Understanding Sleep Apnea and Its Effects on the Heart
Sleep apnea is a common sleep disorder that affects millions of people worldwide. It is characterized by pauses in breathing or shallow breaths during sleep, causing the individual to awaken frequently throughout the night. These disruptions in sleep can have a significant impact on a person's overall health, including their heart health. In this article, we will explore the link between sleep apnea and heart rhythm disorders, and how addressing these issues can improve both conditions.
Types of Sleep Apnea and Their Influence on Heart Rhythms
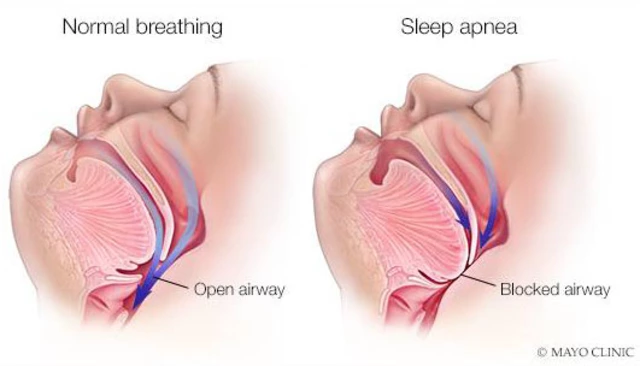
There are two main types of sleep apnea: obstructive sleep apnea (OSA) and central sleep apnea (CSA). OSA is the most common form and occurs when the muscles in the throat relax during sleep, causing a blockage of the airway. CSA, on the other hand, occurs when the brain fails to send the proper signals to the muscles responsible for controlling breathing. Both types of sleep apnea can lead to interrupted sleep patterns and decreased oxygen levels in the blood, which can have a negative impact on heart health.
Low oxygen levels in the blood can cause the heart to work harder to pump oxygen-rich blood throughout the body. This increased workload can lead to an irregular heartbeat, or arrhythmia, which is a common heart rhythm disorder. Additionally, the frequent awakenings associated with sleep apnea can cause an increase in stress hormones, which can further exacerbate heart problems.
Increased Risk of Atrial Fibrillation
Atrial fibrillation (AFib) is a common heart rhythm disorder characterized by a rapid, irregular heartbeat. Research has shown that individuals with sleep apnea are at an increased risk of developing AFib. This is because sleep apnea can cause fluctuations in blood pressure and oxygen levels, which can trigger irregular electrical signals in the heart. Additionally, the stress hormones released during sleep apnea episodes can also contribute to AFib development.
Managing sleep apnea through treatment can help reduce the risk of AFib and improve overall heart health. In some cases, treating sleep apnea can even reverse existing AFib, leading to a more regular and healthy heartbeat.
Heart Failure and Sleep Apnea
Heart failure is a condition in which the heart is unable to pump blood effectively, leading to a buildup of fluid in the lungs and other parts of the body. Studies have shown that individuals with sleep apnea are at an increased risk of developing heart failure. This is likely due to the strain placed on the heart as it works harder to pump oxygen-rich blood through the body during episodes of sleep apnea.
Treating sleep apnea can help improve heart function and reduce the risk of heart failure. In some cases, individuals with heart failure who receive treatment for sleep apnea may experience an improvement in their condition.
High Blood Pressure and Sleep Apnea
High blood pressure, or hypertension, is a common risk factor for heart rhythm disorders. Sleep apnea can contribute to the development of high blood pressure by causing fluctuations in blood pressure during sleep. When breathing is disrupted during sleep, the body releases stress hormones that cause blood vessels to constrict, leading to increased blood pressure.
Addressing sleep apnea through treatment can help lower blood pressure and reduce the risk of heart rhythm disorders. In some cases, treating sleep apnea can even eliminate the need for blood pressure medication.
Treatment Options for Sleep Apnea and Improved Heart Health
Fortunately, there are several treatment options available for individuals with sleep apnea. The most common treatment is continuous positive airway pressure (CPAP) therapy, which involves wearing a mask over the nose and/or mouth during sleep. The mask provides a continuous flow of air, helping to keep the airway open and prevent apnea episodes. Other treatment options include lifestyle changes, such as weight loss and avoiding alcohol and sedatives, as well as positional therapy for those with positional obstructive sleep apnea.
By addressing sleep apnea through treatment, individuals can improve their heart health and reduce the risk of heart rhythm disorders. It is important to work closely with a healthcare professional to determine the best treatment plan for each individual's unique needs.
Conclusion: The Importance of Addressing Sleep Apnea for Heart Health
In conclusion, there is a clear link between sleep apnea and heart rhythm disorders. The disruptions in sleep and oxygen levels caused by sleep apnea can lead to an increased risk of atrial fibrillation, heart failure, and high blood pressure. By seeking treatment for sleep apnea, individuals can improve their heart health and reduce the risk of these serious conditions. It is crucial for those with sleep apnea to work closely with their healthcare provider to develop a comprehensive treatment plan that addresses both sleep apnea and any associated heart health issues.





Doris Montgomery
Honestly, this article reads like a textbook you skim through in a coffee shop. The link between sleep apnea and arrhythmias is real, but the prose feels a bit fluffy. I'd say most readers get the gist after a quick glance, though. Still, the takeaway about CPAP helping heart health is spot on.
Nick Gulliver
Wake up, America-sleep apnea is stealing our heartbeats.
Sadie Viner
Thank you for presenting the evidence in a clear and structured manner. The physiological mechanisms-intermittent hypoxia, sympathetic surges, and blood pressure variability-are well articulated. Moreover, the discussion of atrial fibrillation risk aligns with current cardiology guidelines. Your emphasis on multidisciplinary management, involving sleep specialists and electrophysiologists, is commendable. I anticipate that this synthesis will aid clinicians in integrating sleep studies into routine cardiac assessment.
Kristen Moss
Yo, if you think the US doesn't care about sleep apnea, think again. We got the best CPAP tech out there, so let’s fix those heart beats before they mess up the nation’s stats.
Rachael Tanner
Let me elucidate: the cascade from nocturnal hypoxemia to ventricular remodeling is akin to a domino effect, each tile representing a stressor that destabilizes cardiac electrophysiology. Researchers have quantified a 30% uptick in atrial fibrillation incidence among moderate‑to‑severe OSA cohorts, a statistic that should ignite urgency in both primary care and cardiology practices. Moreover, gold‑standard polysomnography remains the linchpin for accurate phenotype classification, distinguishing obstructive from central events. In essence, neglecting sleep apnea is tantamount to ignoring a silent saboteur of cardiac rhythm.
Debra Laurence-Perras
Great job breaking down a complex topic into digestible pieces! It's uplifting to see how treating sleep apnea can ripple into better heart health for countless people. Keep spreading this hopeful message-every patient empowered with knowledge takes a step toward a healthier future.
dAISY foto
OMG guys, this stuff is so eye‑opening!! I mean, who knew that a simple mask could save your heart from goin' crazy? Let's all get that CPAP on and boom-heart rhythm back on track. Seriously, sleep tight and let the air do its magic!!!
Ian Howard
Building on Rachael’s point, recent meta‑analyses have demonstrated that effective CPAP adherence reduces atrial fibrillation recurrence by roughly 40% after catheter ablation. The underlying mechanism appears to revolve around dampening nocturnal sympathetic bursts, which otherwise perpetuate atrial ectopy. Additionally, weight loss synergizes with CPAP, curbing the mechanical load on the upper airway and further stabilizing cardiac electrophysiology. Clinicians should therefore screen for OSA in any patient presenting with unexplained arrhythmias, as targeted therapy can markedly improve outcomes. Integrating sleep assessments into cardiology clinics is a pragmatic step toward holistic care.
Chelsea Wilmer
While I acknowledge Ian’s thorough breakdown of the synergistic benefits of CPAP adherence and weight management, it is imperative to recognize that the simplistic reductionist view presented, which posits a linear causality between nocturnal hypoxia and atrial fibrillation, fails to accommodate the complex interplay of genetic predisposition, inflammatory cytokine cascades, and autonomic remodeling that collectively sculpt the arrhythmic substrate. Indeed, the intricate choreography of ion channel expression, gap junction remodeling, and myocardial fibrosis proceeds on a temporal axis that is modulated not solely by breathing interruptions but also by circadian rhythm disruptions, oxidative stress markers, and the elusive yet potent influence of neurohormonal feedback loops. Consequently, a patient who exhibits commendable CPAP compliance yet persists with a burden of atrial ectopy may, in fact, be manifesting an upstream epigenetic signature that predisposes to electrical instability independent of apnea severity. Moreover, the literature increasingly suggests that the mere presence of central sleep apnea, often overlooked in favor of its obstructive counterpart, introduces a pattern of Cheyne‑Stokes respiration that can precipitate ventricular ectopy through intermittent hypercapnia and heightened chemoreflex sensitivity, thereby complicating the therapeutic algorithm. Furthermore, one must consider the socio‑economic determinants that shape access to high‑quality sleep studies, as disparities in healthcare delivery can engender delayed diagnosis, suboptimal device titration, and ultimately a persistence of arrhythmic risk. Taking a holistic view, the integration of wearable technology for continuous nocturnal monitoring, combined with machine‑learning algorithms capable of parsing subtle waveform variations, offers a promising frontier for preemptive identification of patients at imminent risk of transition from paroxysmal to persistent atrial fibrillation. In this context, the role of multidisciplinary clinics-where cardiologists, pulmonologists, sleep technologists, and behavioral therapists converge-cannot be overstated, for they foster an environment wherein personalized treatment plans can be iteratively refined. Finally, the philosophical implication that sleep, a state often dismissed as passive, is in fact a dynamic arena where the heart negotiates its rhythm, reminds us that the pursuit of health must transcend isolated symptom management and embrace the interconnected tapestry of human physiology.