Every year, over 1.5 million people in the U.S. are harmed by medication errors. Many of these aren’t accidents-they’re preventable. Whether you’re taking pills at home or a nurse is handing you medicine in the hospital, mistakes happen because systems are broken, not because people are careless. The good news? We know exactly how to fix them.
What Counts as a Medication Error?
A medication error isn’t just taking the wrong pill. It’s any mistake that happens while a drug is being prescribed, dispensed, administered, or monitored. That includes:- Giving the wrong dose-too much or too little
- Giving the wrong drug, even if it’s close in name (like Celebrex vs. Celexa)
- Missing a dose entirely
- Not checking for dangerous interactions (like mixing blood thinners with certain painkillers)
- Using expired or fake medications bought online
The World Health Organization calls this a global crisis. In hospitals alone, 400,000 patients suffer preventable harm each year in the U.S. And at home? Older adults on five or more medications are 38% more likely to make a mistake. Most errors happen because the system doesn’t support the person taking the meds-it expects them to be perfect.
How Hospitals Are Fighting Back (And Where They’re Still Failing)
Hospitals have tools that work-but only if they’re used right.Barcode Medication Administration (BCMA) is one of the most effective. Nurses scan a patient’s wristband and the drug’s barcode before giving any medication. In one 2025 study, this cut wrong-drug errors by over 56% and missed doses by 67%. Sounds perfect, right? But here’s the catch: in a 2024 survey of 1,200 hospital pharmacists, 57% said new errors popped up because staff started skipping scans or scanning multiple drugs at once to save time.
Computerized Physician Order Entry (CPOE) systems help too. When doctors type orders instead of scribbling on paper, errors drop by half. But too many pop-up alerts? Clinicians start ignoring them. One 2024 study found 42% of providers bypass medication alerts just to keep moving. That’s called alert fatigue-and it’s deadly.
The real winner? Medication reconciliation. That’s when a pharmacist sits down with a patient at every transition-admission, transfer, discharge-and asks: “What are you really taking?” Not what’s on the chart. Not what the nurse remembers. What’s in their actual medicine cabinet. When done well, this cuts adverse events by up to 50%. But in most hospitals, discharge reconciliation is a mess. Patients leave with lists that don’t match what they were told to take.
Why Home Medication Errors Are Even More Dangerous
Hospitals have scanners, pharmacists, and double-checks. Homes? Not so much.Think about a 78-year-old with diabetes, high blood pressure, arthritis, and heart trouble. That’s five or six pills, three times a day. Maybe a cream. Maybe vitamins. Maybe a pill organizer with 28 compartments. Now imagine their vision is fading, their hands shake, and they’re tired. They pick up the wrong container. They take two instead of one. They skip a dose because they think they already did it.
A 2024 study found 89% of home medication errors happen in people 75+ on five or more drugs. The biggest problem? Confusion between pill containers. 63% of users said they mixed up their weekly organizers. Even “smart” pill dispensers with alarms don’t help much if the labels are tiny or the alarms go off at the wrong time.
And then there’s the online pharmacy problem. The WHO says 95% of websites selling prescription drugs are illegal. They look legit-maple leaves, “Canada Pharmacy,” secure-looking logos. But they’re selling fake insulin, expired antibiotics, or pills with no active ingredient at all. One patient in Manchester took a “generic” blood thinner from a site like that. Three weeks later, they had a stroke. The pill had zero active drug.

What Actually Works to Prevent Errors
It’s not about buying fancy gadgets. It’s about changing how things are done.In hospitals:
- Use BCMA-but only after training. Staff need 16-20 hours of hands-on practice, not a 30-minute PowerPoint.
- Reduce alert fatigue. Don’t bombard staff with 50 pop-ups per patient. Prioritize high-risk alerts: anticoagulants, insulin, opioids.
- Put pharmacists at the center of transitions. They’re the only ones trained to catch hidden interactions.
- Don’t just document meds-verify them. Ask patients to show their actual pills.
At home:
- Simplify the regimen. If someone’s on more than three doses a day, talk to their doctor. Can any pills be combined or eliminated?
- Use single-dose packaging. Pharmacies can pre-sort pills into daily packets. This cuts errors by 28%.
- Get weekly check-ins. A 2023 study showed that a 15-minute call from a pharmacist every week reduces home errors by 37%.
- Keep a written list. Not on a napkin. On paper. In a wallet. Include every pill, supplement, cream, and herbal tea. Bring it to every appointment.
- Never buy meds online unless it’s a licensed pharmacy. Check the NABP’s VIPPS seal. If it doesn’t have one, don’t trust it.
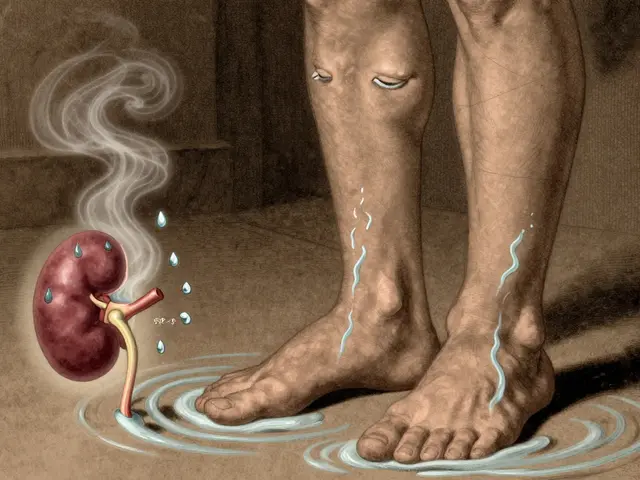
The Hidden Danger: High-Alert Medications
Not all drugs are equal. Some are like loaded guns.Insulin, heparin, warfarin, opioids, and IV potassium are called “high-alert medications.” They’re safe when used right-but deadly if mistimed or overdosed. In 2024, the FDA found these six drugs caused 62% of all severe medication errors in hospitals.
Here’s what helps:
- Insulin: Always use a calibrated syringe or pen. Never guess the dose.
- Warfarin: Get blood tests every 2-4 weeks. Even small changes in diet or other meds can throw it off.
- Opioids: Never take more than prescribed. Never mix with alcohol or sleep aids.
AI is starting to help here. Johns Hopkins tested a system that flagged dangerous prescriptions before they were written-and cut high-risk errors by 53%. But it’s not magic. It needs good data and trained staff to respond.
What’s Next? The Future of Medication Safety
The tools are getting smarter. Blockchain is being tested to track every pill from manufacturer to patient, so fake drugs can’t slip through. AI can now predict which patients are most likely to make an error based on their history, habits, and even their phone usage patterns.But none of this matters if we keep treating safety like a tech problem instead of a human one. Technology can’t fix a culture where nurses feel rushed, doctors don’t talk to pharmacists, or patients are too scared to ask, “Wait, is this right?”
The real solution? Listen to the people who use the system every day. Nurses. Pharmacists. Patients. Grandparents. They know where the cracks are. The WHO’s goal-to cut preventable harm by 50% by 2025-is possible. But only if we stop blaming the person who took the wrong pill, and start fixing the system that let it happen.
Frequently Asked Questions
What’s the most common medication error at home?
The most common error is taking the wrong dose or at the wrong time, especially among people 75+ on five or more medications. Confusion between pill organizers is the top reason-63% of users report mixing up containers, even when they’re labeled.
Can barcode scanning really reduce hospital errors?
Yes. Studies show barcode scanning reduces dispensing errors by up to 44%, wrong drug errors by 57%, and missed doses by 67%. But it only works if staff are trained properly and don’t find workarounds. If scanning becomes a burden, people skip it-and errors come back.
Are online pharmacies safe?
Almost all are not. The WHO estimates 95% of online pharmacies selling prescription drugs are illegal. Many fake sites use Canadian flags or “.ca” domains to look trustworthy. Always check for the VIPPS seal from the National Association of Boards of Pharmacy. If it’s not there, don’t buy.
What should I bring to my doctor’s appointment about my meds?
Bring a written list of everything you take: prescription drugs, over-the-counter pills, vitamins, supplements, and even herbal teas. Include the dose and how often you take it. Also bring the actual bottles if you can. This helps your doctor spot duplicates, interactions, or expired meds.
How can I help an elderly relative avoid medication errors?
Start by simplifying their regimen. Ask their doctor if any meds can be combined or stopped. Use single-dose packaging from the pharmacy. Set up a weekly 15-minute call with a pharmacist to review their list. And never let them manage pills alone-check in regularly. Even small help cuts errors by 37%.
Why do hospitals keep making the same medication errors?
Because they focus on technology, not teamwork. Scanners and computers help, but if nurses are overworked, doctors don’t communicate with pharmacists, and staff aren’t trained to speak up when something looks wrong, errors will keep happening. Safety isn’t a gadget-it’s a culture.





Karen Ryan
Just had my grandma’s med organizer reorganized by her pharmacist last week - 28 compartments, 6 meds, and she was taking insulin at breakfast instead of dinner. 😅 Life-changing. Single-dose packs are a godsend. Why isn’t this standard everywhere?
Kaylee Crosby
My mom’s on 8 meds and I swear she forgets half of them. We started doing those weekly 15-min pharmacist calls and wow - she’s not mixing up her blood pressure pills with her thyroid ones anymore. Seriously, if your loved one’s over 70 and on more than 5 meds, just call a pharmacist. It’s free. It saves lives. 🙌
Valérie Siébert
BCMA is the future but nobody trains nurses like humans anymore - they train them like robots who scan and move on. I worked in a hospital where the barcode scanner beeped 400 times a shift. Nurses started scanning the same barcodes twice just to get it over with. Tech doesn’t fix culture. Culture fixes tech. Stop treating nurses like disposable cogs.
Terry Bell
Man, I get why people take fake meds online. My cousin bought ‘generic’ metformin from a site that looked like it was run by a Canadian grandma with a Shopify store. Cost $12. Real pharmacy? $87. He got sick for three weeks. Turns out the ‘metformin’ was just lactose and glitter. 😭 But here’s the thing - we don’t fix this by scolding people. We fix it by making real meds affordable and accessible. It’s not about being dumb. It’s about being broke.
Dirk Bradley
It is an incontrovertible fact that the erosion of clinical judgment - exacerbated by algorithmic over-reliance and the commodification of healthcare delivery - has precipitated a systemic collapse in pharmacological safety. The deployment of technological panaceas without concurrent investment in human capital constitutes not innovation, but institutional negligence of the highest order.
Mariam Kamish
They say ‘don’t buy meds online’ but no one tells you that your insurance won’t cover your insulin unless you jump through 17 hoops. So yeah, I’ll take my $15 fake pill from a site with a Canadian flag. At least I’m alive. 🤡
Emma Hanna
People need to STOP being lazy. If you can’t read the label, get glasses. If you can’t remember your meds, get a calendar. If you can’t afford your pills, apply for assistance. Don’t blame the system. Blame yourself. And stop buying junk from sketchy websites. It’s not rocket science.
Lawrence Zawahri
They’re hiding the truth. The FDA and big pharma are in bed with these online pharmacies. They want you dependent on fake drugs so they can keep selling you more. That ‘VIPPS seal’? A scam. They’re all owned by the same 3 corporations. They want you sick. They want you scared. They want you paying $500 for insulin while you’re buying ‘Canadian’ pills from a guy in Belarus. Wake up.
Benjamin Gundermann
Look, I get it - hospitals are broken. But let’s be real: most of these errors happen because people can’t read. I’ve seen grandma’s handwritten list with ‘asprin’ and ‘tylenol’ and ‘that blue one for the heart’. No wonder she’s confused. Stop blaming the system. Start teaching people how to read. And why is no one talking about how most of these meds are just sugar pills anyway? Big Pharma’s been milking this for decades.
Manish Pandya
My uncle in Delhi takes 12 pills a day. His daughter prints out a color-coded chart with pictures of each pill. She uses WhatsApp to remind him. No fancy tech. Just love and a phone. Simple works. We don’t need AI. We need families who care.
Adesokan Ayodeji
Man, I’ve been a nurse for 22 years and I’ve seen it all - from barcode scanners that don’t work to pharmacists who’ve been yelled at for asking too many questions. But here’s what I know: when a pharmacist actually sits down with a patient and says, ‘Show me your pills,’ magic happens. Not because of tech. Because of human connection. I had a guy who thought he was taking blood pressure meds - turns out he was taking his dog’s heartworm pill. He didn’t know the difference. We laughed. Then we cried. Then we fixed it. That’s what matters. Not the system. Not the alerts. Us. We’re the system. Let’s stop pretending we’re not.
Patrick Goodall
AI predicting errors? LOL. They’re just using your phone data to sell you more meds. You think your smart pill dispenser is helping? Nah. It’s feeding your habits to a data broker who’s selling your ‘medication noncompliance profile’ to insurers. Next thing you know, your premiums go up because you ‘missed’ a dose you never even got. They’re not fixing the system - they’re monetizing your fear. 💀
Caroline Marchetta
Oh, so now we’re blaming patients for taking fake meds? How about we blame the $1,000 insulin co-pay? Or the 3-hour wait to see a pharmacist? Or the fact that my grandma’s ‘medication reconciliation’ was done by a student intern who didn’t speak English? We’re not failing because people are dumb. We’re failing because we’ve turned healthcare into a horror show with bad lighting and no empathy. And I’m tired of pretending it’s not.
Jack Riley
What if the real error isn’t the pill - but the idea that we should be taking so many? What if the system isn’t broken… it’s just trying to keep us alive in a world that’s designed to make us sick? We treat symptoms like enemies instead of signals. Maybe the answer isn’t more scanners… but fewer pills. Maybe we need to ask: why are we all so sick? And why are we being sold solutions that cost more than our rent?
Rachelle Baxter
As a certified medication therapy management specialist with a Ph.D. in Clinical Pharmacology from Johns Hopkins, I must emphasize that the WHO’s 50% reduction target is statistically unattainable without mandatory pharmacist-led reconciliation protocols, standardized nomenclature across EHRs, and federal funding for single-dose packaging infrastructure. Until then, anecdotal ‘weekly calls’ are merely feel-good noise. Please stop romanticizing amateur interventions. Evidence-based practice is not optional.