Getting your medication schedule right isn't just about setting an alarm. It's about understanding what's written on the label - and using that information to build a reminder system that actually keeps you safe. Too many people set generic alarms for their pills, like "8 AM and 8 PM," and miss the finer details that make a real difference. That’s where medication labels come in. They’re not just instructions. They’re your personal safety manual.
What’s Really on Your Medication Label?
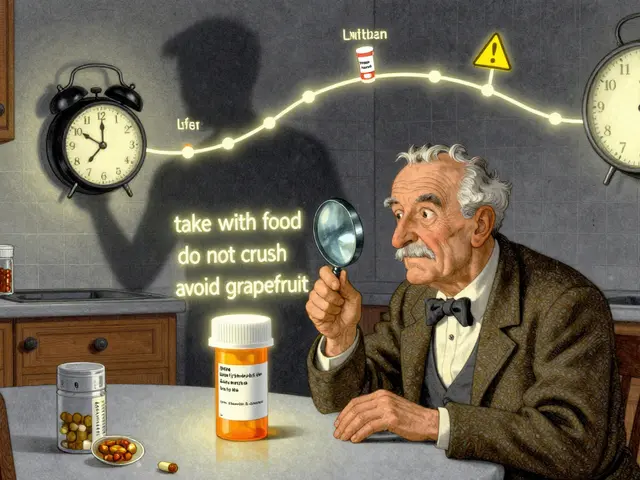
Your prescription label contains more than just your name and the pharmacy’s number. It holds critical data that determines when, how, and even why you should take each pill. The FDA requires labels to include specific details: the name of the drug, the exact dose (like 10 mg or 500 mg), how often to take it ("take one tablet every 8 hours"), whether to take it with food or on an empty stomach, and warnings about interactions with other medications or substances like alcohol.
But here’s the problem: most people glance at the label and assume they got it. A 2023 NIH study found that nearly 8 out of 10 timing-related medication errors happen because the reminder system ignored these details. For example, if your label says "take with food," but your app just pings you at 7 AM and 7 PM, you might end up taking it on an empty stomach - which can reduce effectiveness or cause stomach upset. Or worse, if you’re taking two drugs that shouldn’t be within two hours of each other, and your reminder app doesn’t know that, you could be risking a dangerous interaction.
Why Basic Alarms Fail
Simple alarm apps - the kind that just buzz at fixed times - are easy to use. But they’re blind to the nuances of your meds. They don’t know if your antibiotic needs to be spaced exactly 12 hours apart. They don’t know that your blood pressure pill works best if taken right after breakfast. They don’t know that your cholesterol drug can’t be taken with grapefruit juice.
A 2024 analysis of 12 popular medication apps found that those ignoring label details had over 60% more timing errors than apps that used label data. Apps like Medisafe and MyTherapy, which read and interpret label text, cut those errors by more than half. Why? Because they don’t just say "take now." They say "take one tablet with breakfast, then again 8 hours later, but not before 10 AM because of your other med." That kind of precision matters.
How to Turn Label Info Into Smart Reminders
Here’s how to do it yourself - whether you’re using an app or just organizing your routine manually.
- Read every line. Don’t skip the small print. Look for phrases like "take on an empty stomach," "do not crush," or "avoid dairy products." These aren’t suggestions - they’re instructions that affect absorption and safety.
- Identify the dosing pattern. If it says "take every 8 hours," that means three times a day, spaced evenly - not just at 8 AM, 4 PM, and midnight. You need roughly 8 hours between doses. A 7 AM, 3 PM, and 11 PM schedule works better than 8 AM, 4 PM, 12 AM.
- Check for interactions. If you’re on more than one medication, look for warnings like "take at least 2 hours before or after [other drug]." This is crucial. For example, if you take iron and a thyroid pill, taking them too close together can make both less effective.
- Map it to real life. Don’t just set alarms based on clock time. Set them around your routine. "Take with breakfast" means when you sit down to eat, not at 7:30 AM sharp. Use cues you already follow: brushing teeth, eating lunch, going to bed.
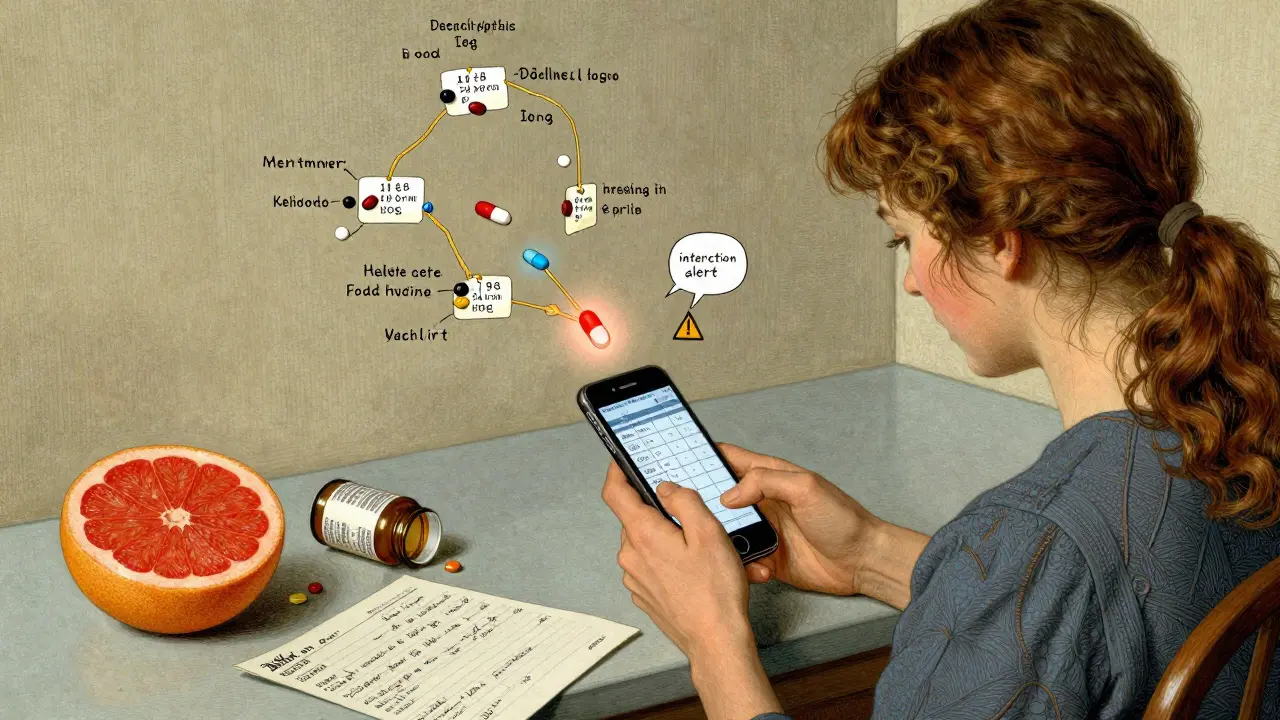
- Use an app that reads labels. Apps like Medisafe, MyTherapy, and CareZone let you scan or manually enter your label info. They then auto-generate reminders with correct intervals and interaction alerts. Some even show you a visual timeline of your whole day’s schedule.
The Power of the Universal Medication Schedule (UMS)
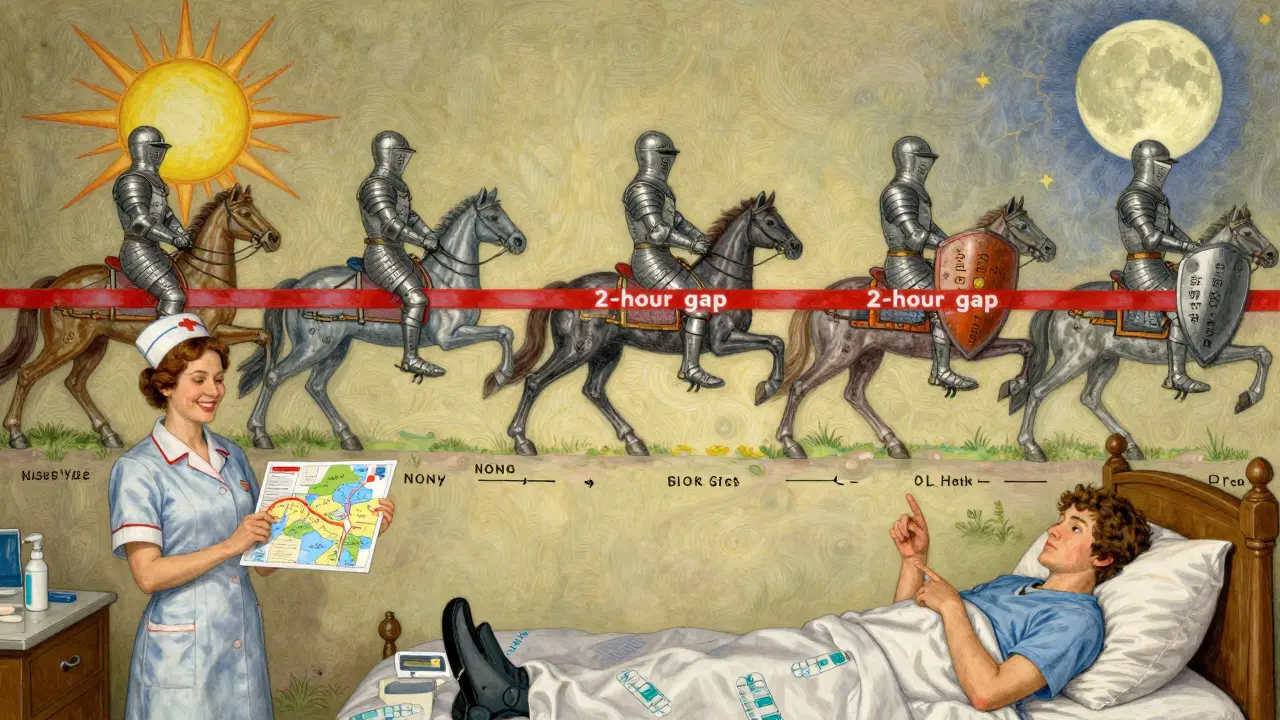
Researchers at the University of Pittsburgh developed a system called the Universal Medication Schedule (UMS) to standardize how label info becomes reminders. It uses two key rules:
- MTCOD (Medication Time Constraint with One Drug): The minimum time between doses of the same drug. For example, if your label says "every 6 hours," MTCOD = 6 hours. No dose should be taken sooner.
- MTCMD (Medication Time Constraint with Multi-Drug): The minimum time between different drugs that interact. For example, if your label says "take Warfarin at least 2 hours before Calcium supplements," MTCMD = 2 hours.
Apps that use UMS logic don’t just guess. They calculate. If you’re taking five medications, they’ll map out a schedule that avoids conflicts, respects intervals, and fits your daily rhythm. In a 2024 study, patients using UMS-based apps had 82.4% adherence rates - far higher than those using basic alarms.
What Happens When Labels Are Ignored?
Ignoring label info isn’t just inconvenient - it’s dangerous.
The FDA’s Adverse Event Reporting System found that 37.8% of overdoses in people taking multiple medications happened because their reminder app didn’t account for minimum intervals. One man took his blood thinner twice in 10 hours because his app reminded him at 8 AM and 8 PM - but his label said "do not take more than once every 12 hours." He ended up in the ER.
Another common mistake: taking antibiotics with food when the label says "on an empty stomach." That can cut the drug’s effectiveness by up to 50%, leading to treatment failure and antibiotic resistance.
And it’s not just about timing. Labels also warn about alcohol, grapefruit, antacids, and even certain foods. If your app doesn’t know that, you’re flying blind.
Real People, Real Results
Users of label-aware apps report dramatic improvements. One Reddit user wrote: "I used to miss doses because I didn’t understand why my meds had to be spaced out. The app showed me a timeline - it clicked. I haven’t missed a dose in 6 months." Another said: "My diabetes and blood pressure meds used to clash. The app flagged it and rescheduled them. My doctor was amazed I finally got it right."
On Trustpilot, CareZone users gave it a 4.7 out of 5, with many praising how it "read my label and set the right times without me having to guess." For seniors, this is huge. A 2024 AARP survey found that 76.4% of adults over 65 improved adherence when reminders included simple cues like "take with breakfast" instead of "8:00 AM."
What to Watch Out For
Even the best apps have limits.
- Ambiguous labels: About 22% of generic drug labels use unclear wording like "take as directed" or "take 1-2 times daily." These confuse even AI systems.
- Personal adjustments: Your doctor might change your schedule based on your body, diet, or other conditions. The label doesn’t know that. Always cross-check with your prescriber.
- Over-reliance on tech: A 2024 Consumer Reports review found that 14.3% of errors in digital tools came from blindly trusting automated interpretations. Always double-check the app’s schedule against your actual label.
The smartest approach? Use an app that reads your label - but keep the physical label handy. Review it once a week. If the app says "take with food" and your label says "take on empty stomach," pause. Call your pharmacist. Don’t assume the app got it right.
The Future Is Label-Driven
By 2026, all Medicare-participating health systems in the U.S. will be required to use medication reminder tools that interpret label information. Major EHR platforms like Epic and Cerner are rolling out new modules in 2025 that automatically sync your prescription label data with your digital reminders.
AI is getting better, too. In late 2024, the FDA approved the first system that uses camera vision to verify you’re taking the right pill at the right time - and it checks the label too. It’s not sci-fi anymore. It’s the new standard.
The bottom line? Your medication label isn’t just paper. It’s a code. And when you learn how to read it - and use it to build smarter reminders - you’re not just staying on schedule. You’re protecting your health.
Can I just use my phone’s alarm app for my medications?
You can, but it’s risky. Basic alarm apps don’t understand medication labels. They can’t tell the difference between "take every 8 hours" and "take with food," or warn you about interactions. A 2024 study showed these apps had over 60% more timing errors than those that use label data. For safety and effectiveness, use a dedicated medication app that reads your prescription label.
What if my label says "take as needed"?
"As needed" means you don’t take it on a fixed schedule - only when symptoms occur. Don’t set a reminder for it. Instead, note the maximum daily dose and time between doses (e.g., "no more than 3 doses in 24 hours, at least 6 hours apart"). Some apps let you set "on-demand" reminders with limits to prevent overuse. Always follow the label’s maximum limits.
Do I need to scan my label every time I get a new prescription?
Yes. Even if it’s the same drug, the dose, timing, or manufacturer may change. A new label could say "take with food" when the old one said "on empty stomach." Always update your app with the current label. Many apps let you scan a new label in seconds - use that feature every refill.
How do I know if my app is reading my label correctly?
Compare the app’s reminder schedule to your physical label. Check: Are the times spaced correctly? Does it mention food, interactions, or special instructions? If your label says "take 2 hours before dinner" but the app says "6 PM," it’s wrong. Look for a "label summary" section in the app - most good apps show you exactly what they pulled from your label. If it’s missing key info, manually correct it.
Can I use this method for over-the-counter meds too?
Absolutely. OTC meds like ibuprofen, antacids, or sleep aids also have labels with timing and interaction warnings. Taking too much ibuprofen in a day? Mixing melatonin with alcohol? These can be dangerous. Add OTC meds to your app and scan their labels too. Many apps let you add non-prescription drugs - use that feature.
If you’re managing multiple medications, the difference between a good schedule and a dangerous one comes down to one thing: paying attention to the label. Not guessing. Not assuming. Reading. And then using that information to build a reminder system that works with your life - not against it.





Joseph Charles Colin
The core insight here is that medication labels encode temporal and pharmacokinetic constraints that generic alarm apps simply cannot parse. The UMS framework-specifically MTCOD and MTCMD-isn’t just a heuristic; it’s a computational model for safe polypharmacy. When you abstract dosing intervals as discrete time windows constrained by drug-drug and drug-food interactions, you’re essentially building a constraint satisfaction problem. Apps that ingest label semantics (e.g., 'take with food' → gastric pH modulation window; 'every 8 hours' → circadian-aligned MTCOD) reduce therapeutic failure by orders of magnitude. This isn’t about reminders-it’s about dynamic pharmacodynamic orchestration.
John Sonnenberg
People are dying because they trust their phones more than their prescriptions. I’ve seen it. A man took his warfarin twice in ten hours because his app said '8 AM and 8 PM.' He bled internally. No one told him the label said 'every 12 hours minimum.' No one. And now he’s on disability. This isn’t a tech problem. It’s a systemic failure of education, oversight, and corporate negligence. The FDA should mandate label-to-app sync. Now.
Joshua Smith
This is really helpful. I’ve been using Medisafe for a few months now, and I didn’t realize how much I was missing until I read this. I used to just set alarms for 'take pill' without thinking about food or spacing. Now I scan the label every time I refill, and the app shows me a little summary of why the timing matters. It’s small, but it makes me feel more in control. Thanks for breaking it down so clearly.
Jessica Klaar
I’m a caregiver for my mother, who’s on seven different meds. I used to set alarms on her phone, but they kept clashing-especially with her blood pressure and thyroid pills. Then I switched to CareZone, scanned every label, and it auto-generated a color-coded timeline. Now she takes everything at the right time, with food or without, and even remembers not to drink grapefruit juice. It’s not magic-it’s just listening to the label. I wish every pharmacy gave this kind of guidance out of the box.
PAUL MCQUEEN
Look, I get it. Labels are important. But let’s be real-how many people actually read the fine print? Most just look at the dose and the time. And apps? Half of them misread 'take with food' as 'take after breakfast' and ignore 'avoid dairy.' This whole system is built on the assumption that people care enough to be precise. They don’t. We’re not all medical students. Maybe instead of over-engineering reminders, we should just simplify the labels. Or make them bigger. Or have pharmacists explain them. Not every 70-year-old is gonna scan a QR code.
glenn mendoza
It is with profound gratitude that I acknowledge the meticulous research and thoughtful articulation presented in this piece. The integration of pharmacological science with digital health infrastructure represents a paradigm shift in patient safety. The Universal Medication Schedule, grounded in empirical data and clinical logic, is not merely a tool-it is a moral imperative. I commend the authors for elevating this discourse beyond convenience and into the realm of ethical healthcare delivery. May this become standard practice across all healthcare systems.
Kathryn Lenn
Of course the FDA is pushing this. What’s next? Mandatory app scans before you breathe? They’ve been quietly turning every pill into a surveillance device. You think your app is helping you? It’s logging every dose, every interaction, every meal you eat with it. And who owns that data? Big Pharma. The same companies that made the drugs in the first place. This isn’t safety-it’s behavioral control wrapped in a ‘helpful’ UI. Wake up. The label is the last thing you can trust. The app? It’s a Trojan horse.
John Watts
You know what’s beautiful about this? It’s not about tech. It’s about dignity. When you take the time to read the label, to understand why your meds need spacing, to care enough to scan it into an app-you’re saying, 'I matter.' I’ve seen seniors who thought 'take as needed' meant 'whenever I feel like it.' Now they’re using the app, setting reminders around their coffee routine, their walk, their TV show. They’re not just taking pills. They’re reclaiming control. And that? That’s the real win. You don’t need a PhD. You just need to read the damn label-and then let the app do the math. You’ve got this.