Carrying extra weight isn’t just a cosmetic concern for people with type 2 diabetes-it’s a major driver of the disease. The good news? Losing even a small amount of weight can dramatically improve blood sugar control, reduce medication needs, and in some cases, send diabetes into remission. This isn’t theoretical. Real people with real diabetes are reversing their condition-not with magic pills, but with consistent, science-backed changes to how they eat, move, and think about their health.
Why Weight Loss Matters So Much for Diabetes
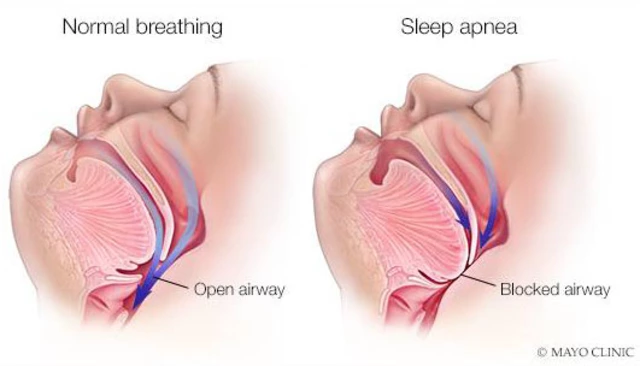
When you carry excess fat, especially around your belly, your body becomes resistant to insulin. That means your pancreas has to work harder to push glucose into your cells. Over time, the pancreas burns out, and blood sugar climbs. Losing weight reverses this process. Studies show that losing just 5% of your body weight can improve insulin sensitivity by up to 40%. That’s why the American Diabetes Association now treats weight loss as a core treatment, not just a side goal.
Take the DiRECT trial, for example. People with type 2 diabetes who lost an average of 10 kilograms (about 22 pounds) had a 46% chance of going into remission after one year. Remission doesn’t mean a cure-it means their blood sugar returned to normal without needing diabetes meds. And it wasn’t because of surgery or extreme diets. It was because they ate fewer calories, focused on whole foods, and kept at it.
How Much Weight Do You Actually Need to Lose?
You don’t need to drop 50 pounds to see results. In fact, aiming for too much too fast can backfire. The sweet spot? Lose 5% to 7% of your starting weight. For someone who weighs 200 pounds, that’s 10 to 14 pounds. That’s it. That’s enough to lower your A1C by 0.5% to 1%, reduce blood pressure, and cut your risk of heart disease.
The Diabetes Prevention Program (DPP) proved this decades ago. People with prediabetes who lost 5-7% of their body weight cut their risk of developing type 2 diabetes by 58%. That’s better than the drug metformin. And the same numbers hold true for people already diagnosed. Losing even 5% can mean fewer pills, fewer doctor visits, and more energy.
What to Eat: The Real Nutrition Rules
Forget fad diets. The most effective eating plan for diabetes and weight loss is simple: fewer calories, more fiber, and smarter carbs.
- Focus on high-fiber carbs: Aim for at least 14 grams of fiber per 1,000 calories. That means swapping white bread for whole grain, sugary cereal for oats, and potatoes for beans or lentils. Fiber slows digestion, keeps you full, and prevents blood sugar spikes.
- Control portions: Use smaller plates. Measure your food for the first few weeks. A serving of pasta isn’t a big bowl-it’s a cup, about the size of a tennis ball. A serving of meat is the size of your palm.
- Choose lean protein: Chicken, fish, tofu, eggs, and legumes help you feel full longer and protect muscle mass while you lose fat. Protein also helps stabilize blood sugar between meals.
- Limit added sugar and refined carbs: Soda, candy, pastries, and white rice spike blood sugar fast and make hunger come back quickly. Water, herbal tea, or sparkling water are better choices.
The Mediterranean diet has shown strong results in studies like DiRECT. It’s not about cutting out entire food groups-it’s about eating more vegetables, olive oil, nuts, fish, and whole grains, and less processed stuff. You don’t have to go full keto or vegan. Just eat more real food and less packaged food.

Move More-But Not Just Walking
Walking is great. But if you only walk, you’ll hit a plateau. To lose weight and keep it off, you need two types of movement: aerobic activity and strength training.
- Aerobic exercise: Aim for 150 minutes a week-about 30 minutes, five days a week. Brisk walking, cycling, swimming, or dancing all count. If you’re new to this, start with 10 minutes a day and build up.
- Strength training: Do this at least twice a week. Use resistance bands, dumbbells, or your own body weight (squats, push-ups, lunges). Muscle burns more calories at rest than fat. Building muscle helps your body use insulin better.
One user on Reddit shared that after losing 18 pounds with just walking, they got stuck. When they added two days of bodyweight workouts, the weight started coming off again. That’s not coincidence. Muscle changes your metabolism.
Medications That Help (and Those That Don’t)
Your meds matter. Some diabetes drugs cause weight gain. Others help you lose weight. Talk to your doctor about switching if you’re struggling.
- Weight-loss friendly: GLP-1 agonists like semaglutide (Wegovy, Ozempic) and tirzepatide (Mounjaro) can help people lose 15% or more of their body weight. SGLT2 inhibitors like empagliflozin also promote weight loss by making your body pee out extra sugar.
- Weight-gain risk: Insulin and sulfonylureas (like glipizide) often cause weight gain. They lower blood sugar by forcing your body to make more insulin-which can increase hunger and fat storage.
If you’re on insulin and trying to lose weight, work with your provider to adjust doses. Too much insulin during weight loss can lead to low blood sugar and cravings. Don’t try to cut insulin on your own-this can be dangerous. But with the right support, many people reduce their insulin needs as they lose weight.

Technology Can Be Your Secret Weapon
Apps aren’t magic, but they’re powerful tools. Tracking your food with MyFitnessPal or Lose It! helps you see where calories sneak in. A 2023 survey found that 85% of users who used portion-control tools like measuring cups and smaller plates stuck with their plan longer.
Continuous glucose monitors (CGMs) are no longer just for people on insulin. Many find them helpful for learning how different foods affect their blood sugar. Seeing your glucose spike after a banana or a bowl of rice can be eye-opening. It turns abstract advice into real-time feedback.
Virtual coaching programs like the CDC’s National Diabetes Prevention Program (NDPP) are covered by Medicare and many private insurers. You get 16 sessions in six months with a certified coach, plus ongoing support. People who complete the program lose 5-7% of their weight on average-and keep it off better than those who try alone.
What Gets in the Way-And How to Beat It
Most people don’t fail because they lack willpower. They fail because they don’t plan for the real obstacles.
- Emotional eating: Stress, boredom, or sadness can trigger overeating. Try journaling your feelings before you eat. Ask: “Am I hungry, or am I upset?”
- Plateaus: After a few months, weight loss slows. That’s normal. Add more movement, tweak your portions, or try intermittent fasting (like eating within an 8-hour window). Don’t give up.
- Hypoglycemia: If you’re on insulin or sulfonylureas, losing weight can make low blood sugar more likely. Keep fast-acting carbs (glucose tablets, juice) on hand. Talk to your doctor about adjusting doses before you start losing weight.
- Social pressure: Family gatherings, office snacks, and celebrations can derail progress. Plan ahead. Eat a healthy snack before going out. Bring a dish you know is safe. Say no politely.
One person in a diabetes forum said, “I lost 22 pounds in six months. My A1C dropped from 7.2% to 5.9%. But the real win? I can now play with my grandkids without getting winded.” That’s the kind of motivation that lasts.
Realistic Expectations: This Is a Lifelong Shift
Weight loss isn’t a sprint. It’s a long-term habit change. The Look AHEAD study showed that only 27% of participants kept off 10% of their weight after four years. That sounds discouraging-but it’s not. Those who succeeded didn’t rely on willpower. They built systems: meal prep on Sundays, weekly check-ins with a friend, tracking progress in a journal, celebrating non-scale wins like better sleep or climbing stairs without pain.
Remission is possible. But it requires consistency, not perfection. Miss a day? Get back on track the next. Eat too much at dinner? Walk after. It’s the pattern over weeks and months that matters.
The goal isn’t to be thin. It’s to be healthy. To feel strong. To live longer without pills, hospital visits, or complications. And that’s something every person with type 2 diabetes can achieve-even if they start at 300 pounds.
Can you reverse type 2 diabetes by losing weight?
Yes, in many cases. Losing 10% or more of your body weight, especially early in the disease, can lead to diabetes remission-meaning your blood sugar returns to normal without medication. This has been proven in studies like DiRECT, where nearly half of participants achieved remission after losing an average of 10 kg. It’s not a cure, but it’s a powerful reversal of the disease process.
How fast should I lose weight with diabetes?
Aim for 1 to 2 pounds per week. That’s about a 500-750 calorie daily deficit. Losing weight too fast can lead to muscle loss, nutrient deficiencies, and increased risk of low blood sugar, especially if you’re on insulin. Slow and steady is safer and more sustainable.
Is it safe to lose weight while on insulin?
Yes, but you must work with your doctor. As you lose weight, your body needs less insulin. If your dose stays the same, you risk dangerous low blood sugar. Your provider should adjust your insulin dose as you lose weight-often before significant loss begins. Never change your dose without medical guidance.
What’s the best diet for weight loss with type 2 diabetes?
There’s no single “best” diet, but the most effective ones focus on whole foods, high fiber, lean protein, and portion control. The Mediterranean diet, DASH diet, and lower-carb high-fiber plans have all shown strong results. Avoid extreme diets. Pick one you can stick to long-term, not just for a few weeks.
Do I need to exercise to lose weight with diabetes?
You can lose weight with diet alone, but exercise makes it easier and keeps the weight off longer. Strength training builds muscle, which improves insulin sensitivity. Cardio burns calories and helps heart health. Combining both gives you the best results-and more energy to enjoy life.
Can I use weight-loss drugs like Ozempic or Wegovy for diabetes?
Yes, and they’re increasingly prescribed for people with type 2 diabetes who need help losing weight. Semaglutide (Wegovy, Ozempic) and tirzepatide (Mounjaro) not only promote weight loss but also improve blood sugar control and reduce heart risks. However, they can cause nausea or digestive side effects, and they’re expensive. Talk to your doctor about whether they’re right for you.
How do I stay motivated when weight loss slows down?
Focus on non-scale victories: better sleep, more energy, clothes fitting better, lower blood pressure, or needing fewer pills. Track your progress with photos, measurements, or how you feel-not just the scale. Join a support group or find an accountability partner. Remind yourself why you started: to live longer, feel stronger, and take control of your health.
Managing diabetes isn’t about perfection. It’s about progress. One healthy meal. One walk. One week of better sleep. Those small wins add up. And if you’ve been told you need to lose weight to control your diabetes-you’re not being blamed. You’re being given the most powerful tool you have to take back your health.





Sumler Luu
Just wanted to say this post hit different. I lost 12 lbs in 4 months by switching to whole grains and walking after dinner. My A1C dropped from 7.1 to 6.0. No meds changed. Just food and movement. Small wins matter.
Still have bad days. But now I know it’s not about being perfect-it’s about showing up.
sakshi nagpal
As someone from India, I can confirm that traditional diets-like dal, roti, and vegetables-are naturally aligned with diabetes management. The problem isn’t the food-it’s the industrialization of our plates. We swapped homemade meals for packaged snacks and wondered why our numbers spiked.
Reverting to simple, seasonal, and locally sourced food made all the difference. No gimmicks. Just truth.
Nikki Brown
Ugh. Another ‘just eat less and move more’ article. 🙄 Like that’s some revolutionary insight. You didn’t mention the fact that Big Pharma profits from keeping people medicated, did you? Or that insulin resistance is often caused by chronic stress and sleep deprivation, not just ‘bad choices’?
People are tired of being shamed while the real culprits-processed food corporations and lazy doctors-get rich.
Peter sullen
While the foundational principles outlined herein are empirically sound, I would like to posit a more granular analysis of the thermodynamic and endocrinological dynamics at play. Specifically, the reduction in adipocyte hypertrophy leads to decreased secretion of pro-inflammatory cytokines-namely TNF-alpha and IL-6-which directly ameliorate insulin receptor signaling dysfunction.
Furthermore, the implementation of resistance training elevates GLUT-4 translocation efficiency, thereby enhancing glucose uptake independent of insulin. A longitudinal cohort study (2022, JAMA Endocrinology) corroborates this mechanism with a 58.3% improvement in HOMA-IR scores among participants adhering to the prescribed regimen.
Natasha Sandra
OMG I DID THIS AND IT WORKED 😭
I started using a tiny plate. A TEENY ONE. And I stopped drinking soda. Just. Stopped. I lost 15 lbs in 3 months. My shoes don’t pinch anymore. My husband said I look like I have energy again. I’m not ‘cured’ but I feel like ME again.
Also-yes, Ozempic is a miracle. But you don’t need it. You just need to stop lying to yourself about how much sugar you’re eating.
Erwin Asilom
I’ve been helping people with prediabetes for over a decade. The most consistent factor in success isn’t the diet-it’s consistency. People who track their meals for even just 30 days develop awareness. Awareness leads to choice. Choice leads to change.
Most fail because they treat it like a 30-day challenge. It’s not. It’s a lifestyle. One meal at a time.
Sandeep Jain
bro i was skeptical but i started eating oats for breakfast and walking 20 min after dinner… lost 18 lbs in 5 months. my doc was shocked. i didnt even know i was eating so much rice. now i just use less. its not hard. just slow.
roger dalomba
Wow. A whole article about losing weight. Groundbreaking.
Next up: ‘Water hydrates you.’
Also, if you need a 16-page guide to stop eating cake, maybe you shouldn’t be allowed near kitchens.
Brittany Fuhs
Why do Americans think they’re the first to figure out that eating real food helps? We’ve been doing this in Europe for centuries. No fancy apps. No CGMs. Just potatoes, bread, and wine. And we didn’t get fat. You overcomplicate everything.
Also, ‘Mediterranean diet’? That’s just what normal people ate before you turned food into a science project.
Sophia Daniels
Let’s be real: if you’re still on insulin and trying to ‘lose weight naturally,’ you’re fighting a losing battle. The system is rigged. Big Pharma doesn’t want you to reverse diabetes-they want you to buy Ozempic every month.
I lost 32 lbs on semaglutide. My A1C went from 8.9 to 5.6. I’m off insulin. I’m not ashamed. I used the tools available. If you’re mad about it, go cry to your doctor who prescribed you glipizide in 2010 and never updated your plan.
Stop romanticizing willpower. This isn’t a morality play. It’s biochemistry.
Steven Destiny
You’re not broken. You’re not lazy. You’re not failing. You’re just fighting a system designed to make you sick. Every time you choose a salad over fries, you’re winning. Every time you walk instead of scrolling, you’re reclaiming your life.
I lost 40 lbs. I’m off meds. I play basketball with my son now. It’s not easy. But it’s worth it. Keep going. You’re doing better than you think.
Fabio Raphael
I’m curious-how do people who are food insecure or on fixed incomes navigate this? The ‘eat whole foods’ advice sounds great until you realize fresh veggies cost more than a box of cereal. And not everyone can afford a CGM or a gym membership.
There’s a lot of privilege baked into these ‘simple’ solutions. I’d love to hear how others are adapting this for real life-not just Instagram lives.
Amy Lesleighter (Wales)
just eat less sugar. walk. sleep. dont stress. its not that hard. you dont need apps or fancy diets. your body knows what to do. you just gotta stop messing with it.
Becky Baker
So you’re telling me I have to stop eating pizza? Like, forever? I’m out.