Birth Control Safety Checker
Check Your Birth Control Safety
This tool helps you determine if your HIV medication and birth control method combination is safe. Based on CDC and WHO guidelines, select your HIV treatment and birth control method to see if they're compatible.
When you're taking HIV protease inhibitors to manage your virus, you might not realize that your birth control could be working less effectively - even if you're taking it exactly as directed. This isn't a myth, a rumor, or something you might have heard on the internet. It's a well-documented, clinically significant drug interaction that has led to unplanned pregnancies in real people, even when both medications were taken perfectly.
Why This Happens: The Science Behind the Interaction
HIV protease inhibitors like lopinavir, atazanavir, and darunavir - especially when boosted with ritonavir or cobicistat - interfere with how your body processes hormones in birth control. These drugs are metabolized by the same liver enzymes (CYP3A4) that break down estrogen and progestin. When protease inhibitors block or alter these enzymes, hormone levels in your blood can drop too low to prevent ovulation or thicken cervical mucus - the two main ways hormonal birth control stops pregnancy. The effect isn't the same across all methods. Combined oral contraceptives (COCs) like Tri-Sprintec or Yaz can see ethinyl estradiol levels drop by up to 45% when taken with lopinavir/ritonavir. The contraceptive patch and ring aren't safer - in fact, studies show the ring can drop to subtherapeutic levels in nearly 4 out of 10 women on efavirenz-based regimens. Even progestin-only pills (the "mini-pill") are affected: the World Health Organization classifies them as Category 3 when used with ritonavir-boosted PIs, meaning the risks usually outweigh the benefits.Which Birth Control Methods Are Riskiest?
Not all hormonal birth control is equally affected. Here’s what the data shows:- Combined oral contraceptives (COCs): Highest risk. Pregnancy rates jump from the typical 7-8% failure rate to 11-15% when taken with efavirenz, and up to 14% with ritonavir-boosted PIs.
- Contraceptive patch and ring: Hormone levels drop sharply. The ring’s etonogestrel can fall below the level needed to prevent ovulation.
- Progestin-only pills (POPs): Not recommended with ritonavir-boosted regimens. Even small missed doses can lead to ovulation.
- Depo-Provera (DMPA): Mixed results. Some studies show no significant drop in hormone levels, but pregnancy rates are still higher than in women not on antiretrovirals - especially with efavirenz.
- Implants (etonogestrel): Dangerous with ritonavir-boosted PIs. Studies show 40-60% reduction in hormone levels. The International AIDS Society-USA advises against this combination.
The bottom line? If you're on a protease inhibitor - especially lopinavir/ritonavir, atazanavir/ritonavir, or darunavir/cobicistat - your hormonal birth control might not be enough.
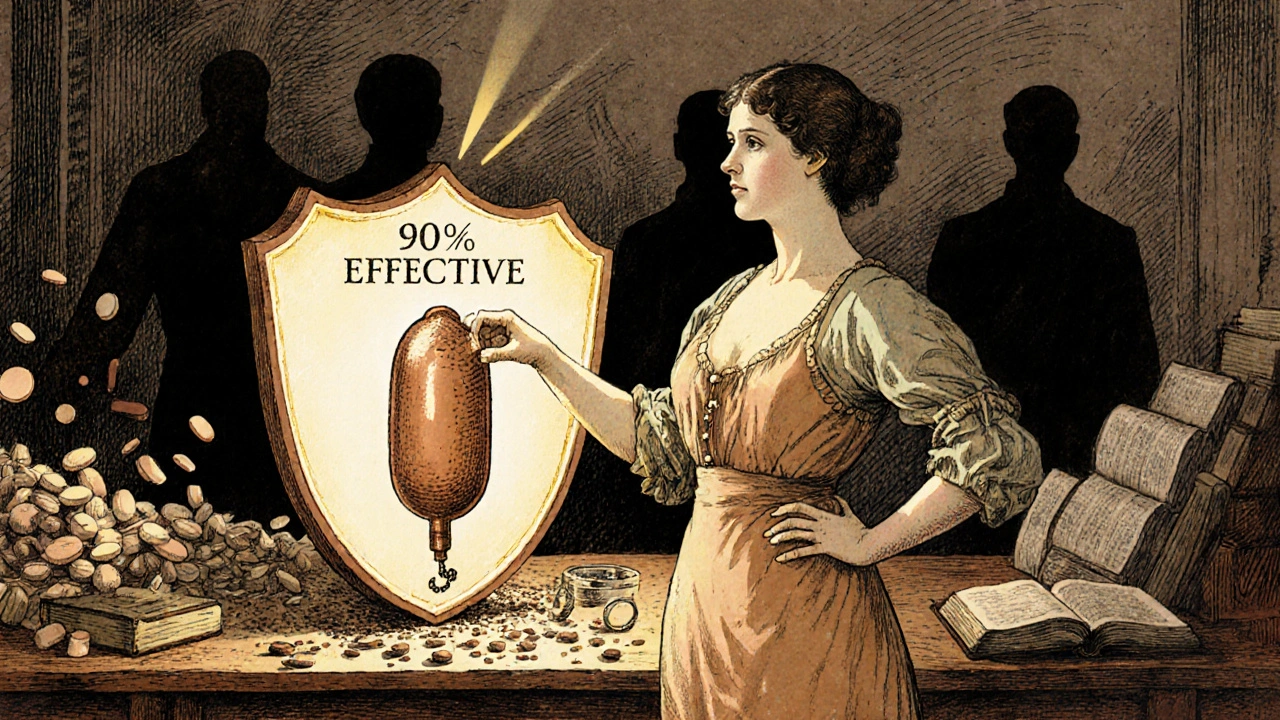
What Works? The Only Safe Options
There’s good news: some methods work just as well regardless of your HIV meds.- Copper IUD: 99% effective. No hormones. No interaction. Lasts up to 12 years.
- Hormonal IUD (levonorgestrel): Also 99% effective. Studies show no meaningful drop in hormone levels even with efavirenz or boosted PIs. The NIH-funded NEXT-Study is confirming this across 15 countries.
- Implants with dolutegravir: New data from 2023 WHO guidelines suggest etonogestrel implants are now safe with dolutegravir-based regimens, which are now the first-line treatment for most new HIV patients.
These are called long-acting reversible contraceptives (LARCs). They’re the gold standard for women on HIV treatment. They don’t require daily pills, patches, or injections. Once placed, they work for years. And they’re not affected by your antiretrovirals.
Real Stories, Real Consequences
Behind the statistics are real women who didn’t know this risk existed. One woman on Reddit shared that she became pregnant at 18 weeks while using Depo-Provera with atazanavir/ritonavir. Her provider told her the interaction was "well-documented but often overlooked." Another woman on HIV.gov forums got pregnant on Tri-Sprintec while taking darunavir/cobicistat - despite perfect adherence. In a 2021 survey of 327 HIV-positive women, nearly 1 in 4 reported contraceptive failure, and 63% of those cases involved protease inhibitors. Worse, many women weren’t warned. A 2018 report from the AIDS Clinical Trials Group found that 41% of women received no counseling about these interactions during their HIV diagnosis. Community clinics were even worse - 28% less likely to offer proper guidance than academic medical centers. Some women have made heartbreaking choices: discontinuing their HIV meds to keep using birth control. That’s not a solution - it puts their health and life at risk. Viral rebound can happen fast.What Providers Should Do
Doctors and nurses need to talk about this - not just once, but every time a woman with HIV discusses birth control. The CDC recommends a 7-10 minute conversation using their free online interaction checker, which lists 147 drug pairs. The American College of Obstetricians and Gynecologists (ACOG) suggests the "teach-back" method: ask the patient to explain the plan in their own words. Studies show 85% of women understand their options this way, compared to just 42% with standard counseling. In high-income countries, 79% of academic centers have formal protocols for this. In community clinics? Only 34%. That gap is deadly.
What You Should Do Right Now
If you're on HIV treatment and using hormonal birth control:- Check your regimen. Are you taking lopinavir, atazanavir, darunavir, or any drug boosted with ritonavir or cobicistat? If yes, your birth control might not be working.
- Don’t stop your HIV meds. That’s dangerous.
- Ask your provider: "Is my birth control safe with my HIV drugs?" Show them your pill bottle or patch.
- Request a copper or hormonal IUD. They’re safe, effective, and long-lasting.
- If you’re on dolutegravir or raltegravir, your risk is much lower - but still confirm with your provider.
Don’t wait for your next appointment. If your provider says, "It’s fine," ask for the CDC’s interaction checker or the WHO Medical Eligibility Criteria. You have the right to know.
The Bigger Picture
The good news? The tide is turning. Dolutegravir-based regimens are now used by 72% of new HIV patients - and they don’t interfere with birth control like protease inhibitors do. By 2030, integrated clinics that offer HIV care and contraception in one visit could reduce contraceptive failures by more than half. But until then, this gap in care is costing women their reproductive autonomy. The science is clear. The tools exist. What’s missing is consistent, urgent communication between providers and patients.If you're on HIV treatment, your birth control shouldn't be a gamble. You deserve to control your body - and your future.
Can I still use the pill if I’m on HIV protease inhibitors?
No - not reliably. Combined oral contraceptives and progestin-only pills are significantly less effective when taken with ritonavir-boosted protease inhibitors like lopinavir/ritonavir or darunavir/cobicistat. Even perfect adherence won’t prevent the drop in hormone levels. The WHO and CDC recommend avoiding these combinations entirely.
Is the birth control shot (Depo-Provera) safe with HIV meds?
It’s complicated. With non-ritonavir-boosted regimens like dolutegravir or nevirapine, Depo-Provera is considered safe (WHO Category 1). But with efavirenz or ritonavir-boosted PIs, studies show higher pregnancy rates - up to 12.3 per 100 woman-years. It’s not banned, but it’s not the best choice. IUDs or implants are safer.
What about the IUD? Will my HIV meds affect it?
No. Both the copper IUD and hormonal IUD (like Mirena or Kyleena) remain 99% effective regardless of your HIV treatment. Studies show no clinically significant drop in hormone levels from the IUD, even with boosted protease inhibitors. They’re the most reliable option for women on antiretrovirals.
Can I use emergency contraception if I’m on HIV protease inhibitors?
Levonorgestrel (Plan B) may be less effective because protease inhibitors can lower its levels. The CDC recommends ulipristal acetate (Ella) instead, or a copper IUD inserted within 5 days - which is the most effective emergency option and also provides ongoing contraception.
Why don’t more doctors know about this?
Many providers, especially in community clinics, haven’t been trained on these interactions. A 2018 report found 41% of HIV-positive women received no counseling about birth control risks at diagnosis. Even today, community health centers are 28% less likely to provide this info than academic hospitals. The CDC offers a free 2-hour online course - but only 8,214 providers have taken it so far.
Are newer HIV drugs safer for birth control?
Yes. Dolutegravir and raltegravir (integrase inhibitors) have minimal interaction with hormonal contraceptives. In fact, WHO now classifies etonogestrel implants as safe with dolutegravir. These are now the first-line HIV treatment for most new patients - so if you’re on one of these, your risk is very low. Still, always confirm with your provider.
What should I do if I got pregnant while on HIV meds and birth control?
You’re not alone - this happens more often than people admit. Talk to your HIV provider and OB-GYN immediately. They can help you adjust your HIV treatment plan safely during pregnancy and connect you with support services. Don’t blame yourself - this is a known medical issue, not a personal failure.






Scott Horvath
bro i just found out my cousin got pregnant on depo while on atazanavir and no one told her until she was 16 weeks 😭 this needs to be screamed from the rooftops
Kimberly Ford
this is exactly why i started pushing all my patients toward iuds. no pills to forget, no patches to fall off, and zero interaction with any antiretrovirals. copper or hormonal, doesn't matter. they're the only real win here. 🩺
Kshitij Nim
in india we dont even have access to iuds in most rural clinics. women are given pills and told 'take it daily' while on boosted pIs. its a disaster waiting to happen. we need mobile health teams trained on this.
jennifer sizemore
i had no idea this was even a thing until my friend got pregnant. i cried for her. how is this not standard counseling? we're talking about people's bodies and futures here. it's not just medical, it's ethical.
jerry woo
the system is broken. providers are overworked, undertrained, and frankly, lazy. you think some clinic nurse in rural kentucky is gonna pull up the CDC interaction checker? nah. they'll say 'it's fine' and move on to the next patient. this isn't negligence-it's systemic abandonment.
Armando Rodriguez
as a healthcare professional, i can confirm: the data is unequivocal. protease inhibitors significantly reduce hormonal contraceptive efficacy. the gold standard remains LARCs-copper and levonorgestrel IUDs. every patient on boosted PIs deserves a dedicated 10-minute counseling session using CDC tools. this is not optional-it's standard of care.
Kevin Ouellette
just got my hormonal iud installed last week 🥹 thank god i read this thread. my doc didn't mention any of this. now i feel like a superhero with my little plastic wand. 🦸♀️💊 #NoMorePills
Patrick Ezebube
this is all a big pharma scam. they want you on iuds because they make more money. the real cause of pregnancy is the ritonavir booster being a toxin that messes with your hormones. the government knows. they just don't care. look at the numbers-34% of clinics don't even warn you. that's intentional.
matt tricarico
interesting how the post assumes all women are rational actors who can advocate for themselves. what about the 18-year-old undocumented immigrant who doesn't speak english and is terrified of her provider? this 'you have the right to know' rhetoric is laughable. systemic change isn't achieved by telling people to ask questions.