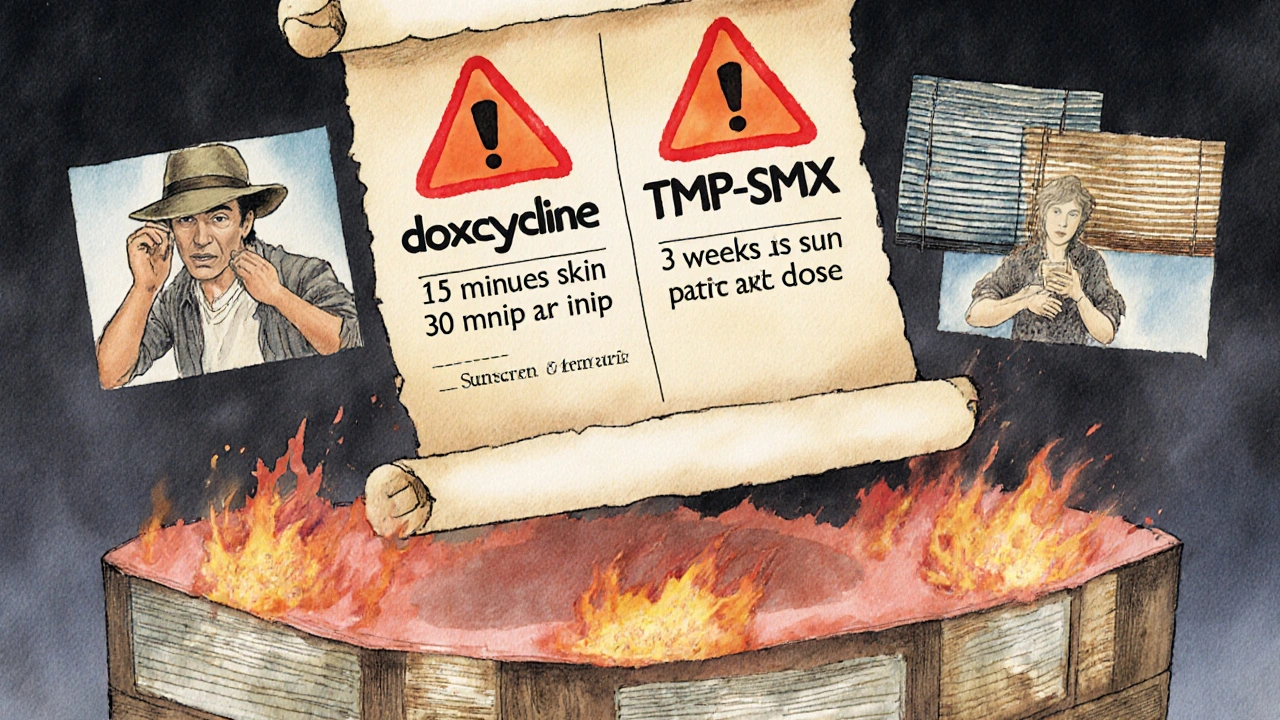
How Fast Can a Reaction Happen?
With doxycycline, symptoms usually show up within 30 minutes to 24 hours after sun exposure. You’ll see redness, swelling, and a burning sensation-like a bad sunburn but often more localized to areas like your neck, shoulders, or the backs of your hands. TMP-SMX can be even trickier. Some people report reactions after just 15 minutes of sun. And unlike doxycycline, where the risk fades within a few days of stopping the drug, TMP-SMX can keep reacting for up to three weeks after your last pill.
One study tracked 10 patients on doxycycline 200 mg daily. Two of them developed full-blown phototoxic reactions after brief outdoor exposure. Another study on demeclocycline (a close cousin of doxycycline) found 9 out of 10 patients burned severely-even with minimal sun. These aren’t rare cases. They’re expected outcomes.
Which Antibiotics Are the Worst Offenders?
Not all antibiotics cause this. Penicillin? Low risk. Amoxicillin? Almost none. But among the commonly prescribed ones, doxycycline and TMP-SMX are top of the list. Fluoroquinolones like ciprofloxacin and levofloxacin are also risky, but less common than tetracyclines and sulfonamides.
Here’s the breakdown:
- High risk: Doxycycline, demeclocycline, TMP-SMX (Bactrim, Septra)
- Moderate risk: Ciprofloxacin, levofloxacin, tetracycline
- Low to no risk: Amoxicillin, azithromycin, cephalexin, clindamycin
Doctors often say, “Some antibiotics cause sun sensitivity,” but that’s too vague. If you’re on doxycycline or Bactrim, you’re in the high-risk group. No guessing. No hoping it won’t happen. It will-if you’re exposed.
What Sun Protection Actually Works
Standard sunscreen isn’t enough. You need broad-spectrum SPF 30 or higher-and you need to apply it right. Most people apply too little. The Skin Cancer Foundation recommends a shot glass full for your whole body. Reapply every two hours, or after sweating or towel-drying. And don’t forget your ears, lips, neck, and the tops of your feet.
But sunscreen alone won’t save you. You need physical barriers. Wear long-sleeved shirts made of tightly woven fabric. Look for clothing labeled UPF 30+-regular cotton T-shirts only block about UPF 5. A wide-brimmed hat (at least 3 inches) is non-negotiable. Sunglasses with UV protection? Essential. Your eyes aren’t immune either.
And yes, you still need protection indoors. If you sit by a window for an hour, your skin is getting UVA exposure. Close blinds or use UV-filtering window film if you’re on these drugs long-term.

Timing Matters: When to Stay Inside
UV radiation peaks between 10 a.m. and 4 p.m. That’s when you’re most at risk. Plan outdoor tasks-walking the dog, gardening, running errands-for early morning or late afternoon. If you have to be outside during peak hours, cover up completely. No shortcuts.
Even in Manchester, where it’s often overcast, UV levels can be high enough to trigger a reaction. Don’t let the weather fool you. Clouds block visible light, not UVA. Your skin can’t tell the difference.
What Happens If You Ignore the Warnings?
Most people think, “I’ve been outside before, nothing happened.” But photosensitivity isn’t cumulative-it’s explosive. One bad exposure can leave you with a blistering rash that takes weeks to heal. In some cases, it leads to permanent dark spots or scarring.
Long-term? Repeated reactions increase your risk of skin cancer. The FDA and Skin Cancer Foundation both warn that drug-induced photosensitivity isn’t just about discomfort-it’s a cancer risk factor. Every burn adds up. And with doxycycline often prescribed for months (like for acne or Lyme disease), the exposure adds up too.
One study found that 40% of patients stop using sunscreen within the first week of taking these antibiotics because it’s “too much trouble.” That’s dangerous. If you skip protection, you’re not just risking a bad sunburn-you’re risking your skin’s long-term health.
How Long Do You Need to Stay Protected?
For doxycycline: protect your skin for the entire time you’re on the drug-and for at least 5 days after your last dose. The drug clears from your system fairly quickly.
For TMP-SMX: protect yourself for up to three weeks after your last pill. The sulfamethoxazole component lingers in your skin and can still react to UV light. Many patients don’t know this. They stop the medication, think they’re safe, and get burned walking to their car. Don’t be one of them.
What If You Already Got Burned?
If you notice redness, pain, or blistering after sun exposure while on these drugs:
- Get out of the sun immediately.
- Cool the area with a damp cloth or cool bath-no ice.
- Apply aloe vera or a fragrance-free moisturizer.
- Take an over-the-counter pain reliever like ibuprofen to reduce inflammation.
- Do NOT pop blisters. That increases infection risk.
- Call your doctor if the burn covers a large area, is very painful, or shows signs of infection (pus, swelling, fever).
Don’t wait to see if it gets better. Early care prevents complications.
What Your Doctor Should Have Told You
Many patients say their doctor never mentioned sun sensitivity. That’s a gap in care. The FDA requires sun safety warnings on the labels of doxycycline and TMP-SMX. If your provider didn’t explain it, ask. Say: “I’ve heard these antibiotics can make me burn easily-what do I need to do?”
Pharmacies often include printed warnings, but they’re easy to miss. Don’t rely on a leaflet. Get the info straight from your provider. Write it down. Share it with a family member. Make it part of your daily routine.
Final Rule: Treat Your Skin Like a Sensitive Organ
These antibiotics are powerful tools. But they come with a trade-off: your skin becomes more vulnerable. You don’t have to give up being outside. You just need to be smarter about it.
Wear sunscreen daily. Cover up. Avoid midday sun. Stay protected even after you finish the pills. This isn’t about being paranoid-it’s about being informed. Your skin doesn’t heal the same way it used to. And once it’s damaged, you can’t undo it.
Don’t let a simple infection cost you your skin’s health. Protect it like you’d protect a child’s-because you’re worth it.
Can I still go outside if I’m taking doxycycline or Bactrim?
Yes, but you must take strict sun protection steps. Avoid direct sunlight between 10 a.m. and 4 p.m., wear UPF 30+ clothing, use broad-spectrum SPF 30+ sunscreen, and wear a wide-brimmed hat and sunglasses. Even sitting near a window can trigger a reaction, so don’t assume you’re safe indoors.
How long does sun sensitivity last after stopping doxycycline or Bactrim?
For doxycycline, sun sensitivity usually fades within 5 days after your last dose. For TMP-SMX (Bactrim), it can last up to three weeks. The active ingredient in Bactrim stays in your skin longer and can still react to UV light even after you’ve stopped taking it. Don’t assume you’re safe just because you finished the pills.
Is SPF 15 enough if I’m on these antibiotics?
No. SPF 15 blocks about 93% of UVB rays, but it doesn’t offer enough UVA protection, which is what triggers photosensitivity with these drugs. Use SPF 30 or higher, and make sure it’s labeled “broad-spectrum.” Apply a full shot glass amount to your entire body and reapply every two hours.
Can I use tanning beds while on doxycycline or Bactrim?
Absolutely not. Tanning beds emit concentrated UVA radiation-exactly the type that triggers severe phototoxic reactions with these antibiotics. Even one session can cause serious burns, blistering, and long-term skin damage. Avoid them completely while on these drugs and for weeks after.
Do I need to avoid the sun if I’m only taking a 5-day course?
Yes. Even short courses can cause phototoxic reactions. Studies show reactions can occur within 30 minutes of sun exposure. Don’t wait until you’ve been on the drug for days to start protecting yourself. Begin sun safety the first day you take the medication.
Are there any antibiotics that don’t cause sun sensitivity?
Yes. Penicillin-based antibiotics like amoxicillin, macrolides like azithromycin, and cephalosporins like cephalexin have very low or no risk of photosensitivity. If you’re concerned about sun exposure, ask your doctor if a lower-risk antibiotic is appropriate for your condition.
What should I do if I get a sunburn while on these antibiotics?
Get out of the sun immediately. Cool the area with a damp cloth or lukewarm bath. Apply aloe vera or a fragrance-free moisturizer. Take ibuprofen for pain and swelling. Do not pop blisters. Contact your doctor if the burn is severe, covers a large area, or shows signs of infection like pus or fever.





Christopher K
Oh wow, finally someone who gets it. I got burned so bad on doxycycline I looked like a boiled lobster after walking to my damn mailbox. My doctor said 'just use sunscreen' like that’s a magic shield. Nah. I wore SPF 50, a hat, gloves, and a goddamn tinfoil cape-and still got roasted. These drugs are sneaky bastards.
Andy Feltus
It’s funny how we treat our skin like it’s disposable. We’ll take a pill that turns our body into a solar target and then act surprised when it breaks down. We live in a world where convenience is worshipped, but biology doesn’t care about your schedule. The real tragedy isn’t the burn-it’s that no one teaches you to respect your own body until it’s too late.
Dion Hetemi
Let me break this down for the slow ones: Doxycycline + sun = chemical warfare on your epidermis. TMP-SMX? Even worse. The FDA warns about this. The Skin Cancer Foundation warns about this. Your pharmacist printed a warning in 6-point font you didn’t read. This isn’t speculation-it’s documented, peer-reviewed, and backed by clinical data. If you’re still ‘hoping it won’t happen,’ you’re not just naive-you’re a liability to your own health.
Kara Binning
Okay but like… I took Bactrim for a UTI and went to the grocery store at 2 p.m. and came back looking like I’d been dipped in hot wax. My husband thought I was having a stroke. I cried for three days. My skin peeled like a snake. And guess what? My doctor didn’t say a word. Not one. I had to Google it. This is medical negligence disguised as ‘standard care.’
river weiss
Proper sun protection requires diligence, not hope. Broad-spectrum SPF 30+ applied generously-approximately 2 milligrams per square centimeter of skin-is non-negotiable. Reapplication every 120 minutes, or immediately after perspiration or dermal contact with water or fabric, is essential. Clothing with UPF 30+ or higher is superior to sunscreen alone. UVA penetrates glass; therefore, indoor exposure near windows must be mitigated via film or shade. Duration of photosensitivity risk extends beyond cessation of therapy for sulfonamides-up to 21 days. These are evidence-based, clinically validated precautions.
Brian Rono
Let’s be brutally honest: this post is 98% correct. But you missed the elephant in the room-Big Pharma doesn’t care if you burn. They make billions off antibiotics, and a little phototoxicity? Just a footnote in the fine print. Meanwhile, your dermatologist is charging $300/hour to fix the scarring you didn’t know was coming. Wake up. The system doesn’t warn you because it profits from your ignorance.
Zac Gray
I get it-you’re scared. I was too. But you don’t have to live in a cave. I took doxycycline for Lyme for six months. I walked my dog at 7 a.m., wore a long-sleeve UPF shirt, a hat, and sunglasses. I reapplied sunscreen like it was my job. I didn’t get burned once. It’s not about avoiding life-it’s about adjusting it. You’re not powerless. You just need a plan.
Steve and Charlie Maidment
Why are we all acting like this is new? My grandma took tetracycline in the '70s and told me about her sunburns. People just forget. And now everyone acts like they’re the first person to ever get burned by a pill. Newsflash: this has been known for 60 years. The real problem isn’t the antibiotic-it’s the collective amnesia of modern medicine.
Michael Petesch
In Japan, patients are routinely given sun safety pamphlets with antibiotics like doxycycline. The cultural emphasis on preventative care is far more integrated. In the U.S., we treat health as an afterthought until something breaks. Is this disparity in patient education a reflection of systemic priorities-or simply a lack of public health infrastructure?
Andrew Montandon
Thank you for this. Seriously. I’m a nurse, and I’ve seen too many patients come in with third-degree burns from ‘just walking to the car.’ I tell everyone: if your antibiotic has ‘tetracycline’ or ‘sulfonamide’ in the name, treat your skin like it’s made of tissue paper. And yes, even indoors. I’ve had patients ask if they can ‘just sit by the window’-and I say: no. Not even for five minutes. Your skin doesn’t know the difference between sunlight and a tanning bed.
Sam Reicks
the whole sun thing is a lie i think the gov wants us to stay inside so they can track us better with the cameras and the drones and also sunscreen is full of chemicals that make you more sensitive like the aluminum and the parabens and the microplastics and the 5g towers are making it worse i got burned even when i was in my basement with the lights off so its definitely the moon or something
Chuck Coffer
Of course you got burned. You probably didn’t even use the right sunscreen. Most people just slap on whatever’s on sale. SPF 15? From a drugstore? You’re not protecting yourself-you’re performing a ritual. And now you’re surprised your skin turned into a raisin? You didn’t follow the rules. You didn’t prepare. You didn’t read the fine print. You got what you deserved.
Marjorie Antoniou
I just want to say: if you’re reading this and you’re scared, you’re not alone. I was on doxycycline for acne and thought I’d be fine. I got burned on my shoulders and cried for hours. But I learned. I bought a sun hat, I wear long sleeves even in summer, and I keep sunscreen in my car, my bag, and my desk. It’s not about being perfect-it’s about being consistent. You’re worth the effort.
Paige Lund
Yeah, I guess I should’ve read the pamphlet. But honestly? I just wanted the acne to go away. Now I have permanent dark spots. Great. Thanks, medicine.