Starting a new medication can feel overwhelming. You’re handed a prescription, a bottle with tiny print, and maybe a quick explanation from your doctor. But what happens when you get home? What if you forget when to take it? What if the pill looks different than last time? What if you’re not sure if it’s safe to take with your other pills? These aren’t just questions-they’re risks. Every year, over 1.3 million people in the U.S. end up in the emergency room because of medication mistakes. And most of them are preventable.
Why Medication Safety Matters More Than You Think
Medication errors aren’t rare. They’re common-and often silent. A 2021 Johns Hopkins study found that medication mistakes contribute to about 7,000 deaths in U.S. hospitals each year. That’s more than car accidents. The good news? Research from the Agency for Healthcare Research and Quality shows that following basic safety steps can cut these errors by up to 50%. It’s not just about avoiding side effects. It’s about making sure the medicine actually works. The World Health Organization says half of all treatment failures for chronic conditions like high blood pressure or diabetes happen because people don’t take their meds as directed. Not because the drug doesn’t work-but because they missed doses, took too much, or mixed it with something dangerous.The Six Rights of Safe Medication Use
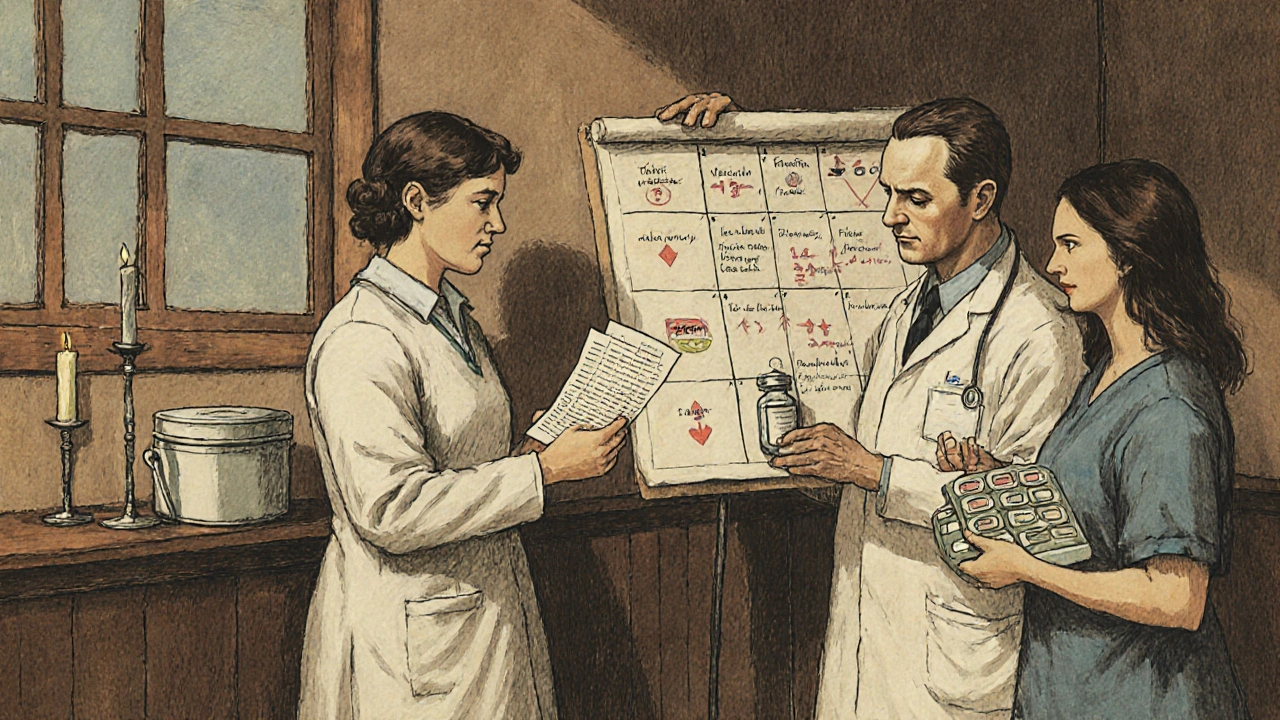
Healthcare providers use a simple checklist called the “Six Rights” to keep patients safe. You can use it too. Before you take any pill, ask yourself:- Right patient: Is this medicine really for you? Double-check your name and date of birth on the label. Don’t assume-mistakes happen.
- Right medication: Does the pill match what your doctor prescribed? If it looks different than last time, ask your pharmacist. Generic versions are just as effective, but they can look totally different.
- Right indication: Why are you taking this? Don’t just swallow it because you were told to. Know what it’s for-whether it’s for blood pressure, pain, or an infection.
- Right dose: Never use a kitchen spoon. Use the measuring cup, syringe, or dosing cap that came with the medicine. Household spoons can be off by 25% to 50%. That’s not a small mistake-it’s dangerous.
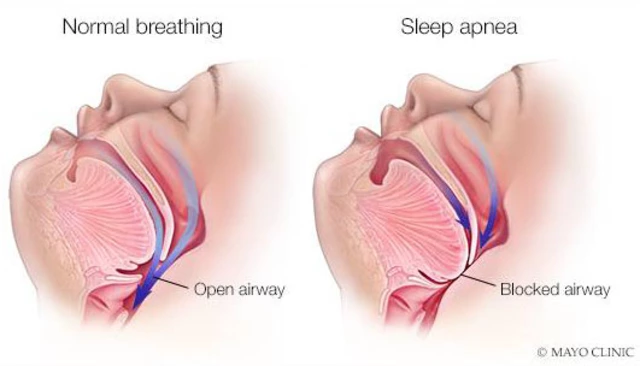
- Right route: Is it meant to be swallowed, placed under the tongue, applied to the skin, or injected? Taking a cream orally or a pill as a suppository can cause serious harm.
- Right time: Does it need to be taken with food? On an empty stomach? At bedtime? Some meds work better at certain times of day. Missing the timing can reduce effectiveness or increase side effects.
Keep a Complete Medication List
Most people don’t realize how many things they’re taking. Prescription drugs. Over-the-counter painkillers. Vitamins. Herbal supplements. Even daily aspirin. All of them matter. A 2022 study in the Journal of the American Pharmacists Association found that patients who kept a full, updated list of everything they took had 27% fewer medication errors. That’s huge. Your list should include:- Full name of the medicine (brand and generic if you know it)
- Dose (e.g., 10 mg, 500 mg)
- How often (once daily, twice a day, every 6 hours)
- Why you’re taking it
- When you started
- Pharmacy name and phone number
Storage Isn’t Optional
Not all pills are created equal when it comes to storage. Heat, moisture, and light can break them down-sometimes without you knowing.- Insulin: Must be refrigerated (36-46°F) until first use. After that, it can stay at room temperature for up to 28 days.
- Most oral pills: Store below 86°F in a dry place. Avoid the bathroom cabinet-it’s steamy and hot.
- Liquid antibiotics: Often need refrigeration. Check the label. Leaving them out can make them useless or even harmful.
- Supplements: Many degrade quickly in heat. Store them like you store food-cool and dry.
Never Share or Take Someone Else’s Medicine
It’s tempting. Your friend had a headache and took their ibuprofen. It worked. Maybe it’ll work for you too. Don’t do it. The FDA says sharing medications causes 8% of emergency visits for adverse drug events. Why? Because your body is different. Your weight, allergies, other meds, and health conditions all change how a drug affects you. What’s safe for one person could be deadly for another. Also, never take medicine that’s not labeled. If a pill is in a baggie with no name, no dosage, no instructions-don’t take it. Mislabeling causes 12% of hospital medication errors.Ask Questions-No Matter How Small They Seem
Pharmacists are trained to help you understand your meds. But most patients don’t ask enough. A 2022 study showed that patients who asked three or more questions about a new prescription had 34% fewer side effects in the first month. Here are the three most important questions to ask every time you get a new medicine:- What should I do if I miss a dose? Only 22% of patients ask this. But the answer matters. Some meds you take as soon as you remember. Others you skip entirely. Getting it wrong can cause harm.
- How should I store this? Forty percent of medications have specific storage needs. If you don’t ask, you might ruin the drug before you even take it.
- What side effects should I watch for? Only 65% of pharmacy consultations cover this, according to AHRQ. Know what’s normal (like mild nausea) and what’s dangerous (like swelling, trouble breathing, or chest pain).
Use Tools to Stay on Track
Remembering when to take your pills gets harder when you’re on multiple meds. A 2023 University of Michigan study found it takes most first-time users 2-3 weeks to build a reliable routine. Use tools to help:- Medication reminder apps: Apps like Medisafe and MyMeds send alerts and track your doses. A 2022 study showed they improve adherence by 28%. The best ones let you scan the barcode on your bottle to confirm you’re taking the right pill.
- Weekly pill organizers: Simple, low-tech, and effective. Fill them once a week. Use different compartments for morning, afternoon, night.
- Phone alarms: Set multiple alarms if needed. Label them clearly: “AM Blood Pressure Pill,” “Evening Pain Med.”
Watch for Changes and Speak Up
If your pill looks different-color, shape, size, markings-don’t assume it’s the same drug. Generic versions are legally required to work the same, but they often look totally different. That’s normal. But you should still confirm with your pharmacist. Also, pay attention to how you feel. New dizziness? Rash? Trouble sleeping? Nausea that won’t go away? These could be side effects-or signs of a bad interaction. If something feels off, call your doctor or pharmacist. Don’t wait. Don’t Google it. Don’t assume it’ll pass. Medication safety isn’t about being perfect-it’s about being aware and speaking up.What to Do When You’re Discharged from the Hospital
One of the riskiest times for medication errors is right after you leave the hospital. A 2023 Patient Safety Network report found that 22% of errors happen during care transitions. Before you go:- Ask for a written list of all your meds-what you’re taking now, what you’ve stopped, and what’s new.
- Ask: “What changed from when I came in?”
- Ask your pharmacist to review all your meds side by side with your home list.
- Don’t leave without knowing how to take your new prescriptions.
Final Tip: You’re the Most Important Person in Your Care
Doctors, nurses, and pharmacists are experts. But you’re the one who takes the pills. You know your body best. You’re the only one who can catch a mistake before it happens. Medication safety isn’t about memorizing rules. It’s about being curious. Being careful. Asking questions. Writing things down. Using tools. Speaking up. The goal isn’t to be perfect. It’s to be informed. And with these steps, you’re already ahead of most people.What should I do if I accidentally take the wrong dose?
Don’t panic, but don’t wait. Call your pharmacist or poison control (1-800-222-1222 in the U.S.) immediately. Have the medicine bottle handy so you can tell them the name, dose, and how much you took. They’ll tell you whether to monitor for symptoms, take an antidote, or go to the ER. Never try to induce vomiting unless instructed by a professional.
Can I crush my pills or open capsules if I have trouble swallowing them?
Only if your doctor or pharmacist says it’s okay. Many pills are designed to release slowly over time. Crushing them can make the medicine work too fast and cause dangerous side effects. Extended-release tablets, capsules with coatings, and some blood pressure or psychiatric meds should never be crushed. Always ask before changing how you take your medicine.
Are over-the-counter meds safe to take with my prescriptions?
Not always. Common OTC drugs like ibuprofen, antacids, cold medicines, and even some herbal supplements can interact badly with prescription meds. For example, ibuprofen can increase bleeding risk if you’re on blood thinners. Antacids can block absorption of antibiotics. Always check with your pharmacist before taking anything new-even if it’s sold without a prescription.
How do I know if a medicine is expired?
Look for the expiration date on the bottle or box-it’s usually labeled “EXP” followed by a month and year. For pills, if they’re cracked, discolored, or smell odd, throw them out-even if the date hasn’t passed. Liquid meds, especially antibiotics and insulin, are more sensitive. If they look cloudy, clumpy, or have particles, don’t use them. When in doubt, ask your pharmacist.
Why do I need to know the difference between brand and generic drugs?
You don’t need to prefer one over the other. Generic drugs contain the same active ingredient as brand names and are required by the FDA to work the same way. But they can look different in shape, color, or size. That’s normal. What matters is that the active ingredient and dose match. If your generic pill looks different from your last refill, ask your pharmacist to confirm it’s the right medicine. Never assume.







Adrian Rios
Man, I wish I had this guide when I first started on blood pressure meds. I took them with grapefruit juice because I thought it’d make them work faster-turns out, that’s a one-way ticket to ER land. Learned the hard way. Now I keep a laminated card in my wallet with every med, dose, and time. My pharmacist even gave me a sticker for it. Small things, big difference.
Casper van Hoof
One is compelled to reflect upon the epistemological foundations of pharmaceutical compliance. The notion of agency in medical adherence is not merely behavioral but ontological-rooted in the individual’s capacity to reconcile institutional knowledge with somatic experience. The Six Rights, while pragmatically useful, risk reducing patient autonomy to a checklist.
Richard Wöhrl
Just a quick note: if you're on warfarin, NEVER take ibuprofen without checking with your doctor-or your pharmacist, who actually knows what they're talking about. I had a friend who thought 'it's just a painkiller' and ended up in the hospital with internal bleeding. Also, don't store meds in the bathroom. Steam ruins everything. And yes, use the dosing cup. A teaspoon is NOT a measuring tool. Seriously. I've seen this too many times.
Pramod Kumar
Bro, this hit different. I used to just grab pills like snacks-until my grandma almost died from mixing her diabetes med with a herbal tea she thought was 'natural detox.' She’s fine now, but man, that scared me straight. I started using Medisafe and now I even remind my cousins when they’re on antibiotics. It’s not just about you-it’s about everyone around you. Keep it clean, keep it clear.
Brandy Walley
lol why are we treating adults like toddlers? if you can’t remember to take a pill maybe you shouldn’t be on meds. also who even uses pill organizers anymore? i just set a reminder on my phone. this article is so condescending.
shreyas yashas
Real talk-my uncle took his blood thinner with green tea because he read it 'helps circulation.' He didn’t tell anyone. Ended up in ICU. Don’t be that guy. Use the list. Talk to the pharmacist. They don’t bite. I used to think I knew everything till I got my first script. Now I ask questions like a kid in a candy store. Best habit I ever picked up.
Lisa Lee
U.S. healthcare is a joke. We need single-payer so people don’t have to Google if their pill is expired. Also why are we blaming patients? Doctors write illegible scripts, pharmacists rush, and then we get lectured like we’re 5? This feels like victim-blaming dressed up as advice.
JD Mette
I appreciate the thoroughness. I’ve been on multiple medications for years and still forget to update my list. I’m going to start keeping a digital version in my notes app. Also, I didn’t realize liquid antibiotics needed refrigeration-I’ve been leaving mine out. Thanks for the reminder.
Dalton Adams
Let’s be real-this guide is basic. I’ve been a clinical pharmacist for 17 years and even I cringe at how obvious this is. But then again, most patients treat their meds like they’re playing Russian roulette with a blindfold. The fact that 1.3 million end up in the ER? That’s not ignorance-it’s negligence. And yes, crushing pills? That’s not just dangerous, it’s a felony in some states. 🤦♂️
Matthew Mahar
I didn’t know expired meds could turn toxic. I’ve been keeping my old antibiotics in my drawer ‘just in case.’ I’m throwing them out tonight. Also, I never realized my vitamin D was supposed to be kept in the fridge. My house is 75 degrees… I’ve been cooking my supplements. 😅
John Mackaill
Brilliant breakdown. I’ve worked in community pharmacy for over a decade and can confirm: the single biggest issue isn’t patient compliance-it’s communication. Patients leave the pharmacy with a bottle and zero context. We’re rushed. They’re overwhelmed. A simple 30-second chat about storage or timing changes everything. This guide should be handed out with every script.
Katy Bell
I’m 28 and on 5 meds. I used to think I was fine until I mixed my thyroid med with coffee and felt like a cartoon character for 3 hours. Now I take everything with water, at the same time, and I write it down. Also, I keep my meds in a little box under my bed. No bathroom. No sun. No chaos. Just me, my pills, and my peace of mind.
Ragini Sharma
soooo… i took my blood pressure pill at night instead of morning bc i forgot and now im kinda scared? also i think my generic looks diff but its the same brand? help? lol
Henrik Stacke
As someone who grew up in a household where medicine was treated like a sacred ritual-measured with spoons, stored in the pantry, and never questioned-I can say with absolute certainty that this guide is not just helpful, it’s lifesaving. My mother took her insulin at room temperature for years because ‘it’s always been that way.’ She’s still here, but barely. Knowledge is power, and power, in this context, is survival.