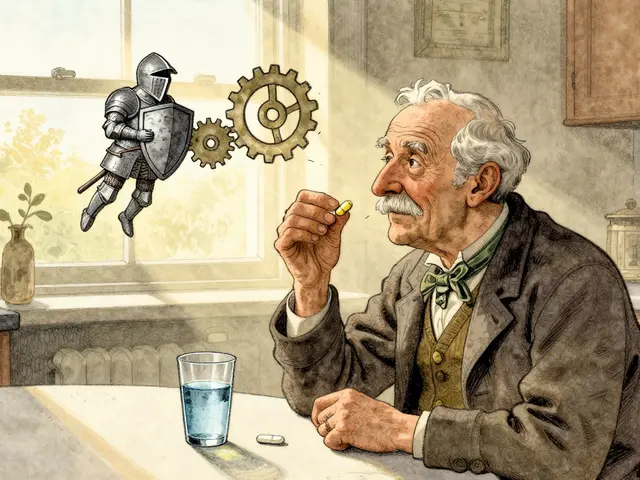
Switching from brand-name to generic immunosuppressants can save thousands of dollars a year - but for transplant patients, that savings might come with a hidden risk. Cyclosporine and tacrolimus aren’t like regular pills. They’re narrow therapeutic index drugs, meaning the difference between a dose that works and one that causes rejection or toxicity is razor-thin. When generics are swapped without careful monitoring, levels can swing dangerously. And for people who’ve waited years for a new organ, that’s not just inconvenient - it’s life-threatening.
Why These Drugs Are So Sensitive
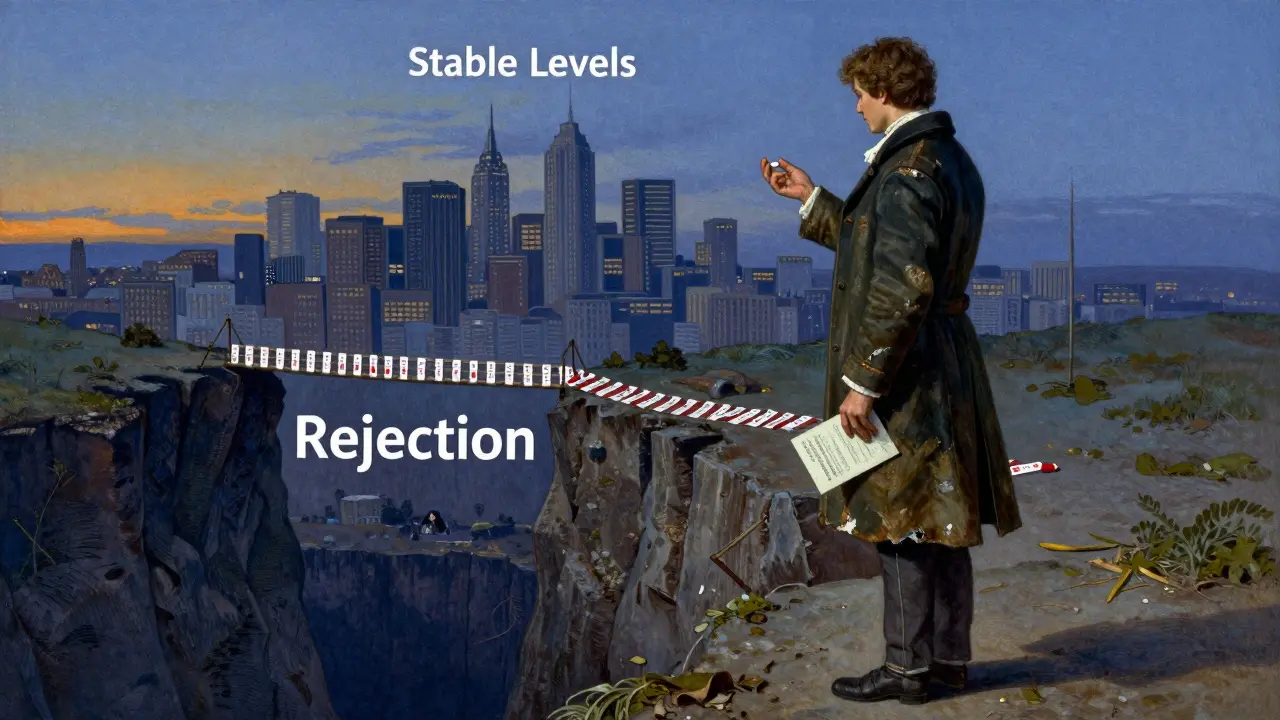
Both cyclosporine and tacrolimus work by blocking calcineurin, a protein that turns on T-cells. No T-cell activation means no immune attack on the transplanted organ. But here’s the catch: your body absorbs these drugs differently depending on what’s in the pill. Cyclosporine comes in oil-based or microemulsion forms. Tacrolimus is absorbed through the gut lining, and even tiny changes in the filler or coating can alter how much gets into your bloodstream. Tacrolimus is 20 to 100 times more potent than cyclosporine. A typical daily dose? Around 5 mg twice a day for tacrolimus. For cyclosporine? About 150 mg twice a day. That might sound like a big difference, but the real issue is precision. Tacrolimus blood levels need to stay between 5 and 15 ng/mL in the first few months after transplant. Go below 5? Rejection risk spikes. Above 15? Kidney damage, tremors, seizures - serious side effects kick in. Cyclosporine levels are higher (100-200 ng/mL), but the margin for error is just as tight. Both drugs are metabolized by the same liver enzyme, CYP3A4. That means grapefruit juice, certain antibiotics, or even a different generic version can change how fast your body breaks them down. One study found that switching between different generic tacrolimus brands led to a 30% drop in blood levels within two weeks - enough to trigger rejection in some patients.The Generic Switch: Savings vs. Risk
Brand-name Prograf (tacrolimus) used to cost $1,200-$1,500 a month. Now, generic versions run $300-$500. Neoral (cyclosporine) dropped from $800-$1,000 to $150-$300. That’s huge for people on Medicare Part D or with high-deductible plans. In the U.S., over 92% of prescriptions for both drugs are now generic. But here’s what insurers don’t always tell you: not all generics are created equal. There are 14 FDA-approved generic tacrolimus products from eight different manufacturers. Eleven generic cyclosporine versions exist. Each uses different fillers, binders, and manufacturing processes. The FDA requires generics to be bioequivalent - meaning their absorption must fall within 80-125% of the brand. Sounds fine, right? Except that range is huge for a drug where 1 ng/mL can mean the difference between survival and failure. Real-world data shows the problem. A 2022 survey of 1,247 transplant patients found 42.7% noticed new side effects after switching to generic tacrolimus. Nearly one in five (18.3%) had to get their blood levels adjusted. On patient forums, stories are common: “My levels crashed after switching to the new generic.” “I got hospitalized for rejection after my pharmacy changed the brand.” “My nephrologist won’t let me switch because the last one messed me up.”What Happens When You Switch
Most transplant centers now have strict protocols when a patient switches from one generic to another - or from brand to generic. It’s not a simple refill change. Here’s what typically happens:- Before the switch, your doctor checks your current blood level and records your dose.
- After switching, you get weekly blood tests for at least four weeks.
- If your level drops below target, your dose is increased - sometimes dramatically.
- If it spikes, you’re at risk for kidney damage or neurological issues.
- Once stable, you’re told to stick with that exact generic brand - no more changes.

Who’s Most at Risk?
Not everyone reacts the same way. Some patients switch from Prograf to a generic and never miss a beat. Others can’t tolerate any change. Factors that increase risk include:- Having a kidney transplant (more sensitive than heart or liver)
- Being a CYP3A5 expresser (a genetic trait that makes you metabolize tacrolimus faster)
- Taking other drugs that affect liver enzymes
- Having had prior rejection episodes
- Being on a complex regimen with multiple immunosuppressants
What Patients Can Do
If you’re on cyclosporine or tacrolimus, here’s how to protect yourself:- Ask your pharmacist which generic brand you’re getting. Write it down.
- Never switch brands without talking to your transplant team. Even if it’s “the same drug,” it’s not.
- Track your levels. Know your target range and when your next test is due.
- Avoid grapefruit and Seville oranges. They interfere with absorption.
- Take your dose at the same time every day. Even a two-hour shift can affect levels.
- Report changes. New tremors, headaches, nausea, or swelling? Tell your doctor immediately.
The Bigger Picture
The push for generics isn’t wrong. Transplant care is expensive. Without generics, many people couldn’t afford their meds. But the system is built on the assumption that all generics are interchangeable. For drugs like cyclosporine and tacrolimus, that assumption is dangerous. Regulators are starting to catch on. In February 2024, the European Medicines Agency updated its guidelines to require bioequivalence studies using actual transplant patients - not just healthy volunteers. That’s a big step. In the U.S., the FDA still relies on healthy person data. The American Society of Transplantation and the International Transplant Society both now warn against unnecessary switching. A new extended-release version of tacrolimus (LCP-tacrolimus) was approved in late 2023. It’s designed to smooth out blood level spikes and dips, making it less sensitive to formulation changes. It’s not a generic yet - and it’s expensive. But it points to the future: better formulations, not just cheaper ones.Final Thoughts
Generic cyclosporine and tacrolimus are essential tools. They’ve made transplant care accessible to more people than ever. But they’re not just cheaper versions of the same drug. They’re different medicines with different absorption profiles. Treating them as interchangeable is like swapping out tires on a race car - even if they’re the same size, the tread, rubber compound, and balance matter. If you’re on one of these drugs, know your brand. Know your levels. And don’t let a pharmacy change your medication without your doctor’s say-so. Your organ depends on it.Can I switch between different generic versions of tacrolimus safely?
No - not without close medical supervision. Switching between different generic tacrolimus brands can cause dangerous drops or spikes in blood levels, even if they’re all FDA-approved. Studies show up to 30% variability in drug concentration after a switch. Always consult your transplant team before changing brands. Most centers now recommend sticking to one generic manufacturer once you’re stable.
Why is tacrolimus more sensitive than cyclosporine to generic changes?
Tacrolimus has a much narrower therapeutic window - its effective blood levels (5-15 ng/mL) are far lower than cyclosporine’s (100-200 ng/mL). Small changes in absorption that might be harmless with cyclosporine can push tacrolimus levels out of the safe range. Also, tacrolimus is absorbed more inconsistently across different formulations, making it more vulnerable to minor ingredient changes in generics.
How often should blood levels be checked after switching to a generic?
Weekly blood tests are recommended for the first four to six weeks after switching. Some centers extend monitoring to eight weeks if levels are unstable. Once stable, testing usually returns to every 1-3 months. Never assume your levels are fine just because you feel okay - rejection can happen without symptoms.
Are there any generics that are considered safer than others?
There’s no official list of “safer” generics. However, some transplant centers report more consistent results with certain manufacturers - often because they’ve tested them internally. The key isn’t the brand name, but consistency: once you find a generic that works for you, stick with it. Don’t switch unless absolutely necessary.
What should I do if my insurance forces me to switch to a different generic?
Ask your transplant team to write a letter of medical necessity explaining why switching could be dangerous. Many insurers will approve a brand-name or specific generic if there’s documented instability. If denied, contact patient advocacy groups like the National Transplant Insurance Assistance Fund - they help patients appeal these decisions. Never switch without monitoring - your life depends on stable drug levels.
Can I take cyclosporine and tacrolimus interchangeably?
No. While both are calcineurin inhibitors, they’re not interchangeable. Tacrolimus is far more potent - a 5 mg dose of tacrolimus is roughly equivalent to 150 mg of cyclosporine. Switching between them requires complete recalibration of your entire immunosuppression plan. This should only be done under strict supervision by a transplant specialist.






jefferson fernandes
Look, I get the cost savings - but this isn’t just about pills. It’s about survival. I’ve seen two friends lose their transplants because a pharmacy swapped their tacrolimus brand without telling them. One ended up back on dialysis. The other? Dead. The FDA’s 80-125% bioequivalence range is a joke when you’re talking about drugs where 1 ng/mL can kill you. We need mandatory patient notification before any switch - not just for doctors, but for the people actually taking these drugs.
Angel Molano
Stop pretending generics are dangerous. If your body can’t handle a switch, you’re not stable enough to be out of the hospital.
Kimberly Mitchell
The systemic failure here is not the generics - it’s the lack of standardized pharmacokinetic labeling across manufacturers. The FDA’s current paradigm is rooted in 1980s bioavailability models that ignore inter-individual variability in CYP3A4/5 expression. Until we mandate pharmacogenomic-aware bioequivalence testing - not just in healthy volunteers, but in transplant cohorts - we’re gambling with lives under the guise of cost containment.
Diana Campos Ortiz
I switched from Prograf to a generic last year and my levels stayed perfect. But I also got tested for CYP3A5 and my doc locked me into one brand. I’m not saying all generics are bad - just don’t switch without testing and tracking. And please, stop letting pharmacies change your meds without asking.
lucy cooke
Ah, the great American paradox: we’ll spend $100,000 on a transplant, then haggle over $300 for the drug that keeps it alive. We’ve turned medicine into a commodity, stripped of nuance, stripped of reverence. These aren’t aspirin. They’re the fragile thread holding life together - and we’re cutting it with a blunt knife labeled ‘cost-efficiency.’ The tragedy isn’t the drug switch - it’s that we’ve stopped seeing patients as people, and started seeing them as data points in a balance sheet.
Trevor Davis
Hey, I’m a transplant recipient too - 8 years post-kidney. I’ve been on the same generic for 5 years now. No issues. But I know people who’ve had nightmares. The key? Consistency. Once you find a brand that works? Never switch. And if your insurance tries to force you? Push back. Hard. Your doc should write a letter - and if they won’t, find one who will. This isn’t just about money. It’s about not dying.
John Tran
Okay so like, I read this whole thing and I’m just sitting here thinking - why are we even letting this happen? Like, if you’re on a drug that’s literally a razor’s edge between life and death, why does the FDA even allow multiple generics? It’s like letting 14 different companies make the same bullet for a sniper rifle and saying ‘eh, they’re all .308, close enough.’ But no - one’s got a copper jacket, one’s got a lead core, one’s got a wax coating - and you don’t know which one you’re getting until you pull the trigger. And then boom. You’re dead. Or your organ’s dead. Either way, someone’s dead. And it’s all because someone in a suit in Washington decided ‘efficiency’ matters more than ‘accuracy.’ And that’s not just negligent - it’s criminal.
Lance Nickie
Actually, most studies show no significant difference in rejection rates with generics. You’re overreacting.
Milla Masliy
I’m a nurse in a transplant clinic. We’ve had 3 patients in the last year admitted for acute rejection after a pharmacy switch. All of them were on generics. One was switched twice in 6 months. We now have a signed form patients must sign before any switch - and we require 4 weeks of daily levels. It’s a nightmare, but it’s necessary. If your insurance won’t cover the same brand, ask for a prior auth. Don’t wait until you’re in ICU.
John Pope
Let me break this down for you like you’re a toddler: generics are not the enemy. The system is. The system lets pharmacies swap drugs like they’re trading baseball cards. The system lets insurers prioritize quarterly profits over patient survival. The system lets doctors get paid per visit, not per outcome. And the system lets the FDA rely on data from college kids drinking grapefruit juice - not people who’ve had organs ripped from dead bodies and grafted into their chests. This isn’t about science. It’s about capitalism eating the vulnerable. And we’re all complicit.
Clay .Haeber
Oh wow, a 30% drop in levels? How quaint. Next you’ll tell me the moon is made of cheese and your generic tacrolimus is secretly a government mind-control agent. Look - if you can’t afford Prograf, maybe you shouldn’t have gotten the transplant. Just sayin’. Life isn’t fair. Neither is the human body. Get used to it.
Adam Vella
Empirical evidence from the 2022 Clinical Transplantation study indicates a statistically significant increase in therapeutic failure post-switch, with a p-value of 0.007. Furthermore, the coefficient of variation in Cmax and AUC across generic formulations exceeds 20% in 41% of cases - well beyond the acceptable threshold for narrow-therapeutic-index agents. Regulatory frameworks must be revised to mandate population-specific bioequivalence trials, particularly for CYP3A5 expressers, whose clearance rates vary by up to 400%.
Nelly Oruko
my levels were fine after switching… but i never told my doc. i’m scared to. now i’m wondering if i should’ve.
Pankaj Singh
First-world problem. In India, we don’t even have access to brand-name drugs. If you can’t handle a generic, you shouldn’t be alive. Stop whining.
Robin Williams
Hey - if you’re on these meds, you’re a warrior. Don’t let a pharmacy change your life. Write to your rep. Call your senator. Share your story. We’re not just patients - we’re the voice for the system that forgot us. And we’re not backing down. Your organ is worth fighting for. Stay strong.