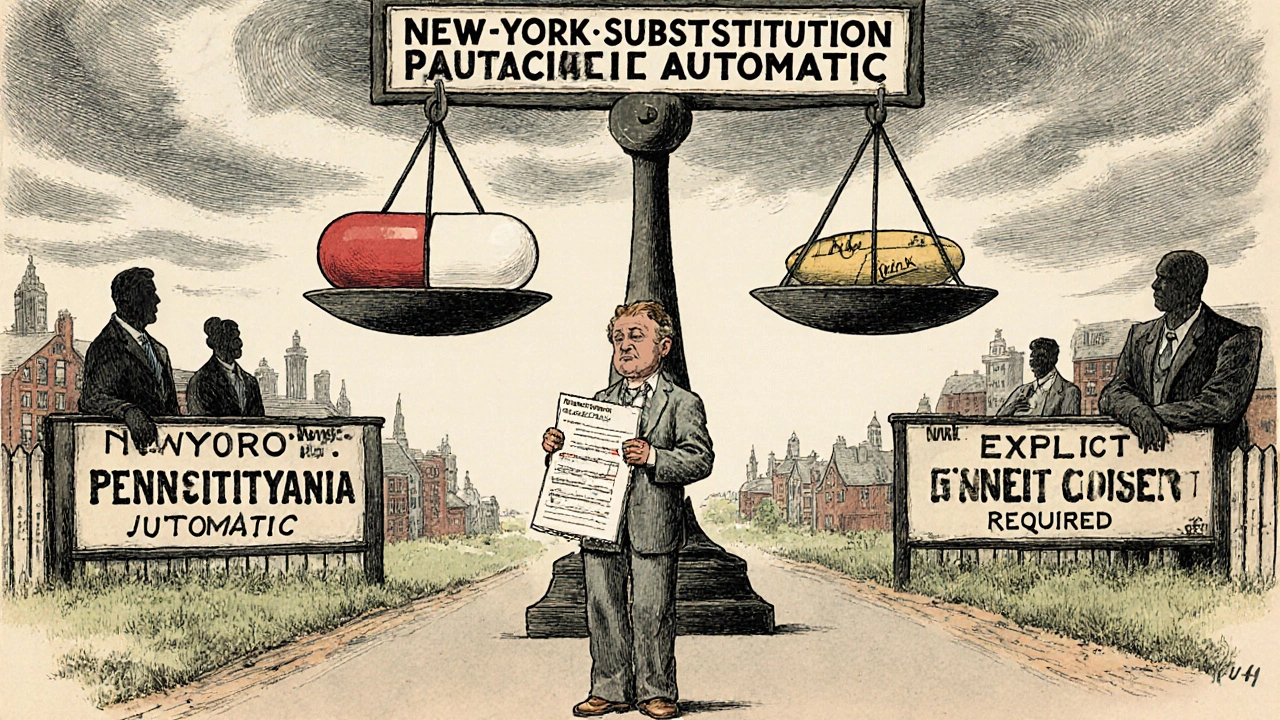
When you pick up a prescription, you might not think twice about getting a generic pill instead of the brand-name one. But behind that simple swap is a tangled web of state laws that vary wildly from one corner of the country to the next. What’s allowed in Texas might be illegal in Hawaii. What’s automatic in New York requires your explicit okay in Pennsylvania. These aren’t just bureaucratic details-they directly affect your health, your wallet, and your trust in the pharmacy system.
How Generic Substitution Works (And Why It Matters)
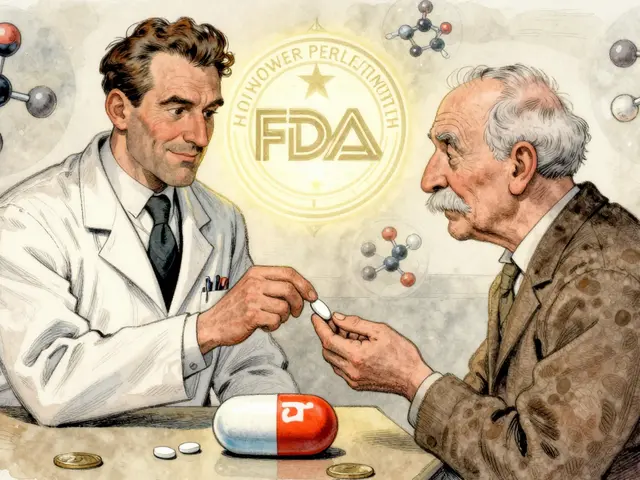
The idea behind generic substitution is straightforward: if a drug’s patent expires, other companies can make the same medicine at a fraction of the cost. The FDA says these generics are therapeutically equivalent-they contain the same active ingredient, in the same strength, and work the same way. That’s why 92.5% of all prescriptions filled in the U.S. are for generics, saving patients and insurers over $313 billion a year.
But here’s the catch: not all drugs are created equal. Some, called narrow therapeutic index (NTI) drugs, have very little room for error. A tiny difference in how much of the drug gets into your bloodstream can mean the difference between treatment and danger. Warfarin, levothyroxine, and certain seizure meds fall into this category. Even if the FDA says two versions are equivalent, some patients report feeling different after a switch. That’s why states stepped in to add their own rules.
The Four Big Ways States Differ
State laws on generic substitution aren’t just slightly different-they’re built on four key choices that change how and when a pharmacist can swap a brand for a generic.
- Must they substitute? In 22 states, pharmacists are legally required to substitute generics unless the doctor or patient says no. In the other 28 states and D.C., substitution is optional. That means in some places, you’ll get the generic by default. In others, you have to ask for it.
- Do you have to say yes? Thirty-two states use presumed consent: if you don’t say no, the pharmacist swaps the drug. Eighteen states require you to give explicit permission before the switch happens. That might sound fairer, but it also means more paperwork, more delays, and more confusion.
- Do you get notified? Forty-one states require pharmacists to tell you after the substitution happens-usually on the label or through a printed notice. But in nine states, you might never know you got a different pill unless you check the bottle yourself.
- Who’s liable if something goes wrong? Thirty-seven states protect pharmacists from lawsuits if they follow the rules. That means if you have a bad reaction after a generic swap, the pharmacist isn’t automatically on the hook-unless they broke the law.
Where the Rules Get Weird
Some states have rules that seem out of step with the rest. Oklahoma, for example, bans substitution unless the prescriber or the person paying for the drug gives permission. That’s rare. Hawaii is even more restrictive: for antiepileptic drugs, you need both your doctor’s approval and your own written consent before a generic can be given. That’s not just caution-it’s a major barrier to cost savings.
Then there’s Louisiana, which scores 0 on a state favorability scale (the lowest possible score), meaning its rules make substitution as easy as possible. Meanwhile, Hawaii scores a 4-the highest, meaning it’s the hardest place to swap generics. These differences aren’t random. They reflect political priorities, lobbying by drug companies, and varying levels of public concern about safety.
Biosimilars: The New Frontier
It’s not just small-molecule generics anymore. Biosimilars-copies of complex biologic drugs used for cancer, arthritis, and autoimmune diseases-are now entering the market. As of 2023, 49 states and D.C. have laws covering biosimilar substitution. But the rules are even messier here.
Florida requires pharmacies to create a formulary that ensures substitutions won’t threaten patient safety. Iowa tells pharmacists to stick with the FDA’s Orange Book. And in 12 states, new laws now align with the FDA’s 2020 designation of “interchangeable” biosimilars-meaning they can be swapped without a doctor’s input, just like regular generics. But not all biosimilars are labeled interchangeable. And not all states agree on what that means.
What Happens When Rules Clash
Imagine you live in New Jersey but work in New York. Your prescription is filled in New York, where substitution is automatic. But your insurance plan is based in New Jersey, where you have to give permission. Which law applies? The answer? It depends. Chain pharmacies use software that tries to sort this out, but errors still happen. One in five pharmacy transactions now involve prescriptions that cross state lines.
Patients often get confused. One Reddit user described how neighbors on either side of the New York-Pennsylvania border got different treatment for the same prescription. “I had to explain why I got a different pill yesterday,” she wrote. “It felt like I was being treated differently just because of my zip code.”
Real Risks, Real Stories
There’s data behind the fear. Between 2020 and 2022, the FDA received 217 reports of problems after generic substitution. Most involved levothyroxine (89 cases) and warfarin (53 cases). In Minnesota, a patient on warfarin had a dangerous bleed after switching generics-even though both versions were rated equivalent by the FDA. The patient’s INR levels jumped unexpectedly. The pharmacy followed all state rules. The doctor didn’t say “dispense as written.” No one broke the law. But the outcome was still dangerous.
Patients with rare diseases are especially vulnerable. The Life Raft Group found that 41% of cancer patients worry about substitution of NTI drugs. Nearly a third say their doctor specifically told them not to allow any switches. That’s not paranoia-it’s experience.
How Pharmacists Are Coping
Pharmacists are on the front lines. They’re expected to know the rules in 50 states, plus D.C. The average pharmacist spends nearly 13 minutes per prescription checking state laws, patient history, and formulary rules. That’s time taken away from counseling patients.
Most pharmacy schools now teach 45 to 60 hours on substitution laws. Licensing exams in 92% of states test this knowledge. And 83% of pharmacy management systems now have built-in tools that auto-check state rules and flag conflicts. These tools cut substitution errors by 64%, according to Drug Topics. But they’re not perfect. They can’t always account for handwritten notes on prescriptions or outdated patient preferences.
Who Wins and Who Loses
States with mandatory substitution and presumed consent see higher generic fill rates-up to 94% compared to 88% in permissive states. Medicaid programs save an estimated $1.2 billion a year because of these laws. Patients pay less. Insurers pay less. Taxpayers pay less.
But the cost isn’t just financial. There’s a psychological cost. Patients who feel they didn’t consent to a change lose trust. Pharmacists feel caught between legal obligations and patient care. Doctors get frustrated when their “dispense as written” instructions are ignored.
And then there’s the bigger question: Is this system sustainable? With 6 billion prescriptions filled every year, and with biosimilars set to explode in the next five years, the current patchwork is becoming unmanageable. The American Pharmacists Association says 78% of pharmacists are confused by state-by-state rules. The Uniform Law Commission is working on a model act to bring consistency. But change moves slowly.
What You Can Do
If you’re on a critical medication-especially warfarin, levothyroxine, or an antiepileptic drug-know your rights. Ask your pharmacist: “Is this a generic? Did you substitute it?” Check the label. If you feel different after a switch, tell your doctor. Keep a log of how you feel before and after any change.
If you’re not on a high-risk drug, you’re probably fine with substitution. But don’t assume it’s automatic. In some states, you have to ask. In others, you have to say no. Know your state’s rules. You can find them on your state board of pharmacy’s website.
And if you’re a caregiver or family member helping someone manage medications, speak up. Ask questions. Don’t let confusion become a safety risk.
What’s Next?
The future of generic substitution isn’t about banning it-it’s about making it smarter. The FDA is adding new therapeutic equivalence codes for biosimilars. States are updating laws to match. Some are moving toward uniform standards. Others are doubling down on local control.
One thing is clear: the system won’t stay this way forever. Either states will harmonize their rules-or the federal government will step in. Until then, the burden falls on you, the patient, to understand what’s in your bottle and why.






Johnson Abraham
lol so now we gotta be pharmacists too? 🤡 just give me the cheap pill and stop overcomplicating it. my insurance doesnt care if its brand or generic, why should i?
Shante Ajadeen
this is actually really helpful. i didnt realize how much it varied by state. my grandma switched to a generic levothyroxine last year and felt awful for weeks. she never knew it was swapped. i’m gonna check her bottle next time i visit.
dace yates
i’m curious-how many of these state laws were actually written by lobbyists from big pharma? the fact that Hawaii has the strictest rules but also the highest cost of living makes me think this isn’t about safety, it’s about profit.
Samantha Wade
The systemic fragmentation of pharmaceutical regulation across state lines represents a profound failure of intergovernmental coordination. Patients are being subjected to arbitrary, non-evidence-based disparities in care that directly compromise therapeutic outcomes. This is not merely inconvenient-it is ethically indefensible.
Nicole M
i just got my warfarin refill and the bottle looked different. i didn’t say anything because i assumed it was the same. now i’m scared. how do i even check if they swapped it?
Alex Ramos
yep, been a pharmacist for 12 years. we get 13 mins per script? more like 7 if you're busy. we use the software but half the time the script says 'dispense as written' but the system still auto-substitutes because the insurance says 'preferred'. it's a mess. if you're on warfarin or levothyroxine-just ask. always. no shame.
edgar popa
just ask for the brand if you wanna be safe. easy. no drama. 🤷♂️
Eve Miller
It is unconscionable that patients are being subjected to pharmaceutical roulette based on their ZIP code. This is not healthcare-it is a legal lottery. Every state that permits presumed consent without informed consent is complicit in medical negligence.
Chrisna Bronkhorst
usa you guys are wild. in south africa we just get what the pharmacy has. no forms no questions. if you feel weird go see doctor. simple. why make it so hard?