Keeping emergency medications like epinephrine, naloxone, or nitroglycerin both accessible and secure isn’t just a best practice-it’s a life-or-death balance. You need them ready in seconds during a cardiac arrest, allergic reaction, or opioid overdose. But you also can’t leave them where a child can grab them, a visitor can steal them, or heat can ruin them. This isn’t about being paranoid. It’s about being smart.
Know What You’re Storing
Not all emergency meds are the same. Epinephrine auto-injectors (like EpiPens) work best at room temperature. Refrigerating them can damage the device. Naloxone (Narcan) is more forgiving but still needs to stay dry and cool. Nitroglycerin tablets lose potency fast if exposed to light or air. Each has its own rules.Check the label. Manufacturers often list storage temps: 20°C-25°C (68°F-77°F) is standard for most. Some say 15°C-30°C (59°F-86°F) is acceptable. Anything above 40°C (104°F) can break down the drug. That means don’t store them on a windowsill, in a car glovebox, or near a radiator. Even a bathroom cabinet above the sink can get too hot from steam.
Home Storage: Lock It, But Not Too Tight
In homes, the biggest risks are kids and accidental misuse. The EPA recommends locked cabinets or safes. But here’s the catch: if it takes 30 seconds to open the lock during a seizure or anaphylaxis, it’s too slow.Many families solve this with a two-tier system. Keep the primary dose-say, an EpiPen-in a small, clearly labeled container on a high shelf in the kitchen or hallway. No lock. Just out of reach of toddlers. Then store backups in a locked box in a bedroom closet or a medicine safe. That way, the one you need right now is seconds away. The others are safe.
Medicine safes are cheap now. You can buy one for under £30 that fits in a drawer. Look for ones with a key or combination lock, not just a latch. Some even have alarms. If you use naloxone, keep it near the front door or in the living room-not tucked in a bedroom where visitors might not think to look.
For Caregivers: Kids, Schools, and Daycares
Childcare settings have different rules. In England, Ofsted guidelines say emergency meds like inhalers or epinephrine must be immediately accessible to trained staff but not to children. That means a locked drawer in the nurse’s station, with a key only the supervisor holds. But the drawer must be opened in under 10 seconds during a drill.Many schools now use wall-mounted boxes with push-button locks. Staff enter a code, the box opens, and it logs who accessed it. No keys. No delays. If your child has a severe allergy, ask the school: Where’s the EpiPen? Who has access? How often do they test it?
And never, ever leave meds on a countertop because “I’ll remember.” A 2022 FDA review found only 43% of prescription labels include clear storage instructions. That means you can’t rely on the label. You have to decide for yourself.
EMS and Hospitals: The Rules Are Tighter
In ambulances and hospitals, storage is regulated. The DEA requires controlled substances (like morphine or fentanyl) to be in locked, substantially built cabinets. Schedule II drugs (strong opioids) must be stored separately. But emergency meds like epinephrine or atropine? They’re often kept in crash carts-locked, but with a quick-release mechanism.Here’s what works: tamper-evident seals. If someone opens the cart, the seal breaks. That tells staff someone accessed it. In operating rooms, the American Society of Anesthesiologists says meds should be secured with locks that can be broken quickly by authorized staff. Think of it like a fire extinguisher-locked, but designed to be smashed open if needed.
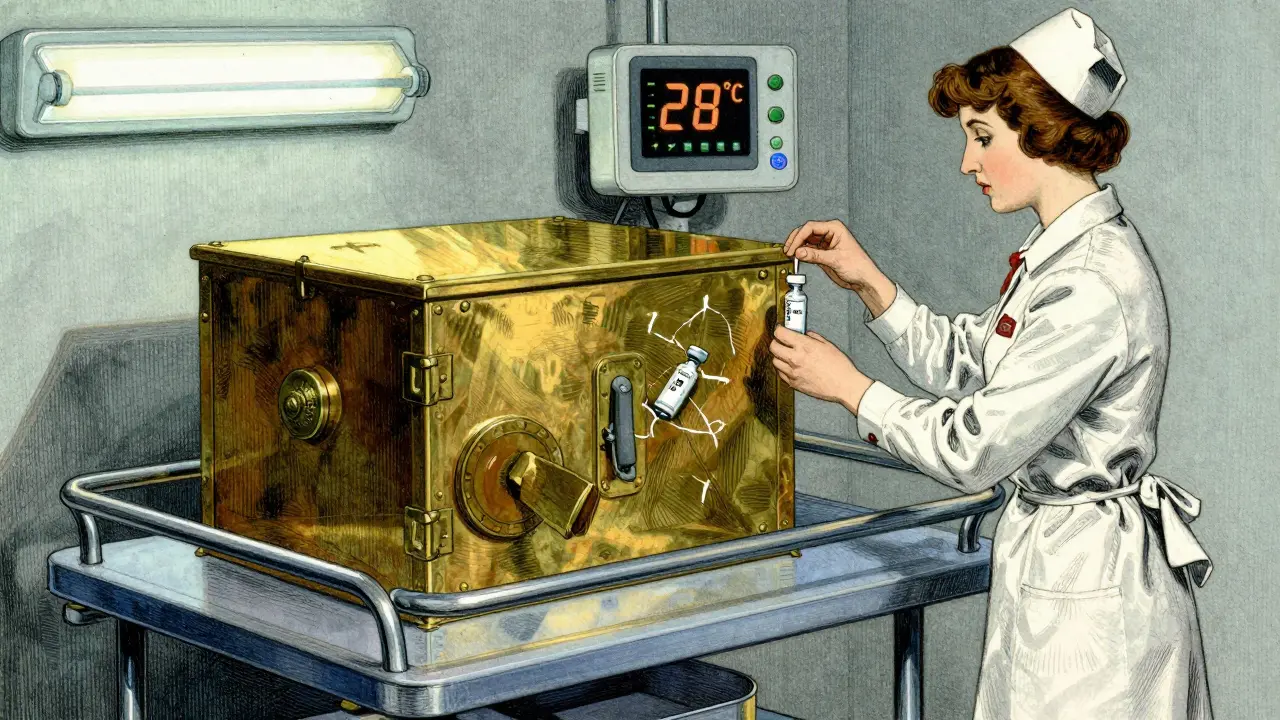
Temperature matters here too. EMS vehicles in winter can drop below freezing. In summer, they can hit 50°C. That’s why smart EMS units now use portable temperature monitors. If the box hits 30°C for more than 10 minutes, an alert goes off. The FDA-approved TempTraq system, tested by the University of Michigan, is 99.2% accurate. It’s not science fiction-it’s standard in many UK ambulance services now.
What Not to Do
- Don’t store meds in the fridge unless the label says so. Cold can ruin auto-injectors.
- Don’t keep them in a purse or backpack. Heat, pressure, and movement can damage them.
- Don’t assume your partner knows where they are. Practice with them. Show them how to open the box.
- Don’t ignore expiration dates. Epinephrine loses potency after 12-18 months. Replace them on time.
- Don’t hide them so well that even you can’t find them in panic. Label everything clearly: “EPINEPHRINE - EMERGENCY ONLY.”

Training and Drills Save Lives
A 2023 study in the American Journal of Health-System Pharmacy found that 85% of staff became confident in handling emergency meds after just two 90-minute training sessions. That’s not much time. But it’s enough.Practice at home. Set a timer. Can you find the EpiPen in under 15 seconds? Can your teenager open the lock? Can your partner read the instructions without panicking? Do a mock drill once a month. Treat it like a fire drill.
Some families keep a small checklist taped to the medicine box: 1. Locate. 2. Remove. 3. Inject. 4. Call 999. Simple. Clear. No guesswork.
The Future Is Smarter
By 2027, Gartner predicts 65% of hospitals will use AI-powered systems that adjust access based on real-time risk. If a patient’s heart rate drops suddenly, the cabinet unlocks automatically for the nurse. If a visitor tries to open it, the system sends an alert.For homes, that tech is coming too. Smart medicine boxes with fingerprint locks, app alerts when meds are taken, and auto-replacement reminders are already on the market. Sales of these devices jumped 28% in the first half of 2024.
But the core principle hasn’t changed: speed matters, but safety matters more. The goal isn’t to lock everything away. It’s to make sure the right person can get the right drug in the right second-without anyone else getting in.
When It’s Time to Dispose
Expired meds? Don’t flush them. Don’t toss them in the trash. The EPA says take them to a pharmacy drop-off box. Many UK pharmacies now have free take-back containers. If yours doesn’t, call your local council. Some cities run biannual collection days.For naloxone or epinephrine pens: remove the needle (if detachable), put the device in a sealed plastic bag, and drop it in the disposal bin. Never leave them in a drawer where someone else might find them.
Can I keep emergency meds in my car?
Generally, no. Car interiors can reach 60°C in summer and drop below freezing in winter. Both extremes can ruin medications like epinephrine or nitroglycerin. If you must, use a thermal-insulated case with a cold pack-but even then, check the meds every 3 months. Better to keep them at home or work where temperature is controlled.
What if I’m not sure whether my EpiPen still works?
Check the solution inside. If it’s discolored (pink or brown), cloudy, or has particles, throw it out. Even if it’s not expired, it’s no longer safe. Replace it. Most manufacturers offer patient assistance programs if cost is an issue. Don’t risk it.
Is it legal to store naloxone at home without a prescription?
Yes, in the UK, naloxone is available over-the-counter at pharmacies without a prescription. You don’t need to be a doctor or have a patient’s name to buy it. Many local councils give it out for free to families at risk of opioid overdose. Keep it in a visible, accessible spot.
Should I store emergency meds in a pill organizer?
No. Pill organizers expose meds to air, light, and moisture, which can degrade them. They’re meant for daily pills, not emergency drugs. Keep emergency meds in their original packaging with the label intact. That’s how you know the dose, expiry, and storage instructions.
What’s the biggest mistake people make?
Putting it away too well. I’ve seen families lock epinephrine in a safe behind five layers of locks, then panic when they can’t find the key. Or store it in a drawer with 20 other things. The best system is simple: one clear location, easy access, labeled clearly, and practiced regularly. Speed isn’t optional-it’s the whole point.







Mark Harris
This is so spot on. I keep my kid's EpiPen in a bright yellow case on the fridge door. No lock, just high enough she can't reach it. We practice every Sunday after pancakes. Seriously, if you don't drill this, you're gambling with their life.
Mayank Dobhal
Dude. Just keep it in your pocket. Done.
Ariel Edmisten
Love the two-tier system. My mom used to hide hers in a cookie jar. We almost lost her once because no one knew where it was. Now it’s in a labeled box next to the coffee maker. Simple. Fast.
Ashley Hutchins
Why do people still store meds in bathrooms? I swear half the population thinks steam is fine for epinephrine. Stop. Just stop. It's not a sauna. It's a life saver.
Lakisha Sarbah
I work in a daycare and we use those wall-mounted boxes with codes. Staff love them. Parents love them. Kids can't get in. And if someone tries to open it without the code, it pings the admin's phone. Genius.
Ritu Singh
In India, we often face challenges with storage due to extreme heat. Many families keep naloxone in the coolest corner of the house-near the AC vent or in a sealed metal box. I recommend placing it in a sealed ziplock with silica gel packs. It’s low-cost, effective, and culturally adaptable. Also, training should be community-based. Not every household has a pharmacist nearby.
Niel Amstrong Stein
I got one of those smart medicine boxes last month. 🤖 It sends me a text if someone opens it, reminds me when refills are due, and even locks if the temp goes too high. Cost like $80 but worth it. My mom’s nitroglycerin is now safer than my phone. 📱💉
Mary Carroll Allen
I used to think I was being careful by locking everything away. Then my husband had a panic attack and we spent 4 minutes hunting for the key to the safe. FOUR MINUTES. We lost 20 seconds just finding the damn keychain. Now? One EpiPen on the counter. One backup in the locked drawer. I made a laminated checklist. We do drills every month. No more guessing. No more panic. Just action.
AMIT JINDAL
lol why are we overcomplicating this. just keep it in the glovebox with a sticker that says EMERGENCY. car temp? who cares. if you're having a reaction you don't care if the pen is 2% less effective. just use it. also why are you even storing this if you dont know how to use it? maybe dont have kids if you cant handle it. 🤷♂️
Savannah Edwards
I’ve been a nurse for 18 years and I’ve seen too many families treat emergency meds like a chore. It’s not about storage-it’s about identity. If you don’t treat this medication like part of your family’s survival system, you’re setting them up to fail. I had a mom once who kept her daughter’s EpiPen in a purse that got stolen. The girl had a reaction the next day. She didn’t survive. That’s not negligence. That’s systemic failure. We need to normalize talking about this. Like sex ed. Like fire drills. Like CPR. It’s not optional. It’s biology. And if you’re too lazy to label it, or too proud to practice, you’re not just being careless-you’re choosing not to love them as hard as you can.
Heather Burrows
I get that speed matters. But isn’t this just enabling reckless behavior? If you have to rely on a 15-second window, maybe the real problem is that you’re living with a condition that shouldn’t be left unmanaged. Why not focus on prevention instead of storage hacks?
Mark Harris
To the person who said 'just keep it in your pocket'-you’re lucky you’ve never had to watch someone turn blue because the EpiPen was in a bag they couldn’t reach. Not everyone lives in a 200 sq ft studio. Some of us have toddlers. Some of us have dogs. Some of us have grandparents with narcolepsy. This isn’t about convenience. It’s about safety. And you don’t get to decide what safety looks like for someone else.
Paula Sa
I love that the article mentions the TempTraq system. My husband’s EMS team uses them. One time, the box hit 31°C for 12 minutes during a heatwave. The alert went off. They replaced the epinephrine before a call came in. Saved a life. Tech isn’t magic-but when it’s built for real-world chaos? It’s a hero.
Joey Gianvincenzi
The notion that 'speed matters more than safety' is dangerously reductive. True safety is systemic. It requires institutional accountability, standardized training, and regulatory oversight-not just a labeled box on a kitchen shelf. Until we treat emergency medication access as a public health imperative-not a personal responsibility-we will continue to bury children because we prioritized convenience over compliance.