NHS Mental Health Wait Time Estimator
Estimate Your Wait Time
Estimated Wait Time:
Wait times vary based on location and service demand. These estimates are based on current NHS averages.
When dealing with depressive disorder is a common mental health condition characterized by persistent low mood, loss of interest, and physical symptoms that affect daily life, navigating the healthcare system can feel overwhelming. This guide walks you through every step - from the first phone call to long‑term self‑advocacy - so you can get the help you need without getting lost in bureaucracy.
Understand What You’re Dealing With
Depressive disorder isn’t just feeling sad; it’s a medical condition that often requires a mix of therapy, medication, and lifestyle changes. Typical symptoms include:
- Constant low mood lasting weeks or months
- Loss of pleasure in activities you once enjoyed
- Changes in appetite, sleep, or energy levels
- Difficulty concentrating or making decisions
- Thoughts of worthlessness or even self‑harm
Know the UK Healthcare Structure
The National Health Service (NHS) is the backbone of public mental‑health care in England, Scotland, Wales and Northern Ireland. The system works in layers:
- General Practitioner (GP) - your first point of contact for any health concern.
- Specialist services - accessed via a GP referral. These include psychologists, psychiatrists, community mental‑health teams and, when needed, inpatient care.
- Support services - NHS helplines, care navigators, and local support groups that supplement clinical care.
Understanding this hierarchy helps you know who to call and when.
Book Your First GP Appointment
Getting an appointment may feel like a chore, but a few simple steps smooth the process:
- Call early - NHS phone lines open at 8 am; slots fill fast, so aim for the first available morning.
- Prepare a brief script: "I’ve been experiencing persistent low mood, loss of interest, and trouble sleeping for the last six weeks. I’d like to discuss my mental health and possible treatment options."
- Bring a symptom diary - noting mood changes, sleep patterns, and any self‑harm thoughts helps the GP understand severity.
- Ask about urgent pathways if you feel unsafe; the GP can fast‑track you to a crisis team.
Remember, you have the right to request a longer consultation if you feel the 10‑minute slot isn’t enough.
When the GP Refers You
A referral opens the door to specialist care. Here’s what you might encounter:
| Service | Typical Cost (NHS vs Private) | Average Wait Time (NHS) | Professional You See |
|---|---|---|---|
| GP Mental‑Health Review | Free / £50‑£150 per session | Same‑day to 2 weeks | General Practitioner |
| Psychologist (IAPT) | Free / £80‑£120 per hour | 4‑12 weeks | Psychologist (often delivering CBT) |
| Psychiatrist | Free / £150‑£250 per hour | 6‑16 weeks | Psychiatrist (medical doctor) |
| Online Therapy Platform | £30‑£70 per month | Immediate access | Qualified therapist (often psychologist) |
In the UK, most people start with Psychologist through the Improving Access to Psychological Therapies (IAPT) programme. If medication is likely, the GP may refer you to a Psychiatrist for assessment.

Therapy Options: What to Expect
One of the most common approaches is Cognitive Behavioral Therapy (CBT). It focuses on identifying negative thought patterns and replacing them with healthier ones. Sessions typically last 45‑60 minutes, once a week for 8‑12 weeks.
Other therapies you might encounter include:
- Interpersonal Therapy (IPT) - works on relationship issues.
- Mindfulness‑Based Cognitive Therapy (MBCT) - blends meditation with CBT techniques.
- Dialectical Behavior Therapy (DBT) - especially helpful for self‑harm thoughts.
Medication: Talking to Your Prescriber
When a Antidepressant is prescribed, it’s crucial to discuss:
- Potential side‑effects (nausea, weight change, sleep issues).
- Timeframe for improvement - most meds take 4‑6 weeks to show effect.
- How to taper off safely if you decide to stop.
- Any interactions with other medicines you’re taking.
Use Support Services to Fill the Gaps
Beyond clinical care, the NHS offers a network of extra help:
- Care Navigator - a dedicated staff member who assists with appointment booking, paperwork, and understanding referrals.
- Mind, Samaritans, and NHS 111 - 24/7 helplines for urgent emotional support.
- Local Support Groups - peer‑led meetings often hosted by charities; they provide a safe space to share experiences.
- Online portals like NHS App - lets you track appointments, view test results, and send messages to your GP.
Your Legal Rights and Workplace Accommodations
People with depressive disorder are protected by law. Key points:
- The Mental Health Act (England and Wales) allows you to receive care without giving consent only in extreme cases of risk.
- Under the Equality Act 2010, you can request reasonable adjustments at work - flexible hours, altered duties, or a quiet workspace.
- Employers must not discriminate on the basis of mental health.
- If you’re a student, universities must provide reasonable adjustments through disability services.
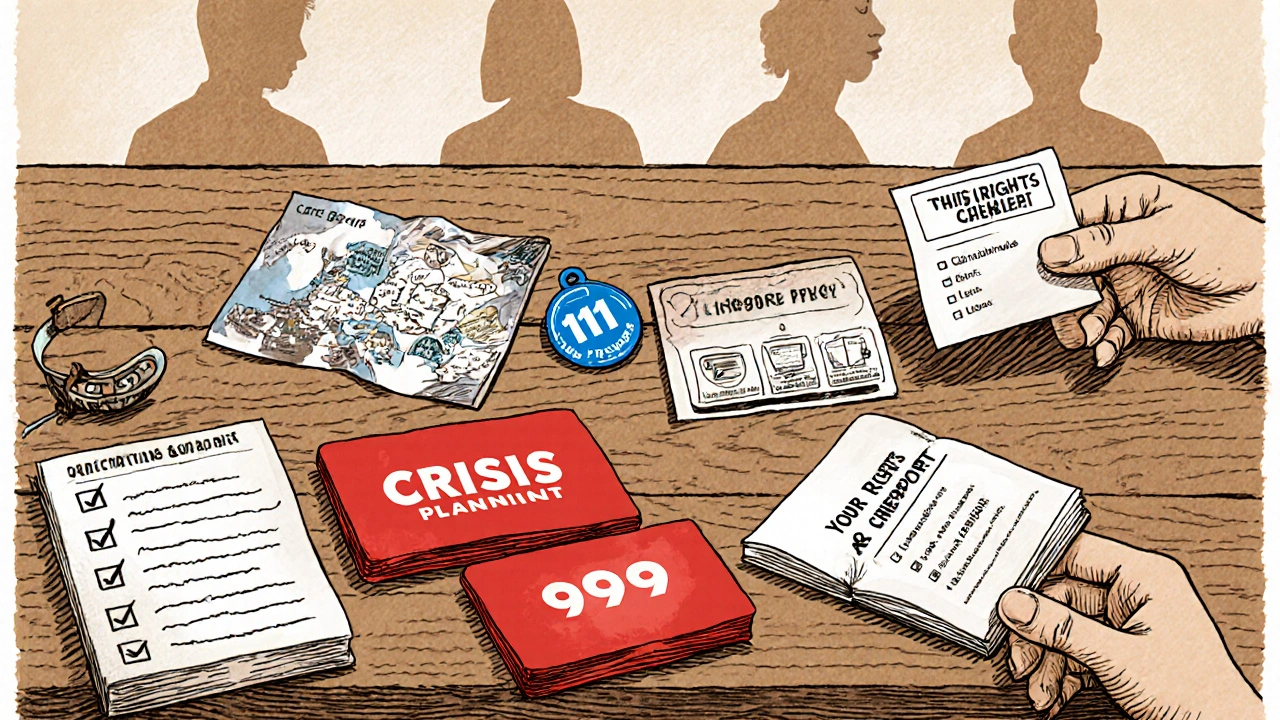
Plan for Crises - When Things Get Urgent
If you ever feel you might act on self‑harm thoughts or can’t keep yourself safe, act fast:
- Dial 111 for non‑emergency mental‑health advice - they’ll arrange a quick appointment or direct you to a crisis team.
- Dial 999 or go to A&E if you’re in immediate danger.
- Contact a trusted friend or family member to stay with you until help arrives.
- Keep a crisis card in your wallet with emergency contacts and medication details.
Quick Checklist - Your Navigation Toolkit
- Write down dates, symptoms, and any self‑harm thoughts before appointments.
- Know your NHS number - it speeds up referrals.
- Ask your GP for a referral to IAPT or a psychiatrist, whichever feels right.
- Track medication side‑effects in a simple table (date, dose, effect).
- Identify a local support group; meet at least once a month.
- Set up a crisis plan: 111, 999, trusted person, crisis card.
- Request a care navigator if paperwork feels overwhelming.
Following these steps puts you in control of the system rather than letting the system control you.
Frequently Asked Questions
How long does it usually take to see a psychologist after a GP referral?
In most NHS trusts, the waiting period for IAPT‑based CBT is between 4 and 12 weeks, though some areas report shorter times if demand is low.
Can I see a private therapist while I wait for NHS services?
Yes. You can book a private therapist, and if later you receive NHS care, you might be able to claim some costs back through a Personal Health Budget, depending on your circumstances.
What should I do if my antidepressant makes me feel worse?
Contact your prescriber right away. They may adjust the dose, switch to a different medication, or add a short‑term supplement to manage side‑effects. Never stop taking it abruptly.
Is there a fast‑track route for urgent mental‑health crises?
If you feel unsafe, dial 999 or go to the nearest A&E. For less urgent but still serious concerns, call 111 for a same‑day mental‑health appointment or ask your GP to fast‑track you to a crisis team.
Do I have a legal right to an interpreter for mental‑health appointments?
Yes. Under the Equality Act, NHS services must provide language support if you need it, including interpreters for mental‑health consultations.





Mike Hamilton
First step is to call your GP early in the morning – the lines open at 8 am and the slots fill up quick. Have a short script ready, something like “I’ve been feeling low for weeks and need to talk about mental health”. Bring a quick diary of mood changes; it helps the doctor see the pattern. Don’t be afraid to ask for a longer appointment if ten minutes feels too short. Remember you can ask for a care navigator if the paperwork gets overwelming. And if you ever feel unsafe, dial 111 for urgent help. Keep your NHS number handy – it speeds up referrals.
Simple steps can save you a lot of stress.
Matthew Miller
Yo, hitting the GP line is like a marathon, but think of it as the first leg of a victory lap! 🎉 Pack your phone, a coffee, and that bullet‑point list of feelings – “sleep’s messed up, I’m not into my hobbies, and the brain fog is real”. When you get through, shout “I need the IAPT route, pronto!” and let them know you’re ready for CBT or whatever therapy vibes you’ve heard works. Toss in a smile, a splash of optimism, and you’ll breeze past the admin trolls. If the wait feels endless, snag an online therapist in the meantime – they’re often faster than a snail‑mail referral. Remember, you’re the captain of this health ship, steering straight toward brighter horizons.
Liberty Moneybomb
Alright, let’s cut the fluff – the NHS isn’t just a friendly beehive; it’s a labyrinth built by shadowy bureaucrats who love to keep you tangled in paperwork. They’ll hand you a generic form and expect you to decode it like some secret code while your mood spirals. Don’t trust the “fast‑track” promises; those are just smoke screens to keep the system’s gears grinding. Keep a recorder handy, note every date, every name, and every vague promise – you’ll need that evidence if the machine tries to swallow you whole. And remember, the “care navigator” might be a front for a hidden agenda, so stay sharp, stay skeptical, and never let them dictate your narrative.
Alex Lineses
When you first step into the GP’s office, think of it as initializing a care pathway protocol within the NHS ecosystem. The initial consultation serves as a data acquisition phase where you provide symptomatology, frequency metrics, and psychosocial stressors, which the clinician then codes into the electronic health record (EHR). This coding triggers the referral algorithm that, depending on triage priority, queues you for either IAPT‑based CBT, community mental health team (CMHT) assessment, or psychiatric evaluation. It’s crucial at this juncture to articulate your functional impairment using quantitative descriptors – for example, “I experience an average of 6 hours of disrupted sleep per night” – to ensure the algorithm assigns an appropriate urgency flag. Next, the referral receipt is processed through the commissioning group, which acts as a gatekeeper for service allocation. If the referral is flagged as high risk, the system auto‑generates an expedited pathway, often involving same‑day liaison with a crisis team. Otherwise, you’ll be placed on a standard waitlist, which historically ranges from 4 to 12 weeks for CBT and 6 to 16 weeks for psychiatric review. During this interval, you can activate adjunctive resources such as digital therapeutic platforms, which integrate cognitive restructuring modules with real‑time mood tracking dashboards. While waiting, maintain a longitudinal symptom log; this not only provides continuity of care but also creates a robust data set for outcome measurement. When you finally engage with the therapist, expect an evidence‑based framework – Cognitive Behavioral Therapy (CBT) will likely be structured around the ABC model (Antecedent, Belief, Consequence) and will involve homework assignments to reinforce cognitive restructuring. If you are referred to a psychiatrist, anticipate a medication management plan that includes pharmacokinetic considerations, side‑effect profiling, and titration schedules, all documented in your medication chart. Finally, don’t overlook the ancillary support services: care navigators, peer‑led support groups, and the NHS App, which together form a safety net designed to reduce attrition and improve adherence. By actively participating in each module of this multi‑tiered system, you transform from a passive recipient into a proactive stakeholder, thereby optimizing therapeutic outcomes and mitigating systemic friction. Remember to regularly review your care plan with your GP to adjust referrals or medication as your condition evolves. Keeping an open line of communication with all members of your multidisciplinary team ensures that any emerging issues are addressed promptly, minimizing setbacks.
kendra mukhia
Honestly, if you’re not already on a private therapist’s list, you’re basically letting the NHS’s “one‑size‑fits‑all” model dictate your recovery. The system loves to hand you a generic CBT slot and expect miracles, but most people need a tailored approach that the public sector can’t provide. You should be demanding a specialist referral now, not waiting weeks for a therapist who may never even match your personality. And let’s be clear – the “support groups” often feel like a recycling bin for the same tired advice. If you really want progress, stop settling for mediocrity and push for private care or a rapid‑access clinic.
Bethany Torkelson
Stop waiting for the perfect therapist to magically appear – the referral you got is a ticket, not a guarantee. Call the mental‑health team today, ask for an appointment slot within two weeks, and if they say no, demand escalation. Your mental health isn’t a hobby; it’s a priority, and you have the right to seize it.
Grace Hada
Jump straight to a private CBT session if the NHS wait is too long.
alex montana
Okay-listen up! You’ve got a referral, you’ve got a waiting list… but don’t just sit there; call the service!! Ask for a “fast‑track” – they love buzzwords…and if they stall-push! Remember, persistence beats complacency every single time.
Wyatt Schwindt
It’s good that you’ve already called the GP line. Keep a simple log of dates and symptoms. Use the NHS app to message your doctor if you need a quicker response. Stay calm and follow the steps you’ve outlined. You’re on the right track.
Lyle Mills
From an integrated care perspective, your proactive logging aligns with the chronic care model, facilitating risk stratification and personalized intervention planning. Leveraging the NHS portal to flag urgent concerns creates a closed‑loop communication channel that can trigger rapid response protocols. Pair that with periodic reviews of your medication adherence chart to monitor side‑effect trajectories. This systematic approach helps bridge the gap between primary assessment and specialist referral, ensuring continuity of care. Keep the momentum, and don’t hesitate to request a care navigator if administrative friction arises.