Macrolide Heart Risk Assessment Tool
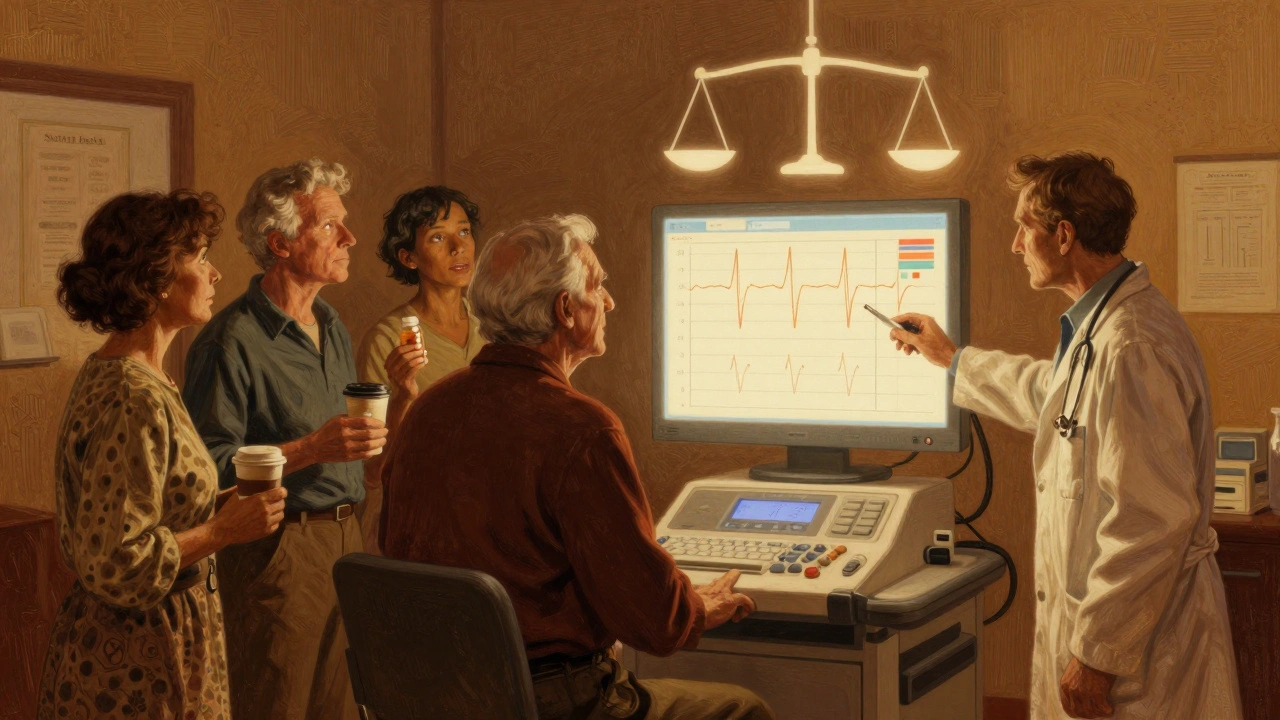
This tool helps determine if you should get an ECG before starting macrolide antibiotics (like azithromycin, clarithromycin, or erythromycin) based on your personal risk factors. The American Heart Association's 2025 guidelines recommend using a 9-point risk score to identify high-risk patients.
Your Risk Assessment
Every year, millions of people take macrolide antibiotics like azithromycin, clarithromycin, and erythromycin for common infections-strep throat, bronchitis, pneumonia. Most walk away feeling better. But for some, these drugs can quietly mess with their heart rhythm. The danger? A dangerous arrhythmia called Torsades de Pointes, which can lead to sudden cardiac arrest. It’s rare-but when it happens, it’s often preventable. And the key to prevention isn’t avoiding the drug. It’s knowing who needs an ECG before they start taking it.
Why Macrolides Can Be Risky for Your Heart
Macrolides don’t just kill bacteria. They also block a specific potassium channel in heart cells called hERG. This slows down the heart’s electrical reset after each beat, which shows up on an ECG as a longer QT interval. A prolonged QT interval means the heart takes longer to recharge between beats. When it’s too long, the heart can develop chaotic, dangerous rhythms. The risk isn’t the same for everyone. Erythromycin carries the highest risk-nearly five times more likely to cause QT prolongation than azithromycin, based on pooled data from 13 studies. Azithromycin is safer, but it’s still linked to a 2.7-fold higher risk of cardiovascular death compared to amoxicillin, according to a major 2012 study in the New England Journal of Medicine.The absolute risk of Torsades de Pointes is low-about 1 to 8 cases per 10,000 patient-years. But that number jumps sharply when the corrected QT interval (QTc) hits 500 milliseconds or more. For every 10 extra milliseconds beyond 500 ms, the risk of a life-threatening arrhythmia goes up by 5-7%. That’s not a small bump. That’s a red flag.
Who Should Get an ECG Before Starting Macrolides?
Not everyone needs an ECG. But certain people are at much higher risk. The British Thoracic Society (BTS) says: if you’re starting long-term macrolide therapy-for conditions like bronchiectasis or cystic fibrosis-you need a baseline ECG before the first dose. Their cutoff? QTc over 450 ms in men, over 470 ms in women. That’s not arbitrary. These values are backed by years of data showing when the risk becomes clinically meaningful.But what about people taking macrolides for a short course-say, five days for a sinus infection? Here’s where things get messy. The UK’s NHS says you only need an ECG if you have risk factors. So what are those risk factors?
- Female sex: Women are almost three times more likely than men to develop drug-induced long QT syndrome.
- Age 65 or older: The risk more than doubles after 65.
- Existing heart disease: History of heart failure, prior arrhythmia, or congenital long QT syndrome.
- Low potassium or magnesium: Common in people on diuretics or with eating disorders.
- Multiple QT-prolonging drugs: Taking azithromycin with antidepressants, antifungals, or antiarrhythmics? That’s a dangerous combo.
- Chronic kidney disease: Impaired clearance means higher drug levels in the blood.
If you have two or more of these, your risk isn’t just higher-it’s high enough that skipping an ECG is a gamble. A 2024 study of 247 primary care doctors found that 78% knew macrolides could affect the heart, but only 22% routinely ordered ECGs. Why? Time. Cost. Uncertainty. But one Reddit post from a nurse in Manchester tells a different story: a 68-year-old woman with a QTc of 480 ms took clarithromycin for pneumonia. Five days later, she went into Torsades. She survived, but only because her ECG was reviewed in the ER. That ECG was never done before she left the clinic.

When ECGs Are Mandatory (and When They’re Not)
There’s a clear divide between hospital and community care. In the ICU, if you’re on a macrolide and being monitored continuously, you’re fine. But if you’re being moved to a regular ward and the monitor gets turned off? You need a new ECG. The REMAP-CAP trial guidelines are clear: if QT prolongation develops, stop the drug.In outpatient settings, it’s a mess. Only 12% of primary care clinics in the UK follow ECG guidelines for macrolides. In the US, it’s even worse-just 18% of primary care providers screen before prescribing. Meanwhile, specialized respiratory clinics following BTS guidelines hit 87% compliance. Why the gap? It’s not that doctors don’t care. It’s that they’re overwhelmed. A single ECG costs about £28.50 in the UK. Multiply that by 12 million annual macrolide prescriptions, and you’re looking at £342 million a year. No health system can afford universal screening.
So the smart answer isn’t to screen everyone. It’s to screen the right people. The American Heart Association’s 2025 update recommends a 9-point risk score: add one point for age over 65, one for female sex, one for kidney disease, one for low potassium, one for each additional QT-prolonging drug, and so on. Score of 4 or higher? Get an ECG. Score below 2? You’re likely safe for a short course. This isn’t theory-it’s practice. Epic’s electronic health record system now flags macrolide prescriptions with automated QTc alerts in 43% of US hospitals. That’s progress.
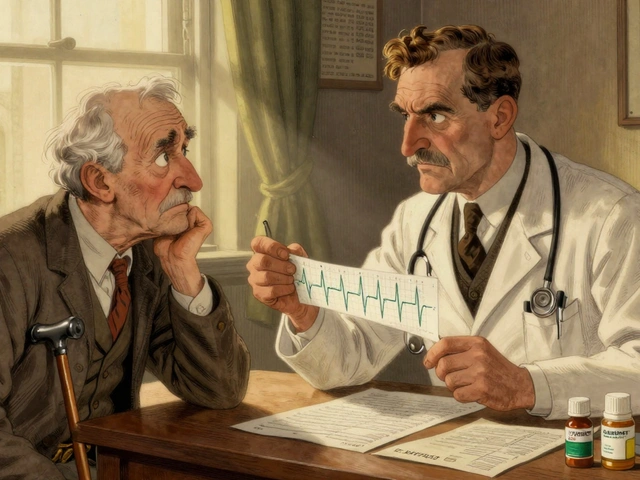
What Happens After the ECG?
If your QTc is normal-under 450 ms for men, under 470 ms for women-you’re good to go. No further ECGs needed for a short course. But if you’re on long-term therapy (think months, not days), you need a repeat ECG at one month. Why? Because QT prolongation can develop slowly. Some patients start with a normal reading and drift into danger after weeks of daily dosing.If your QTc is borderline-470 to 499 ms-don’t panic. But don’t ignore it either. Stop other QT-prolonging drugs. Check your electrolytes. Consider switching to a different antibiotic. Azithromycin might still be okay, but clarithromycin? Probably not. And if your QTc is 500 ms or higher? Don’t start the macrolide at all. Find another treatment. The NIH’s 2025 analysis says that when you control for all the other risk factors, the drug itself isn’t the main culprit-it’s the combination. So fix the combination first.
What You Can Do Right Now
If you’re prescribed a macrolide:- Ask: “Do I have any risk factors for heart rhythm problems?”
- Ask: “Should I get an ECG before I start this?”
- Ask: “Are there other antibiotics I could take instead?”
If you’re a patient with heart disease, kidney issues, or you’re over 65-don’t wait. Push for the ECG. It takes five minutes. It costs less than a coffee. And it could save your life.
If you’re a clinician: use the 9-point risk score. Don’t rely on gut feeling. Use the data. And if your clinic doesn’t have a system for flagging high-risk prescriptions? Advocate for one. Electronic alerts are cheap. They’re accurate. And they’re already working in hospitals across the US and UK.
The Bigger Picture
This isn’t just about antibiotics. It’s about how we manage drugs that affect the heart. We’ve known for decades that some medications can trigger deadly arrhythmias. But we’ve treated them like side effects, not red flags. The truth is, we’re prescribing QT-prolonging drugs every day-antibiotics, antipsychotics, antifungals, even some cancer drugs. And we’re doing it without checking the heart’s electrical system.ECG monitoring during macrolide therapy isn’t about overtesting. It’s about smart testing. It’s about protecting the people who need it most. The British Thoracic Society got it right: baseline ECG for long-term use. The American Heart Association got it right: risk-stratify for everyone else. The data is clear. The tools are available. The only thing missing is consistency.
For the 98% of people who take azithromycin and never have a problem, this won’t change anything. But for the 2% who are at risk? This could be the difference between walking out of the clinic and being rushed to the ER.
Do all macrolide antibiotics carry the same heart risk?
No. Erythromycin has the highest risk of QT prolongation, with an odds ratio of 4.82 compared to azithromycin’s 1.77. Clarithromycin falls in between. Azithromycin is the safest option among macrolides, but it’s still linked to a 2.7-fold increase in cardiovascular death risk compared to amoxicillin. Don’t assume all macrolides are equal.
Can I get an ECG at my local pharmacy or urgent care?
Yes, in many places. Urgent care centers, walk-in clinics, and some pharmacies now offer basic ECG services. It’s quick-usually under 10 minutes-and doesn’t require a doctor’s order in some regions. If your primary care provider won’t order one, ask if you can get it done elsewhere. Many insurance plans cover it when medically indicated.
What if my QTc is borderline-470 to 499 ms?
Don’t start the macrolide yet. Check your potassium and magnesium levels-low levels make QT prolongation worse. Stop any other QT-prolonging medications if possible. Talk to your doctor about switching to a non-macrolide antibiotic. If you must use a macrolide, azithromycin is the safest choice. Recheck your ECG after one week. If the QTc drops, you may proceed. If it climbs, stop the drug.
Is ECG monitoring only needed for long-term use?
No. While long-term use (like for bronchiectasis) requires mandatory baseline and follow-up ECGs, short-term use can still be dangerous if you have risk factors. A 68-year-old woman with kidney disease and on a diuretic can develop Torsades after just three days of azithromycin. Risk isn’t about duration-it’s about your personal profile.
What are the signs of a dangerous heart rhythm from macrolides?
Symptoms can be subtle or sudden. You might feel dizzy, lightheaded, or have palpitations. Some people pass out without warning. Others describe a "fluttering" or "skipping" heartbeat. If you’re on a macrolide and suddenly feel faint, have chest pain, or your heart races uncontrollably, seek emergency help immediately. Torsades de Pointes can turn fatal in minutes.
Are there alternatives to macrolides that don’t affect the heart?
Yes. For respiratory infections, doxycycline, amoxicillin-clavulanate, or fluoroquinolones (like levofloxacin) are often alternatives-but they have their own risks. Fluoroquinolones also carry a QT prolongation warning. The best alternative depends on your infection, allergies, and other health conditions. Never switch antibiotics on your own. Talk to your doctor about the safest option for your profile.




vinoth kumar
Finally, someone breaks down the real risk without sugarcoating it. I work in a rural clinic in Kerala and we see this all the time - old folks on diuretics getting azithromycin for a cough. No ECG. No electrolytes. Just a prescription and a smile. One guy coded last month. We found out his QTc was 520. We didn’t know until it was too late.
shalini vaishnav
Western medicine still clings to outdated protocols. In India, we’ve known for decades that macrolides are dangerous in elderly patients with metabolic imbalances. Why does it take a 2024 study to confirm what our grandmothers warned about? This isn’t science - it’s bureaucracy dressed in white coats.
bobby chandra
Let’s be real - this isn’t about ECGs. It’s about systemic neglect. We’re prescribing QT-prolonging drugs like they’re aspirin while ignoring the fact that we’re playing Russian roulette with cardiac electrophysiology. The fact that Epic’s EHR flags this in less than half of U.S. hospitals is a national disgrace. We have the tech. We have the data. We just don’t have the will.
Archie singh
They’ll never fix this because the pharmaceutical industry profits from ignorance. Azithromycin is cheap. ECGs cost money. Who wins? The lab companies. The hospital systems. Not you. Not me. Not the 68-year-old woman who almost died because her doctor was too busy to click a button.
Gene Linetsky
Did you know the WHO quietly removed azithromycin from their essential meds list in 2023? No one talks about it. They just swapped it for doxycycline and called it a day. The CDC knows. The FDA knows. But the public? They’re still getting prescriptions like it’s 2010. This is controlled demolition of public trust - and no one’s asking why.
Ignacio Pacheco
So let me get this straight - we’re okay with a 2.7x higher risk of cardiac death from azithromycin compared to amoxicillin… but we won’t spend $28.50 to check a QTc? That’s not risk management. That’s statistical nihilism wrapped in a white coat.
Jim Schultz
Wow. Just… wow. A 9-point risk score? Really? That’s what we’ve come to? We used to have clinical judgment. Now we need a spreadsheet to tell us not to kill our patients. And let’s not forget the 78% of docs who know the risk but don’t act - that’s not ignorance. That’s malpractice by omission. Someone’s getting sued. And it’s going to be ugly.
Kidar Saleh
I’ve seen this in Manchester. A nurse walked into the clinic with a patient’s ECG in hand - already done at the pharmacy. The GP rolled his eyes. "We don’t do that here." Two days later, the patient was in cardiac arrest. We got the ECG then. Too late. The system isn’t broken. It’s indifferent. And indifference kills faster than any arrhythmia.
Chloe Madison
ECG before azithromycin. Five minutes. Less than a latte. Do it.