Combination Therapy Safety Checker
Check Your Combination Safety
Select your specific medications to see if this combination is safe based on current medical guidelines.
Select medications and click "Check Safety" to see results.
Combining beta-blockers and calcium channel blockers might sound like a smart way to tackle high blood pressure or angina-after all, they work in different ways, right? But this combo isn’t as simple as tossing two pills into a bottle. When used together, they can either save a life or trigger a cardiac crisis, depending on which drugs you pick and who’s taking them.
How These Drugs Work-And Why They’re Often Combined
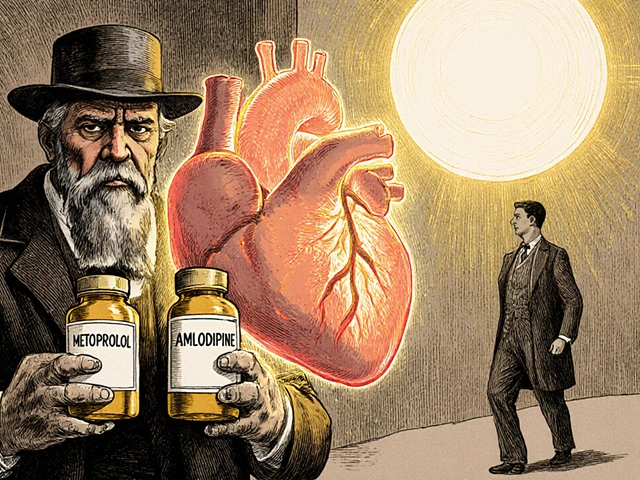
Beta-blockers, like metoprolol and atenolol, slow your heart rate and reduce the force of each heartbeat by blocking adrenaline. This lowers blood pressure and eases chest pain. Calcium channel blockers, such as amlodipine and diltiazem, relax your blood vessels by stopping calcium from entering heart and artery cells. This also lowers pressure and improves blood flow.
Doctors reach for this combo when one drug isn’t enough. For example, someone with high blood pressure and frequent angina might need both: the beta-blocker to reduce heart strain during activity, and the calcium channel blocker to widen arteries and stop spasms. It’s not about doubling down-it’s about covering two different pathways to the same goal.
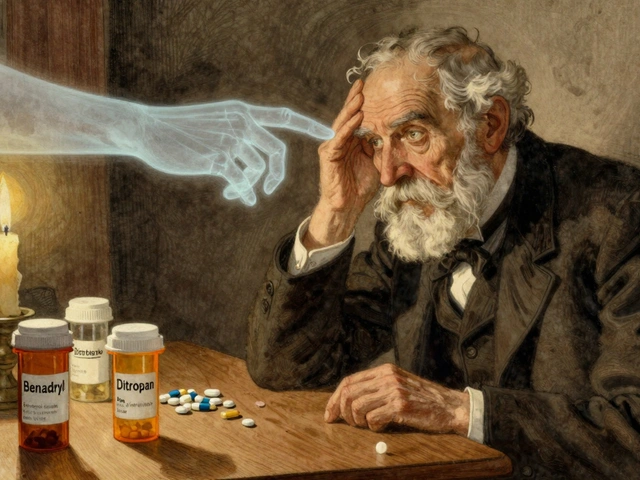
The Big Divide: Dihydropyridines vs. Non-Dihydropyridines
Not all calcium channel blockers are the same. There are two main types, and mixing them with beta-blockers has wildly different outcomes.
Dihydropyridines-like amlodipine and nifedipine-mostly act on blood vessels. They barely touch the heart’s electrical system. That’s why beta-blocker + amlodipine is the most commonly used and safest combo. Studies show it lowers blood pressure better than either drug alone, with minimal risk to heart rhythm. In fact, a 2023 study of nearly 19,000 patients found this combo cut stroke risk by 22% and heart failure risk by 28% compared to other dual therapies.
Non-dihydropyridines-verapamil and diltiazem-are a different story. They directly slow down the heart’s electrical signals. Combine them with a beta-blocker, and you’re stacking two drugs that suppress heart rate and conduction. The result? Dangerous drops in heart rate, prolonged PR intervals on ECGs, and sometimes complete heart block.
One study found that 10-15% of patients on verapamil plus a beta-blocker developed serious bradycardia or heart block requiring emergency care. In elderly patients, the risk of needing a pacemaker jumped 3.2 times compared to those on beta-blocker + amlodipine.
Who Should Avoid This Combo?
Some people should never get this combo. The European Society of Cardiology guidelines are clear: avoid verapamil or diltiazem with beta-blockers if you have:
- Sinus node dysfunction (sick sinus syndrome)
- Second- or third-degree heart block
- PR interval longer than 200 milliseconds
- Heart failure with reduced ejection fraction (HFrEF)
Even if you don’t have a diagnosed condition, risk goes up with age. One study found that 15% of patients over 75 had undiagnosed conduction problems-silent until the combo was started. That’s why doctors now require an ECG and echocardiogram before prescribing this mix.
Real-World Risks and Patient Stories
Behind the numbers are real people. A Reddit thread from February 2023 featured a cardiologist who lost a patient to complete heart block after adding verapamil to metoprolol. The patient was 82, had a borderline PR interval, and no prior symptoms. The doctor now refuses to use this combo in older adults.
On the flip side, a Massachusetts General Hospital clinician reported treating over 200 patients with metoprolol and amlodipine. Only 3% developed ankle swelling-manageable by lowering the amlodipine dose. No one needed a pacemaker. That’s the difference between the two combos.
And it’s not just heart rate. Beta-blocker + verapamil increases the risk of severe fatigue, dizziness, and fainting. One study showed 18.7% of patients on this combo stopped taking their meds due to side effects-more than double the rate of those on beta-blocker + amlodipine.
What About Side Effects?
Even the safer combo isn’t side-effect free. Ankle swelling (peripheral edema) is common with dihydropyridines like amlodipine. About 22% of patients on beta-blocker + amlodipine get it, compared to 16% on other combinations. It’s not dangerous, but it’s annoying-and often leads to patients thinking they’re allergic to the drug.
Other side effects include:
- Low heart rate (below 50 bpm)
- Low blood pressure causing lightheadedness
- Worsening fatigue or depression
- Cold hands and feet (from reduced circulation)
These aren’t rare. A 2022 survey of 1,247 doctors found 27% had seen unexpected bradycardia in patients on these combos, and 32% had patients quit due to swelling or tiredness.
How Doctors Decide-And What You Should Ask
There’s no one-size-fits-all. Doctors look at your age, heart function, ECG results, and other meds. If you’re 50 with high blood pressure and angina, and your heart’s working fine, beta-blocker + amlodipine is a strong option. If you’re 78 with a history of dizziness or a slow ECG, they’ll likely avoid non-dihydropyridines entirely.
Here’s what to ask your doctor:
- “Is this a dihydropyridine or non-dihydropyridine calcium blocker?”
- “Have you checked my PR interval and ejection fraction?”
- “What’s the plan if my heart rate drops too low?”
- “Are there alternatives if I can’t tolerate this combo?”
Don’t assume all calcium blockers are the same. If your prescription says “verapamil” or “diltiazem,” ask if amlodipine could be substituted. Many patients don’t realize there’s a safer option.
Monitoring and Safety Protocols
If you’re prescribed this combo, you’ll need close follow-up. Most protocols require:
- Baseline ECG before starting
- Echocardiogram to check heart pumping strength
- Weekly checks of heart rate and blood pressure for the first month
- Repeat ECG if you feel dizzy, faint, or notice your pulse is unusually slow
Tools like the European Society of Cardiology’s online bradycardia risk calculator (validated on 4,500 patients) help doctors predict who’s at risk. In systems like Kaiser Permanente, where standardized protocols were rolled out in 2020, emergency visits for this combo dropped by 44%.
Is This Combo Still Worth It?
Yes-but only in the right hands and the right patients. Beta-blocker + dihydropyridine CCB combos remain a first-line choice for people with hypertension and angina, especially if they’re under 70 and have no conduction issues. The data shows fewer heart attacks, strokes, and heart failure hospitalizations compared to other dual therapies.
But verapamil and diltiazem with beta-blockers? Those are fading fast. The FDA added a boxed warning in 2021. The EMA now requires heart function testing before prescribing. And in clinical practice, only 12% of U.S. doctors would consider it-even in select cases.
The future? More use of amlodipine-based combos, fewer verapamil ones. The trend is clear: safety over convenience. As populations age and polypharmacy grows, precision matters more than ever.
Bottom Line
Beta-blockers and calcium channel blockers can work brilliantly together-but only if you know which ones you’re using. Amlodipine + metoprolol? Often safe and effective. Verapamil + propranolol? High risk, rarely worth it. The difference isn’t just medical-it’s life or death.
If you’re on this combo, know your drugs. Ask for your ECG results. Track your pulse. And never assume two blood pressure pills are automatically safe together. The heart doesn’t care about good intentions-it only responds to what’s in your bloodstream.






Nikki C
So let me get this straight if you mix verapamil with a beta blocker you might die but amlodipine is basically chill as hell
Why does pharma even make the dangerous ones then
Alex Dubrovin
Been on metoprolol + amlodipine for 3 years
Only side effect is my socks get stained from the swelling
Worth it
Natashia Luu
It is unconscionable that physicians continue to prescribe non-dihydropyridine calcium channel blockers in combination with beta-blockers without mandatory pre-screening ECGs
The data is unequivocal
The risk of complete heart block in elderly patients is not a statistical anomaly
It is a predictable catastrophe
And yet we persist in this reckless practice
Because convenience outweighs caution
Because billing codes matter more than breaths
Because we have forgotten that medicine is not a transaction
It is a covenant
And we are breaking it
Akash Chopda
They're hiding the truth
Big Pharma wants you on two pills so you stay dependent
They know amlodipine is safer but they push verapamil because it's cheaper to produce
And your doctor doesn't care because they get bonuses for hitting BP targets
Check your ECG results
They're lying to you
Victoria Stanley
Just wanted to add that if you're on this combo and notice your pulse dropping below 50 or feeling dizzy when standing
Don't just wait it out
Take your BP and pulse
Call your doc
It's not worth the gamble
I've seen too many patients ignore early signs until they collapse
Early detection saves pacemakers
Andy Louis-Charles
My grandpa got verapamil + metoprolol and ended up in the ER with a 38 bpm
Now he's on amlodipine and feels like a new man
❤️
akhilesh jha
Interesting how the safest combo is also the most common one
But I wonder if the reason it's common is because it works
Or because the dangerous options are being quietly phased out
Like how we stopped using thalidomide
Not because we didn't know it was dangerous
But because we finally had a better choice
And the system changed
Vineeta Puri
For patients who are newly prescribed this combination, I strongly recommend maintaining a daily log of heart rate, blood pressure, and any episodes of dizziness or fatigue
Bring this log to each follow-up appointment
It empowers you to participate actively in your care
And provides your provider with objective data
Do not rely on memory
Document consistently
This is not just medical advice
It is a form of self-advocacy
Douglas cardoza
My doc just switched me from diltiazem to amlodipine last month
Woke up feeling like I could breathe again
Also stopped feeling like a zombie
Thanks for the post