Most people don’t realize that adherence tracking for generic medications is one of the biggest unsolved problems in modern pharmacy. You pick up your prescription, fill your pill organizer, and think you’re good to go. But studies show nearly half of patients stop taking their generic meds within a year-especially for chronic conditions like high blood pressure, diabetes, or cholesterol. And when they do, it doesn’t just hurt their health. It costs the U.S. healthcare system $300 billion a year in avoidable hospital visits and complications. The real question isn’t whether patients care-they do. It’s whether the tools they’re given actually work in real life.
Why Generics Are Different
Generic drugs make up 90% of all prescriptions filled in the U.S. They’re cheaper, FDA-approved, and just as effective as brand-name versions. But here’s the catch: they don’t come with support. Brand-name drugs often include free apps, reminders, or even nurse hotlines. Generics? Nothing. No packaging alerts. No refill nudges. No patient portals. Just a plain bottle with a label that says "Take once daily." That’s where digital adherence tools step in. These aren’t just smartphone alarms. They’re systems built to track exactly when a pill is taken-not just when someone opens the bottle. And they’re becoming essential for pharmacies and patients managing long-term conditions with multiple generics.How Digital Tools Actually Work
There are several types of systems out there, each with their own strengths and flaws.- Smart pill bottles like MEMS AS use electronic caps that log every time the bottle is opened. They sync via Bluetooth to a phone app and send alerts if a dose is missed. AARDEX Group claims 100% accuracy, but in real-world use, patients often forget to carry the bottle or leave it at home.
- Smart pillboxes like Tenovi have built-in LED lights-red for missed doses, green for taken. They connect via cellular signal, so no phone is needed. One user with five daily meds said it cut their missed doses by 40%. But the battery dies every few days, and the device is bulky enough to be awkward on a nightstand.
- Electronic blister packs from Wisepill Technologies pop open only at the right time. Each dose is sealed until it’s due. If you miss it, the system knows. These work well for elderly patients who don’t use smartphones, but they’re expensive and require weekly refills.
- Video monitoring like VDOT asks patients to record themselves taking meds. It’s 95% accurate, but 30% of users quit within three months because it feels invasive. One patient on Reddit said, "I felt like I was being watched every morning. It made me anxious, not compliant."
None of these are perfect. But they all generate data-real, verifiable data-that pharmacies and insurers can use to see who’s struggling before they end up in the ER.
What Works in Real Life?
A lot of these tools look great on paper. But here’s what actually happens in pharmacies:- McKesson’s APS dashboard helped a pharmacy in Ohio boost diabetes adherence from 62% to 78% over 18 months. But they had to hire a full-time tech to manage the system.
- Patients using Tenovi’s pillbox reported a 28% improvement over phone reminders alone. But 40% said the constant tracking felt like surveillance.
- One pilot study with 22 patients showed 64% were still using Med-eMonitor after 30 days. After 60 days? Only 45%. The main reason? "It was too much work."
The pattern is clear: tools that require the least effort from the patient do best. Simple reminder apps? Low engagement. Complex systems with multiple parts? High dropout. The sweet spot is something that works silently in the background-like a smart bottle that just sends a gentle text if a dose is missed, without demanding constant interaction.
Cost and Accessibility
Price is a huge barrier. Tenovi’s device costs $149 upfront, plus $30 a month. That’s more than some monthly generic prescriptions. MEMS AS is used mostly in clinical trials-not for everyday patients. Wisepill’s blister packs cost $50 per week in refill fees. For someone on a fixed income, that’s not an option.Insurance coverage is even worse. Only 38% of Medicare Advantage plans pay for remote therapeutic monitoring as of late 2022. Most patients pay out of pocket. And independent pharmacies? Only 18% have adopted any kind of digital tracking system. Big chains like CVS and Walgreens are moving faster, but they’re still figuring out how to make it profitable.
Integration Is Everything
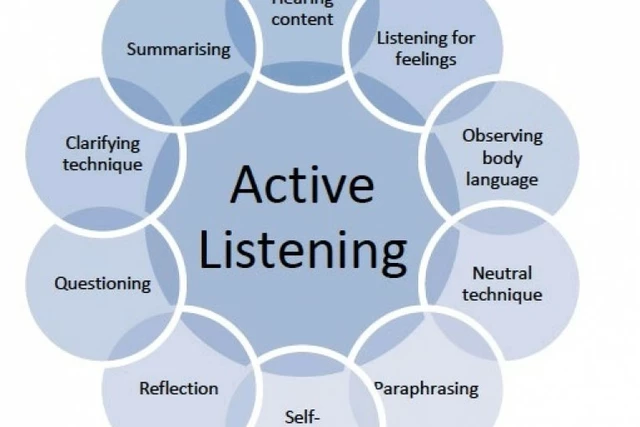
The best tools don’t just track-they connect. Systems that link directly to EHRs like Epic or Cerner, and can send alerts to pharmacists when a patient misses a dose, are the ones making a difference. One pharmacist in Melbourne told me she started checking her dashboard every morning before opening. If she saw a patient hadn’t picked up their blood pressure med in 10 days, she’d call them. Not to scold. Just to ask, "Is everything okay?"That’s the magic. It’s not the tech. It’s the human response it enables. When a pharmacist knows who’s struggling, they can adjust doses, switch to a simpler regimen, or just offer support. That’s where adherence tracking becomes meaningful-not as a surveillance tool, but as a safety net.
What’s Next?
The FDA released draft guidance in early 2023 to standardize how these tools are tested. That’s a big deal. Right now, anyone can build an app that says "I track adherence"-but few can prove it. The new standards could force out the junk and elevate the good ones.AI is also starting to play a role. CVS Health ran a pilot using machine learning to predict which patients are most likely to stop their meds. They found patterns: people who refill early, skip doses on weekends, or stop after a hospital stay. The system flagged them before they even missed a dose. Then pharmacists reached out. Result? 22% fewer dropouts.
And in 2025, CMS is tightening its Star Ratings for Medicare Advantage plans. Higher adherence scores mean more money for insurers. That’s driving hospitals and pharmacies to invest-not because it’s nice, but because it pays.
The Real Challenge
The biggest problem isn’t technology. It’s trust. Patients don’t want to be monitored. They want to be helped. Tools that feel like punishment fail. Tools that feel like support succeed.One patient with hypertension told me: "I didn’t care about the app. I cared that my pharmacist remembered my name and asked if I was sleeping okay. The pillbox just made it easier for her to know when to ask."
That’s the future. Not smarter boxes. Smarter conversations-enabled by data, not replaced by it.
What Should You Do?
If you’re a patient taking generics for a chronic condition:- Ask your pharmacist if they use any digital tracking tools.
- Don’t assume the app on your phone counts-it’s not the same as a system that verifies actual ingestion.
- Look for tools that require minimal effort. A simple text reminder is better than a complex device you forget to charge.
- If you’re uncomfortable with monitoring, say so. There are low-tech options: pill organizers with alarms, weekly refill checks, or even a family member helping out.
If you’re a pharmacy owner or staff member:
- Start small. Pick one chronic condition-hypertension or diabetes-and pilot one tool with 10-15 patients.
- Train staff to use the data as a conversation starter, not a report card.
- Look for systems that integrate with your existing software. No one needs another log-in.
- Track outcomes, not just adherence rates. Are hospital visits dropping? Are refills becoming more consistent?
Adherence tracking for generics isn’t about control. It’s about connection. The right tool doesn’t just record when a pill is taken. It reminds someone that someone cares enough to notice when they stop taking it.
Do digital adherence tools really improve generic medication use?
Yes-but only when they’re used correctly. Studies show tools like Tenovi and MEMS AS can improve adherence by 20-40% in patients with chronic conditions. But the biggest gains come when these tools are paired with human follow-up. A pillbox alone won’t help. A pillbox + a pharmacist calling to check in? That’s what changes outcomes.
Are these tools covered by insurance?
Very rarely. As of 2023, only about 38% of Medicare Advantage plans cover remote therapeutic monitoring for adherence. Most patients pay out of pocket. Some pharmacy chains offer subsidies for high-risk patients, but it’s not standard. Always ask your pharmacist or insurer before buying a device.
What’s the cheapest way to track generic medication adherence?
The cheapest effective method is a simple pill organizer with a daily alarm, combined with a weekly check-in from a family member or pharmacist. Many pharmacies offer free refill reminders via text or phone. While not as precise as smart devices, they’re far more affordable and still improve adherence by 15-25% for many patients.
Can these tools be used for multiple medications at once?
Yes. Systems like Tenovi and Wisepill are designed for polypharmacy-tracking up to six or more medications in one device. MEMS AS can monitor multiple bottles synced to one app. The key is choosing a system that matches your regimen complexity. If you’re on five or more daily pills, a smart pillbox is worth considering. For one or two meds, a basic app or reminder system may be enough.
Do these tools protect my privacy?
It depends. Clinical-grade systems like MEMS AS and Wisepill follow HIPAA rules and encrypt data. Consumer apps? Many don’t. A 2022 study found 78% of medication apps didn’t clearly explain how data was used or shared. Always check the privacy policy. Ask your pharmacy if they use a secure, regulated platform. If they can’t tell you, it’s a red flag.
How do I know if a digital adherence tool is right for me?
Ask yourself three things: 1) Do I forget doses often? 2) Am I comfortable with technology? 3) Would I want someone to know if I missed a pill? If you answered yes to #1 and #2, a smart device might help. If you’re uncomfortable with monitoring, try low-tech options like a pill organizer with alarms or weekly check-ins. The goal isn’t perfection-it’s consistency. Pick the tool that fits your life, not the other way around.



Sarah Mailloux
My grandma uses a Tenovi box and honestly? It saved her life. She’s 82, forgets everything, but that little box beeps and lights up and she takes her pills. No phone needed. She doesn’t even know what Bluetooth is. Just the green light says ‘you’re good.’
Pharmacists should hand these out like candy for high-risk patients. Why make people jump through hoops when a $150 box stops ER visits that cost $10k?
Nilesh Khedekar
Oh please. Another tech bro solution for a problem caused by corporate greed. Generic drug makers don’t give a damn about adherence because they’re making pennies per pill. The real fix? Make brand-name drugs affordable. Stop letting pharma jack up prices so high that patients choose between insulin and rent.
Smart bottles? Cute. Meanwhile, my cousin in Texas is splitting his 50mg Lisinopril pills in half because the $120 monthly generic is ‘too expensive.’ No app fixes that. Only policy does.
Amy Ehinger
I work at a community pharmacy and we tried MEMS bottles last year. We had maybe 12 patients on them. Half of them stopped using them after two weeks because they’d leave the bottle on the counter while they went to the bathroom and then forgot to open it. The system thought they missed the dose, sent a text, and they got annoyed.
Turns out, people don’t want to be tracked-they want to be reminded in a way that doesn’t make them feel like a lab rat. The best tool we found? A simple printed chart with checkboxes and a weekly call from the tech assistant. Low tech, high trust. And guess what? Adherence went up 20%.
It’s not about the gadget. It’s about who’s on the other end of the call.
Ayush Pareek
As someone from India where generics are the only option for 90% of the population, I’ve seen this play out differently. We don’t have smart pillboxes. We have grandmas who set alarms on their ₹200 Nokia phones. We have siblings who text each other: ‘Did you take your blood pressure pill?’
What works here isn’t tech-it’s community. A neighbor checking in. A cousin calling. A pharmacist who remembers your kid’s name.
These tools? Great if you can afford them. But let’s not pretend they’re the answer for the global south. Real innovation means making human care scalable, not just making gadgets.
Nat Young
Let’s be real-this whole ‘adherence tracking’ thing is just Big Pharma’s way of getting more data to sell to insurers and employers. You think they care if you take your meds? No. They care if you don’t die before your insurance premium goes up.
And don’t get me started on ‘AI predicting dropouts.’ That’s just algorithmic discrimination. You flag someone who skips doses on weekends? They’re probably working two jobs. Or caring for a sick parent. Or depressed. Not ‘noncompliant.’
This isn’t healthcare. It’s surveillance capitalism wrapped in a white coat.
ellen adamina
I’ve been on 6 different meds for 8 years. I’ve tried every app, every smart bottle, every pillbox. The only thing that kept me on track was when my pharmacist wrote me a handwritten note: ‘I noticed you missed your last refill. Everything okay? I’m here if you need to talk.’
That’s it. No tech. No data. Just someone who noticed.
Maybe the real innovation is training pharmacists to be human again.
RUTH DE OLIVEIRA ALVES
It is imperative to acknowledge that the current regulatory landscape surrounding digital therapeutic adherence tools remains profoundly fragmented. While the FDA’s draft guidance represents a commendable step toward standardization, the absence of mandatory interoperability protocols with EHR systems continues to impede scalable implementation.
Furthermore, the lack of federal reimbursement mandates for remote therapeutic monitoring under Medicare Part D constitutes a systemic failure of policy architecture. Until such mechanisms are codified, adoption will remain confined to affluent urban centers, exacerbating health inequities rather than mitigating them.
One must not confuse technological novelty with therapeutic efficacy. The data is clear: human connection remains the most potent adherence enhancer.
Diane Hendriks
Let me tell you something. The reason Americans don’t take their meds? Because they’re lazy. They want everything handed to them. A pillbox? Too much work. A reminder? Too much effort. They’d rather die than take responsibility for their own health.
And now we’re supposed to pay for fancy gadgets so they can feel better about being irresponsible? No. The solution is simple: stop subsidizing bad choices. If you don’t take your pills, you don’t get your next refill. Period.
It’s not the tech that’s broken. It’s the culture.
Crystel Ann
I just wanted to say thank you for writing this. I’m a nurse and I’ve seen patients cry because they can’t afford their meds, then feel guilty because they ‘failed’ to take them. The guilt is real.
One woman told me, ‘I take my pills when I have money. When I don’t, I feel like a failure.’
That’s not noncompliance. That’s survival. We need systems that meet people where they are-not punish them for being poor.
Jami Reynolds
Did you know that 70% of these ‘smart’ devices transmit unencrypted data? And that many of them sell anonymized usage data to third-party advertisers? You think your pill-taking habits are private? They’re being sold to marketing firms who then target you with ads for weight loss supplements, antidepressants, and even funeral plans.
This isn’t healthcare. It’s a data harvesting scheme disguised as a wellness tool. The FDA doesn’t regulate the data. The FTC doesn’t care. And your pharmacy? They’re getting kickbacks.
Don’t trust the tech. Trust nothing.
Niki Van den Bossche
Ah, the romanticization of the ‘human touch.’ How quaint. As if empathy is some magical elixir that can cure systemic neglect. You speak of pharmacists calling patients-yes, beautiful, poetic, and utterly unsustainable in a system where one pharmacist serves 1,200 patients daily.
The real tragedy isn’t the lack of human connection-it’s the failure to engineer scalable, dignified systems that don’t rely on the emotional labor of overworked professionals. We don’t need more calls. We need better infrastructure. Less sentiment. More engineering.
And if you think a handwritten note fixes Medicare’s broken reimbursement model, you’re not a healer-you’re a poet with a clipboard.
Nicholas Urmaza
Just use a pill organizer with a cheap alarm. Done.