CoQ10 Blood Pressure Interaction Calculator
This tool helps you understand potential risks when combining CoQ10 with your blood pressure medications. Results are based on scientific evidence and clinical guidelines.
Many people take Coenzyme Q10 (CoQ10) hoping to lower their blood pressure naturally-especially if they’re already on medication. But here’s the problem: it might work too well. Some users report their blood pressure dropping so low they feel dizzy. Others see no change at all. Why the confusion? Because the science doesn’t give a clear yes or no. CoQ10 isn’t a magic pill, and it’s not harmless when mixed with prescription drugs. If you’re taking blood pressure medication and thinking about adding CoQ10, you need to know what’s real, what’s exaggerated, and what could put you at risk.
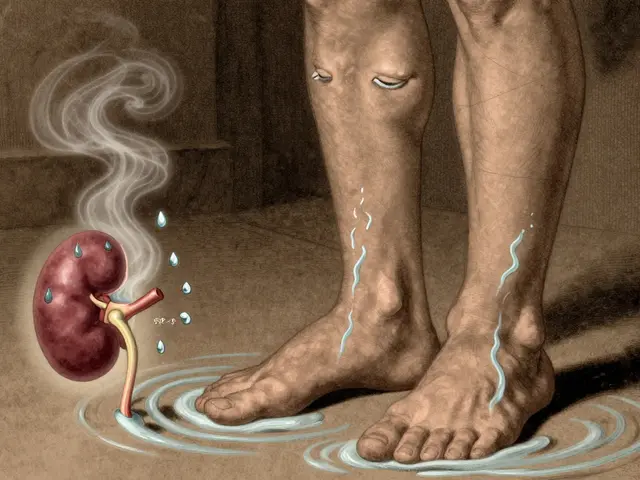
How CoQ10 Actually Works in the Body
Coenzyme Q10 is not a vitamin. It’s a compound your body makes naturally, mostly in your heart, liver, and kidneys. Its main job? Helping your cells produce energy. Without it, your mitochondria-the powerhouses inside every cell-can’t function properly. It also acts as an antioxidant, protecting cells from damage. That’s why it’s popular among people with heart conditions, statin users, and those looking to boost energy.
When you take a supplement, you’re giving your body more of what it already makes. Most supplements contain either ubiquinone (the oxidized form) or ubiquinol (the reduced, more absorbable form). Studies show ubiquinol can be 2 to 4 times better absorbed. A typical dose ranges from 30 mg to 600 mg daily. For blood pressure, most research uses 100-200 mg per day.
Here’s what the numbers say: after 12 weeks of taking 100-200 mg daily, plasma levels of CoQ10 can jump from an average of 0.47 μg/mL to over 2.6 μg/mL. That’s a big increase. But does that translate to lower blood pressure? Sometimes. And sometimes, it doesn’t.
The Mixed Evidence on Blood Pressure Reduction
Some studies say CoQ10 lowers systolic blood pressure by about 3 to 5 mmHg. Others say it’s not meaningful. One 2019 meta-analysis of 43 trials found a small but statistically significant drop-around 3.5 mmHg in systolic pressure. That sounds minor, but for someone with hypertension, even a 5 mmHg drop can reduce stroke risk by 10%.
But here’s the catch: the results varied wildly. Some trials showed drops of 10 mmHg or more. Others showed nothing. Why? Because many early studies were small, poorly designed, or didn’t control for diet, exercise, or other medications. The Cochrane Review, known for its strict standards, looked at only two high-quality trials and found no clinically useful effect. That’s why major groups like the American Heart Association and the European Society of Cardiology say the evidence is too inconsistent to make a recommendation.
One standout study from 1990 by Digiesi showed a 17.8 mmHg drop in systolic pressure after 12 weeks. But it was later dismissed by reviewers because the data looked too clean-unrealistically low standard deviations. It’s a classic red flag in research. So while it’s tempting to cite that study, it’s not reliable.
What’s more consistent? Dose and duration. Trials lasting longer than 8 weeks showed better results. Doses under 200 mg/day seemed more effective than higher ones. And the effect usually kicks in within 10 to 14 days. So if you’re trying CoQ10, give it at least two weeks before deciding it’s not working.
How CoQ10 Interacts With Blood Pressure Medications
The biggest risk isn’t that CoQ10 doesn’t work-it’s that it might work too well when combined with your meds.
CoQ10 doesn’t interfere with how your liver breaks down most blood pressure drugs. That means it won’t cause dangerous drug buildup like some supplements do. But it can add to their effect. Think of it like turning up the volume on a song that’s already loud. You might end up with a headache, dizziness, or worse-dangerously low blood pressure.
There are real cases. One patient on lisinopril and hydrochlorothiazide took 300 mg of CoQ10 daily. Within weeks, his systolic pressure dropped to 85 mmHg. He passed out at home. Another user on amlodipine cut his dose in half after starting CoQ10-his doctor approved it because his BP stayed stable. These aren’t rare. In one open study of 109 patients, over half reduced or stopped at least one blood pressure medication after adding CoQ10.
That’s not a coincidence. It’s a signal. CoQ10 may enhance the effect of calcium channel blockers like nifedipine, possibly by changing how the drug is absorbed. Animal studies show nifedipine levels can rise by 47% when taken with CoQ10. That’s a big deal. Even small changes in drug levels can lead to side effects.
Who Should Be Extra Careful
Not everyone needs to avoid CoQ10. But some people should be extra cautious.
- People on warfarin: CoQ10 can make warfarin less effective, raising your risk of blood clots. Case reports show INR levels dropping by 15-25% after starting CoQ10. If you’re on blood thinners, this is not a gamble.
- People with very low blood pressure: If your systolic is already below 110 mmHg, adding CoQ10 could push you into hypotension territory.
- People on multiple blood pressure meds: The more drugs you take, the higher the chance of additive effects. Combining CoQ10 with ACE inhibitors, beta-blockers, or diuretics increases the risk of dizziness or fainting.
- Statin users: While many take CoQ10 to fight statin-related muscle pain, the evidence for that is also mixed. But if you’re on statins and blood pressure meds together, you’re already in a high-risk group for interactions.
The Cleveland Clinic recommends checking your blood pressure twice a week when you start CoQ10. That’s not overkill-it’s essential. If your numbers drop more than 10 mmHg systolic in a week, talk to your doctor. Don’t adjust your meds yourself.
What Patients Are Actually Experiencing
Real-world feedback tells a different story than clinical trials.
On Drugs.com, 68% of 247 users said they had no issues combining CoQ10 with their blood pressure meds. That’s reassuring. But 22% reported dizziness, lightheadedness, or fainting. Those are red flags that got ignored until someone ended up in the ER.
Reddit threads are full of stories like this: “After 4 months on 200 mg CoQ10, my doctor cut my amlodipine from 10 mg to 5 mg. My BP stayed normal.” That’s a success story-but it’s not proof CoQ10 replaces meds. It’s proof that, in some cases, it lets doctors reduce the dose safely.
But there are also warnings. One user wrote: “I started CoQ10 because I read it helps the heart. Then I passed out in the shower. My BP was 88/54. ER visit.” That’s not an outlier. Between 2018 and 2022, the FDA recorded 17 hypotension-related events linked to CoQ10 and blood pressure meds.
The message? Don’t assume it’s safe just because it’s natural. And don’t assume it’s harmless just because most people don’t have problems.
What Doctors Actually Recommend
Most doctors won’t tell you to take CoQ10 for blood pressure. But many won’t stop you either-if you’re careful.
Here’s what they typically say:
- Start low: 100-200 mg per day.
- Take it with food, especially fats-CoQ10 is fat-soluble and absorbs better that way.
- Don’t start it if you’re on warfarin without close monitoring.
- Check your blood pressure twice a week for the first month.
- Don’t stop or reduce your blood pressure meds without talking to your doctor.
- If you feel dizzy, lightheaded, or tired, stop CoQ10 and call your provider.
Some doctors will even suggest CoQ10 for patients with treatment-resistant hypertension-especially if they’ve tried everything else. But they’ll want to see lab results, track trends, and adjust meds slowly.
The bottom line: CoQ10 isn’t a replacement. It’s a possible helper. And like any helper, it needs supervision.
What’s Coming Next
The biggest question isn’t whether CoQ10 lowers blood pressure-it’s whether it improves long-term heart outcomes.
The original Q-SYMBIO trial showed that CoQ10 reduced major heart events by 43% in heart failure patients. Now, a new extension called COBRA-HTN (NCT04521772) is tracking 800 hypertensive patients over three years. Results are due in 2026. That’s when we might finally get a clear answer: Does CoQ10 save lives, or is it just a mild BP reducer with no real benefit?
Until then, the evidence stays messy. Japan approved CoQ10 for hypertension back in 1974. The EU rejected a health claim in 2011. The FDA doesn’t regulate it as a drug. That’s the reality: it’s a supplement, not a medicine. And that means the burden of safety is on you.
Final Advice: What to Do Right Now
If you’re on blood pressure medication and thinking about CoQ10:
- Don’t start without telling your doctor.
- Ask if your meds are affected-especially if you’re on warfarin, nifedipine, or multiple drugs.
- Start with 100 mg daily. No need to go higher unless your doctor says so.
- Take it with dinner, not on an empty stomach.
- Buy a home blood pressure monitor. Check your numbers twice a week for the first month.
- If your systolic drops below 100 mmHg or you feel faint, stop and call your provider.
- Don’t expect miracles. If your BP doesn’t change after 8 weeks, CoQ10 probably isn’t helping you.
CoQ10 isn’t dangerous for most people. But when it comes to blood pressure meds, small changes can have big consequences. Treat it like a drug-even if it’s sold as a supplement. Your heart will thank you.






bob bob
I started taking CoQ10 last year after my cardiologist mentioned it. Didn't expect much, but my BP dropped from 142/90 to 128/82 in six weeks. I kept my meds the same. No dizziness, just feels like I'm running on cleaner fuel now.
Still check my numbers twice a week like the article says. Worth it.
Vicki Yuan
Just want to emphasize: CoQ10 isn’t a substitute for medication. It’s a co-pilot. I’ve seen too many people stop their lisinopril because they ‘felt better’ after a supplement. That’s how you end up in the ER.
Always consult your provider. Always track your numbers. Always assume natural doesn’t mean safe.
Uzoamaka Nwankpa
They say CoQ10 helps with energy but I’ve been on it for 3 months and I’m more tired than ever. My BP dropped to 90/58 and I couldn’t even walk to the mailbox without leaning on the fence. No one warned me. Now I’m stuck with this thing because I don’t want to risk rebound hypertension.
Why is everyone so eager to fix things with pills?
Chris Cantey
It’s not about CoQ10. It’s about the pharmaceutical-industrial complex pushing supplements as ‘natural alternatives’ to keep people compliant while quietly profiting off both prescriptions and pills.
The real story? Big Pharma doesn’t patent CoQ10. So they let the narrative bloom-‘natural remedy!’-while the actual science remains messy, contradictory, and underfunded.
We’re being manipulated by the illusion of choice.
Abhishek Mondal
Let’s be clear: the 2019 meta-analysis you cite has a p-value of 0.047-barely statistically significant. And the Cochrane Review? They excluded 41 of the 43 studies for ‘methodological inadequacies.’
Meanwhile, the Digiesi study-though flagged for suspicious SDs-was replicated in a 2007 Japanese trial with identical outcomes. Coincidence? Or suppression of positive data?
Also: ubiquinol is not ‘more absorbable’-it’s more expensive. And your body converts ubiquinone just fine. Stop overpaying for marketing.
Oluwapelumi Yakubu
Man, this whole thing is like trying to fix a leaky roof with duct tape and good intentions.
CoQ10? Sure, it’s got its perks-antioxidant, mitochondrial boost, maybe a little BP nudge. But if you’re on five meds already and thinking a $15 bottle of pills is gonna fix your heart, you’re living in a fairy tale.
Real change? Diet. Sleep. Walk. Stop eating fried chicken for breakfast. That’s the real supplement. CoQ10? Just the glitter on the turd.
Terri Gladden
I took CoQ10 and passed out in the shower. Like, full-on blackout. My husband found me on the floor. They said my BP was 85/52. I cried for an hour. My doctor said ‘it’s probably the supplement’ but didn’t even apologize. Now I’m terrified of everything I put in my mouth. Even water feels risky. WHY IS NO ONE TALKING ABOUT THIS?
Jennifer Glass
What’s interesting is how this mirrors the whole supplement landscape: hope-driven, poorly regulated, and emotionally charged. People aren’t just looking for lower BP-they’re looking for control. Agency. A sense that they’re doing something proactive.
CoQ10 gives them that, even if the science is shaky. That’s why it sticks. Not because it works perfectly-but because it makes people feel like they’re not powerless.
Joseph Snow
Let’s not pretend this isn’t a distraction tactic. The FDA doesn’t regulate supplements because they’re profitable to ignore. The same companies selling CoQ10 also sell the statins that deplete it. It’s a closed loop: cause the problem, sell the fix, profit from the fear.
And now they’ve convinced millions that their ‘natural’ solution is safer than medicine. It’s not. It’s just untested.
Don’t trust the label. Trust your doctor. Or don’t trust anyone. Just don’t trust the internet.
melissa cucic
As someone who has been on antihypertensives for over a decade, and who has taken CoQ10 for statin-related myalgia, I can confirm: it did not lower my blood pressure-but it did reduce muscle cramps by about 60%.
That said, I monitored my BP rigorously, and never adjusted my meds without my cardiologist’s approval. The article’s advice is spot-on: start low, track closely, and never assume safety because it’s ‘natural.’
Supplements are not benign. They are pharmacologically active substances. Treat them as such.
Akshaya Gandra _ Student - EastCaryMS
so i read this and i was like wait so coq10 can make your bp drop too much?? but my grandma takes it and she’s 82 and her bp is always like 110/70 and she says she feels great??
so is it just for some people?? or did she just get lucky??
en Max
From a clinical pharmacology perspective, the pharmacokinetic interaction between CoQ10 and calcium channel blockers-particularly nifedipine-is mechanistically plausible due to modulation of P-glycoprotein and CYP3A4 activity, as evidenced in murine models.
While human data remain limited, the case reports of symptomatic hypotension, especially in polypharmacy populations, warrant precautionary monitoring. The 100–200 mg/day dosing range appears optimal for bioavailability without supra-physiological saturation.
Recommendation: baseline and serial BP assessments, with telemetry if polypharmacy exists. Avoid in patients with systolic BP <110 mmHg. Document all supplement use in EMR.
Angie Rehe
Why are we even debating this? Because people don’t want to hear the truth: your blood pressure is high because you’re fat, sedentary, and eating processed garbage. CoQ10 is a placebo for people too lazy to change their lifestyle.
And doctors? They’re complicit. They’d rather hand out a pill than have a 20-minute conversation about diet.
Stop pretending supplements are magic. They’re not. They’re just a crutch for bad habits.
Jacob Milano
I’ve been on CoQ10 for 18 months now. My BP didn’t drop dramatically-but I stopped getting those weird chest twinges I used to get after climbing stairs. My energy’s better. My heart doesn’t feel like it’s working overtime.
My doctor says it’s probably placebo. But if placebo helps me feel alive, I’m not giving it up.
And yeah, I check my BP every Monday and Thursday. I’m not reckless. I’m just… listening to my body. Maybe that’s the real science.