Transplant Eligibility Calculator
Eligibility Criteria
Based on article guidelines for heart transplantation candidates
- Required Age under 70 years
- Required Peak VO₂ > 12 ml/kg/min
- Required Pulmonary artery pressure < 50 mm Hg
- Recommended Ejection fraction < 40%
Results
When a heart can’t pump blood effectively because the left ventricle is weak, doctors often face a tough decision: manage the symptoms or aim for a cure. Heart transplantation is a surgical procedure that replaces a failing heart with a healthy donor organ has become a lifeline for many patients with advanced Left ventricular dysfunction a condition where the left ventricle can’t contract strongly enough to circulate blood. This article breaks down why a transplant might be the right move, what the process looks like, and how outcomes stack up against other therapies.
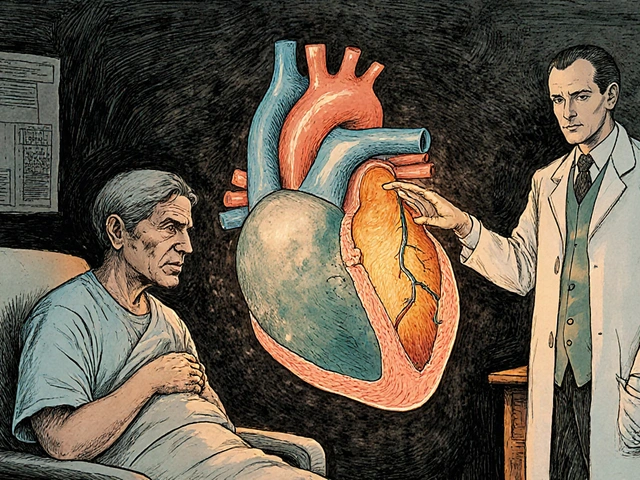
Understanding Left Ventricular Dysfunction
First, let’s get clear on the problem. The left ventricle does the heavy lifting of pushing oxygen‑rich blood out to the body. When its pumping power drops below about 40% of normal (a measure called ejection fraction), patients start feeling fatigue, shortness of breath, and fluid buildup. This state is called heart failure a clinical syndrome where the heart cannot meet the body’s metabolic demands. Left‑sided failure is the most common form and often progresses despite medication.
When Standard Therapies Aren’t Enough
Doctors usually start with lifestyle changes, ACE inhibitors, beta‑blockers, and diuretics. Devices like implantable cardioverter‑defibrillators (ICDs) and cardiac resynchronization therapy (CRT) can also help. However, about 10-15% of patients with severe left ventricular dysfunction remain symptomatic despite optimal medical therapy. At this stage, two major options emerge:
- Long‑term mechanical support, typically a ventricular assist device a pump that helps the left ventricle move blood to the rest of the body
- Definitive organ replacement via heart transplantation
Choosing between them depends on age, comorbidities, transplant eligibility, and personal goals.
The Transplant Journey: Step by Step
- Evaluation: A multidisciplinary team runs a battery of tests-echocardiogram, cardiac MRI, pulmonary function tests, and psychosocial assessments. The goal is to confirm that the left ventricle is the primary issue and that the patient can tolerate major surgery.
- Listing: Once deemed suitable, the patient is entered into the UNOS United Network for Organ Sharing, the organization that allocates donor hearts in the United States (or local equivalent). Allocation follows a scoring system that weighs urgency, blood type, and waiting time.
- Donor Matching: A compatible donor heart a heart recovered from a brain‑dead or circulatory‑determined deceased donor is identified. Matching criteria include size, blood type, and geographic proximity to limit cold‑ischemia time.
- Surgery: The recipient’s diseased heart is removed, and the donor organ is sewn in place. Surgeons typically spend 4-6 hours on the operation, with cardiopulmonary bypass supporting the body throughout.
- Post‑Op Care: Intensive monitoring, early extubation, and gradual mobilization begin immediately. The biggest hurdle is preventing rejection, which brings us to immunosuppression.
- Immunosuppression Therapy: Patients receive a lifelong cocktail-usually a calcineurin inhibitor (tacrolimus), an antimetabolite (mycophenolate mofetil), and steroids. Recent protocols add mTOR inhibitors to lower kidney toxicity.
- Rehabilitation: Structured cardiac rehab restores functional capacity. Most patients achieve a marked improvement in quality of life within 3-6 months.
While the roadmap sounds linear, real‑world cases often involve setbacks-infectious complications, renal dysfunction, or even early graft failure.
Outcomes: Survival, Quality of Life, and Risks
Data from the International Society for Heart and Lung Transplantation (ISHLT) 2023 registry provide a clear picture:
- 1‑year survival after heart transplant sits at ~90% for adults.
- 5‑year survival hovers around 75%.
- Median functional capacity improves from NYHA Class III/IV to Class I/II.
- Rejection rates have halved in the past decade due to newer immunosuppressants.
Compare that to ventricular assist devices (VADs). A 2022 meta‑analysis reported:
- 1‑year survival of 80% for continuous‑flow LVADs.
- Higher rates of bloodstream infections (30% within first year).
- Device‑related complications-pump thrombosis, driveline infections-affect up to 15% of users.
In short, a transplant offers better long‑term survival and fewer device‑related hassles, but it comes with the lifelong commitment to immunosuppression and the uncertainty of organ availability.
| Metric | Heart Transplant | Left Ventricular Assist Device (LVAD) |
|---|---|---|
| 1‑Year Survival | ≈ 90% | ≈ 80% |
| 5‑Year Survival | ≈ 75% | ≈ 60% |
| Major Infection Rate (1 yr) | ≈ 15% | ≈ 30% |
| Quality‑of‑Life (NYHA) | Improves to Class I/II | Usually remains Class II/III |
| Need for Re‑operation | Low after first year | ≈ 20% due to pump issues |
Who Benefits Most from a Transplant?
Not every patient with left ventricular dysfunction is a transplant candidate. Ideal candidates typically meet these criteria:
- Age under 70 (younger patients fare better).
- Peak VO₂ > 12 ml/kg/min on cardiopulmonary exercise testing-indicates retained functional reserve.
- Absence of irreversible pulmonary hypertension (pulmonary artery pressure < 50 mm Hg).
- Compliance with medication regimens and follow‑up visits.
- Social support network-family or caregivers who can assist during recovery.
Patients who are too frail, have active infections, or significant kidney/liver disease may be steered toward VADs or palliative care instead.
Common Myths and Misconceptions
Myth 1: Transplants are only for the very young. In reality, many centers transplant patients in their 60s with outcomes comparable to younger cohorts, provided comorbidities are controlled.
Myth 2: You’ll live forever after a transplant. While survival has improved, lifelong immunosuppression means patients remain at higher risk for infections and certain cancers.
Myth 3: A donor heart is always a perfect match. Size and blood type matching are critical, but minor differences are often acceptable. Surgeons can tailor the anastomosis to accommodate slight mismatches.
Future Directions: Bridging the Gap
Research is racing ahead on three fronts:
- Artificial hearts: The latest SynCardia 50 cc total artificial heart shows promise for patients who can’t receive a donor organ.
- Immune tolerance protocols: Gene‑editing of donor tissue to reduce antigenicity could eventually shrink or eliminate the need for chronic immunosuppression.
- Improved organ preservation: Portable normothermic perfusion systems keep donor hearts beating longer, expanding the geographic reach of viable organs.
These advances may lower the waiting‑list mortality that still affects about 10% of candidates each year.
Key Takeaways
- Left ventricular dysfunction leads to severe heart failure when ejection fraction falls below 40%.
- When medications and devices fail, heart transplantation offers the best long‑term survival and quality of life for eligible patients.
- The transplant process involves rigorous evaluation, listing, donor matching, complex surgery, and lifelong immunosuppression.
- Compared with LVADs, transplants provide higher survival rates and fewer infection‑related complications, but donor availability remains a limiting factor.
- Emerging technologies-artificial hearts, tolerance‑inducing regimens, and better preservation-could reshape the treatment landscape over the next decade.
Frequently Asked Questions
How long is the waiting period for a heart transplant?
Waiting times vary widely by region and blood type, but in the United States the median wait is 4-6 months. Patients with higher urgency scores may receive an organ in weeks.
What are the biggest risks after the surgery?
Early risks include bleeding, infection, and primary graft failure. Long‑term, rejection episodes and side‑effects from immunosuppressants-like kidney damage or post‑transplant lymphoproliferative disorder-are the main concerns.
Can a patient live with both a transplant and a VAD?
Yes, some patients receive a VAD as a bridge to transplant. The device supports circulation while they wait for a donor heart, then is removed during the transplant surgery.
How does immunosuppression affect daily life?
Patients must take meds exactly as prescribed, avoid certain foods (like grapefruit), and get regular blood tests. The regimen does increase infection risk, so flu shots and hygiene are crucial.
Is a heart transplant curative for left ventricular dysfunction?
In most cases, replacing the failing heart restores normal left‑ventricular function, effectively curing the mechanical problem. However, underlying diseases (like amyloidosis) can still affect other organs.




Mahesh Upadhyay
Heart transplants save lives, but the waiting list feels like a cruel joke.
Rajesh Myadam
I get that frustration; the evaluation process is grueling, yet it weeds out those who might not survive the surgery.
Patients who make it past the listing often report a dramatic boost in daily activities.
It’s worth the paperwork marathon.
Kate McKay
Great rundown! The step‑by‑step layout really demystifies what can feel like a black box.
When you break it down, patients see a clear path from diagnostics to rehab.
That transparency can reduce anxiety and improve adherence to post‑op meds.
Also, remembering that quality‑of‑life scores jump after transplant helps keep hope alive.
Keep the info coming!
Kirsten Youtsey
While the overview is adequate, it glosses over the geopolitical undercurrents influencing organ allocation.
One must consider the ethical commodification inherent in the current UNOS paradigm.
Deja Scott
The article captures the medical facts nicely.
However, it omits the cultural stigma some patients face when discussing organ donation.
Addressing those beliefs could improve donor rates.
Andrew Hernandez
True, cultural perception matters a lot.
Education campaigns can shift attitudes.
Demetri Huyler
Let’s be honest: America’s transplant success rates set the global benchmark.
Our surgeons are unrivaled, and the infrastructure outpaces most nations.
Any criticism of the system ignores the hard work of our medical elite.
Patriotism should fuel continued investment.
JessicaAnn Sutton
The data presented is accurate, yet the narrative lacks critical analysis of long‑term immunosuppression side effects.
A deeper dive into post‑transplant malignancy statistics would be valuable.
Israel Emory
Indeed, the omission is glaring; however, let’s not overlook that the survival benefit still outweighs the oncologic risk, especially when patients adhere to rigorous screening protocols;
more comprehensive longitudinal studies are essential, and the community should demand them;
only then can we claim true transparency.
barnabas jacob
Yo, those VAD infection stats are straight up terrifying.
jessie cole
Indeed, the infection rates can be daunting; however, many patients still opt for VADs as a bridge to transplant.
The technology has improved, and prophylactic antibiotics reduce risk.
Ultimately, the decision hinges on individual risk tolerance.
Stay hopeful.
Matthew Hall
Man, the wait times feel like an eternity, but the hype around artificial hearts is blowing up.
We’ll see if they can actually replace good old transplants.
Vijaypal Yadav
Artificial hearts are still limited by power source durability and biocompatibility concerns.
Current devices can operate for months, not years, without major complications.
Research into wireless energy transfer may soon change that landscape.
Ron Lanham
When discussing the merits of heart transplantation versus mechanical support, one must first acknowledge the ethical responsibility we bear toward the most vulnerable patients.
It is not merely a matter of statistical survival percentages, but a profound moral imperative to restore dignity to those whose lives have been eclipsed by severe cardiac insufficiency.
Transplantation, when performed under stringent criteria, offers a chance at a near‑normal existence, allowing individuals to return to work, care for families, and contribute to society.
Conversely, ventricular assist devices, while technologically impressive, consign patients to a life tethered to machinery, fraught with constant infection risks and device‑related failures.
The psychological burden of living with an external pump cannot be understated; many patients report feelings of alienation and loss of bodily integrity.
Moreover, the allocation of donor organs is governed by principles of justice, urgency, and compatibility, ensuring that those most in need receive priority.
This framework, however, is vulnerable to manipulation and must be safeguarded against any form of nepotism or commercial influence.
It is incumbent upon the medical community to maintain transparency in listing criteria, rejecting any attempts to prioritize patients based on socioeconomic status.
Equally important is the need for lifelong adherence to immunosuppressive regimens, which, while life‑saving, expose patients to heightened infection and malignancy risks.
Patients must be educated thoroughly about these risks, and follow‑up care must be accessible regardless of insurance coverage.
The financial burden of transplantation, including medication costs, rehabilitation, and monitoring, should be mitigated through public health initiatives and insurance reforms.
Neglecting these socioeconomic dimensions perpetuates health inequities that are antithetical to the very ethos of medicine.
In addition, ongoing research into tolerance‑inducing protocols holds promise for reducing reliance on lifelong immunosuppression, potentially alleviating many of these concerns.
Investment in organ preservation technologies, such as normothermic perfusion, can expand donor pools and reduce waiting‑list mortality.
Ultimately, a balanced approach that integrates cutting‑edge mechanical support as a bridge, while prioritizing transplantation for eligible candidates, represents the most humane and ethically sound strategy.
Natalie Morgan
Thanks for the comprehensive moral perspective.
It highlights why policy and compassion must go hand in hand.