Every day, hospitals and clinics across the U.S. are making impossible choices. Beds are closed because there aren’t enough nurses to staff them. Emergency rooms stretch waits to 72 hours. Doctors are forced to skip lunch just to keep up. This isn’t a worst-case scenario-it’s today’s reality. The healthcare staffing shortage isn’t just a buzzword. It’s breaking the system, and patients are paying the price.
Why the Staffing Crisis Is Worse Than Ever
The problem didn’t start with the pandemic, but it sure made it explode. Before 2020, hospitals were already struggling to fill open nursing positions. By 2025, the gap has turned into a chasm. The Health Resources and Services Administration estimates more than 500,000 registered nurses will be missing by 2030. That’s not a projection-it’s a countdown. And it’s not just nurses. Primary care doctors, mental health providers, and even lab technicians are in short supply. One key reason? Burnout. Nurses are leaving the field at record rates. Nearly 63% say they’re thinking about quitting, according to the Medscape Nurse Compensation Report. Why? Unsafe patient loads. One ICU nurse in New York told a Reddit thread she was managing three critically ill patients at once-double the safe limit. She had two near-miss medication errors last month. That’s not negligence. That’s systemic failure.What Happens When There Aren’t Enough Nurses
It’s not just longer wait times. When nurse-to-patient ratios climb above 1:4, mortality rates jump by 7%, according to a 2022 JAMA study. That’s not a small number. It means more people die because there’s no one to catch the early signs of decline. Emergency departments are hit hardest. The American College of Emergency Physicians reports patients now wait 22% longer than they did in 2022. In rural Nevada, some patients wait three days just to be seen. Meanwhile, hospitals are closing inpatient beds-not because they’re empty, but because there’s no staff to run them. Mercy Health’s CEO said they’re losing $4.2 million a month just from bed closures. Even routine care suffers. Diabetic patients miss follow-ups. Post-surgery checks get delayed. Chronic conditions spiral out of control. The result? More people end up in the ER-not because they’re sicker, but because their care fell through the cracks.Rural Clinics Are Falling Behind
Urban hospitals can pay travel nurses $185 an hour to fill gaps. Rural clinics can’t. They’re stuck with 37% higher vacancy rates than city hospitals, according to the Rural Health Information Hub. Many have no full-time doctor on staff. Instead, they rely on part-time providers who drive in from neighboring towns. In places like eastern Kentucky or western Montana, clinics shut down entirely. Patients drive two hours just to get a prescription refill. Some skip care altogether. The consequences? Higher rates of uncontrolled hypertension, diabetes complications, and preventable hospitalizations. The gap isn’t just about staff-it’s about access.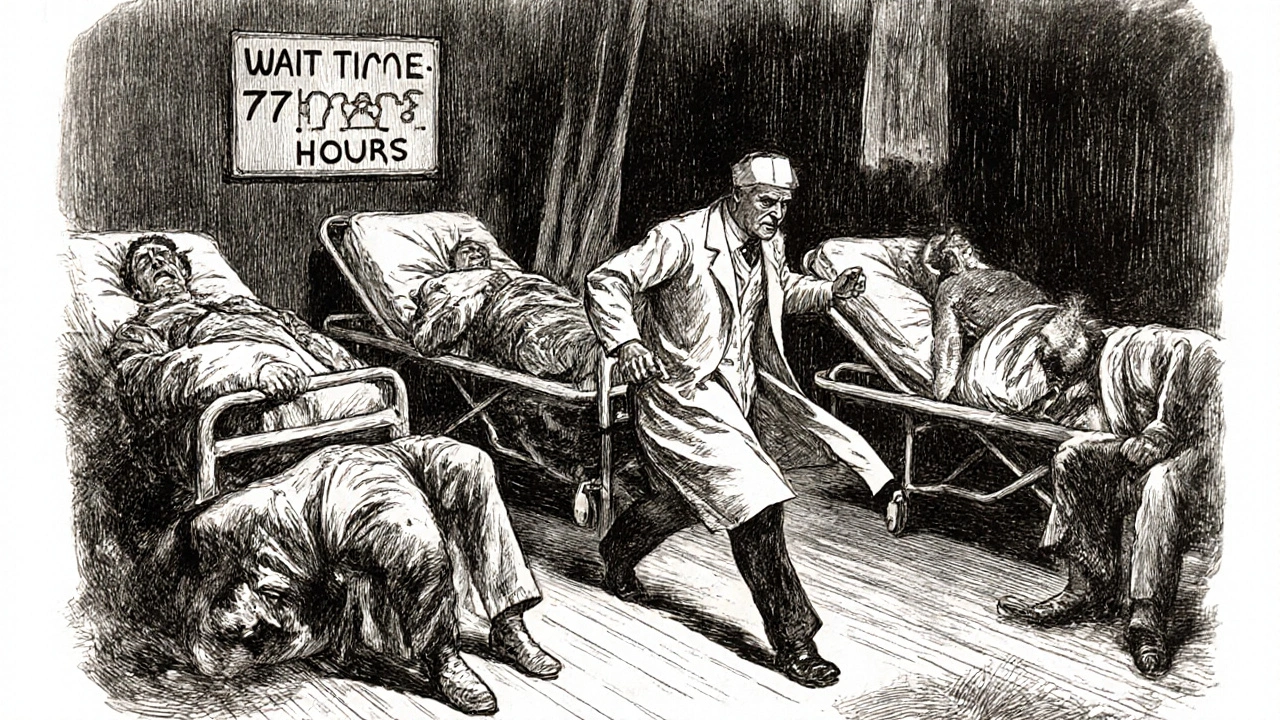
Behavioral Health Is in Free Fall
While everyone talks about nursing shortages, behavioral health is collapsing faster. The Department of Health and Human Services projects a deficit of 12,400 mental health professionals by 2025-up 37% from 2023. There are too few psychiatrists, too few therapists, too few crisis responders. Emergency rooms now serve as de facto mental health clinics. A patient having a panic attack waits 18 hours for a bed. A teen in crisis sleeps on a gurney because there’s no inpatient unit with space. This isn’t treatment. It’s storage. And it’s getting worse. Schools can’t refer students to counselors. Families can’t find therapists who take insurance. The system is so backed up that even people with insurance are told, “We can’t help you until next year.”Why Temporary Fixes Are Failing
Hospitals have tried quick fixes. Travel nurses. Mandatory overtime. Cross-training staff. None of it works long-term. Travel nurses filled 12% of hospital roles in 2023-but they cost 34% more. That’s not sustainable. Hospitals are spending millions just to keep the lights on. Meanwhile, permanent staff see their coworkers earning triple their pay, creating resentment and more turnover. Mandatory overtime is another disaster. Forty-one percent of hospitals now require staff to work extra shifts at least twice a week. That’s not a bonus-it’s a survival tactic. And it’s burning people out faster. One nurse on LinkedIn wrote: “I’ve worked 16-hour days for 11 straight weeks. I’m not a robot. I’m not a machine. I’m just tired.”
What’s Really Needed: Long-Term Solutions
The answer isn’t more Band-Aids. It’s rebuilding the system. First: invest in education. The American Association of Colleges of Nursing says 2,305 qualified nursing applicants were turned away in 2023-because there weren’t enough faculty to teach them. The federal government spends $247 million a year on nursing education. Experts say it needs $1.2 billion. That’s a gap of nearly $1 billion. Second: fix licensing. Right now, a nurse licensed in Texas can’t easily work in Oklahoma. The process takes 112 days on average. That’s absurd. States need to adopt compact licenses so providers can move where they’re needed most. Third: use technology wisely. AI tools can cut documentation time by half. Remote monitoring can catch problems before they become emergencies. But these tools require training. And money. And time. Most clinics don’t have any of those. And fourth: treat staff like humans. Magnet hospitals-those recognized for excellence in nursing-provide 4.2 hours of professional development per nurse each month. Non-Magnet hospitals? Just 1.1 hours. The difference? Turnover is 31% lower at Magnet facilities. People stay when they feel valued.What’s Next? The Clock Is Ticking
The U.S. population is aging fast. By 2050, there will be 82 million Americans over 65. That’s nearly double today’s number. But the number of working-age people to support them? It’s falling-from four workers per senior today to 2.9 by 2030. Without major changes, the healthcare system won’t just be strained. It will collapse. More hospitals will close. More clinics will shut down. More people will die because care was just out of reach. The Biden administration’s $500 million investment in nursing education sounds big-but it covers only 18% of what’s needed. The American Hospital Association’s new workforce initiative aims to train 50,000 new workers. That’s a start. But it’s not enough. The truth? We’ve known about this crisis for years. We’ve had the data. We’ve had the experts. What we’ve lacked is the political will to act before it was too late. Now, we’re not just preparing for the future. We’re living it.Why are hospitals closing beds if they’re empty?
Hospitals close beds not because they’re unused, but because they don’t have enough nurses or other staff to safely care for patients in them. A bed without a nurse isn’t just empty-it’s dangerous. If a patient codes, has a fall, or needs urgent meds, there’s no one to respond. Closing beds is a last-resort safety measure.
Are travel nurses making the shortage worse?
Not directly, but they’re making the problem harder to solve. Travel nurses fill critical gaps, especially in rural areas. But they’re paid 2-3 times more than permanent staff, which creates resentment and makes it harder to retain local nurses. Hospitals end up spending more money on temporary help instead of fixing the root causes like pay, workload, and burnout.
Can telehealth fix the staffing shortage?
Telehealth helps, but it’s not a cure. Nurse triage via telehealth reduced ER visits by 19% in pilot programs. But it requires tech infrastructure, training, and reliable internet-things many rural clinics lack. It also doesn’t replace hands-on care for emergencies, surgeries, or chronic disease management. It’s a tool, not a replacement.
Why don’t more people become nurses if there’s such high demand?
Because the job is exhausting, underpaid, and emotionally draining. Nursing schools turn away thousands of applicants each year due to lack of faculty and clinical placements. Even those who graduate face 12-hour shifts, constant stress, and unsafe patient ratios. Many leave within five years. The dream of helping people clashes with the reality of being overworked and under-supported.
What can patients do to help?
Patients can advocate for better staffing policies by contacting their state representatives and supporting legislation that mandates safe nurse-to-patient ratios. They can also choose hospitals with Magnet recognition, which indicates better staffing and patient outcomes. And they can show appreciation to frontline workers-small gestures matter when morale is low.




Alex Boozan
The entire healthcare system is a bloated, inefficient mess because we’ve been prioritizing bureaucracy over bedside care for decades. We keep throwing money at travel nurses while ignoring the root cause: we’ve turned nursing into a soul-crushing assembly line. The government spends billions on electronic health records nobody uses properly, but won’t fund more nursing faculty. This isn’t a shortage-it’s a failure of political will. We need to stop treating healthcare like a tech startup and start treating it like a public good.
mithun mohanta
OMG, this is literally the same in India!! But here, we don’t even have *beds*-let alone nurses!! I saw a guy in Delhi waiting 48 hours for a CT scan because the radiologist was on strike!! And don’t get me started on the “private hospitals” charging $500 for a simple IV drip!! The system is a joke!! 😭😭😭
Evan Brady
Let’s be real: the problem isn’t just numbers-it’s dignity. Nurses used to be trusted professionals. Now they’re glorified order-takers with 100 patients on their screen and zero autonomy. I worked in a rural clinic for five years. We had one RN for 12,000 people. We used WhatsApp to triage chest pain. That’s not innovation-that’s desperation. We need to stop romanticizing ‘resilience’ and start paying people enough to not quit.
Ram tech
lol nurses get paid too much anyway. if they were smart theyd go into tech. also why do we even need so many hospitals? maybe people just need to stop getting sick? also telehealth is the future. why pay for beds when you can zoom?
Jenny Lee
My mom got discharged early because they ran out of nurses. She had a catheter still in. I’m not mad. I’m just… tired.
Erica Lundy
The structural collapse of healthcare is not merely an economic or logistical failure-it is a metaphysical one. We have commodified care to the point where the human element is treated as an ancillary variable, rather than the central axiom. The nurse, once the embodiment of compassionate stewardship, is now a labor unit in a cost-benefit algorithm. The tragedy is not that we lack staff-it is that we have forgotten why we ever needed them.
Kevin Jones
They’re closing beds because the system’s already dead. You can’t staff a corpse. The real crisis? We’ve normalized this. We scroll past ER wait times like they’re TikTok trends. We cheer for ‘hero nurses’ while refusing to fund their pay raises. This isn’t a shortage-it’s a funeral procession, and we’re all holding the flowers.
Premanka Goswami
Wake up. This isn’t about nurses. It’s about the deep state using healthcare collapse to push universal digital ID cards. Every time a hospital closes, it’s a step toward centralized health control. The ‘staffing shortage’? A distraction. The real agenda? Mandatory biometric tracking. They want you dependent. They want you afraid. They want you to beg for a nurse who doesn’t exist. Look at the funding-where’s the money going? Not to training. To data brokers.
Alexis Paredes Gallego
Of course the system’s collapsing. The same people who let Big Pharma raise insulin prices 500% in 10 years are now crying about ‘staff shortages.’ They don’t want to fix it-they want to profit from the chaos. Travel nurses? A scam. They’re paid $200/hr so hospitals can claim they’re ‘doing something’ while the real staff starve. And don’t even get me started on how the AMA and AHA are just front groups for insurance CEOs.
Saket Sharma
Stop blaming politicians. The real issue? Nursing schools are too lenient. Anyone can get in. No standards. No discipline. That’s why we have so many burnt-out nurses-they weren’t trained to handle pressure. Cut enrollment by 50%. Raise admission standards. Make them work 2 years in rural clinics before licensing. No more coddling. Discipline creates excellence.
Alex Boozan
Wow. So your solution is to make nursing even more brutal? You’re not fixing the system-you’re just making it crueler. The real problem isn’t that nurses are soft-it’s that we treat them like disposable parts. You want discipline? Fine. But first, pay them $100k with benefits, cap their patient loads, and give them mental health days. Otherwise, you’re just screaming into the void while the hospital burns.