Many older adults take medications every day to manage conditions like allergies, overactive bladder, depression, or insomnia. But what if some of those everyday pills are quietly harming their brain? That’s the reality of anticholinergic burden-a hidden risk built into common prescriptions and even over-the-counter drugs. It’s not a disease. It’s not a rare side effect. It’s the accumulated damage from blocking a key brain chemical called acetylcholine, and it’s linked to faster memory loss, confusion, and higher dementia risk in people over 65.
What Exactly Is Anticholinergic Burden?
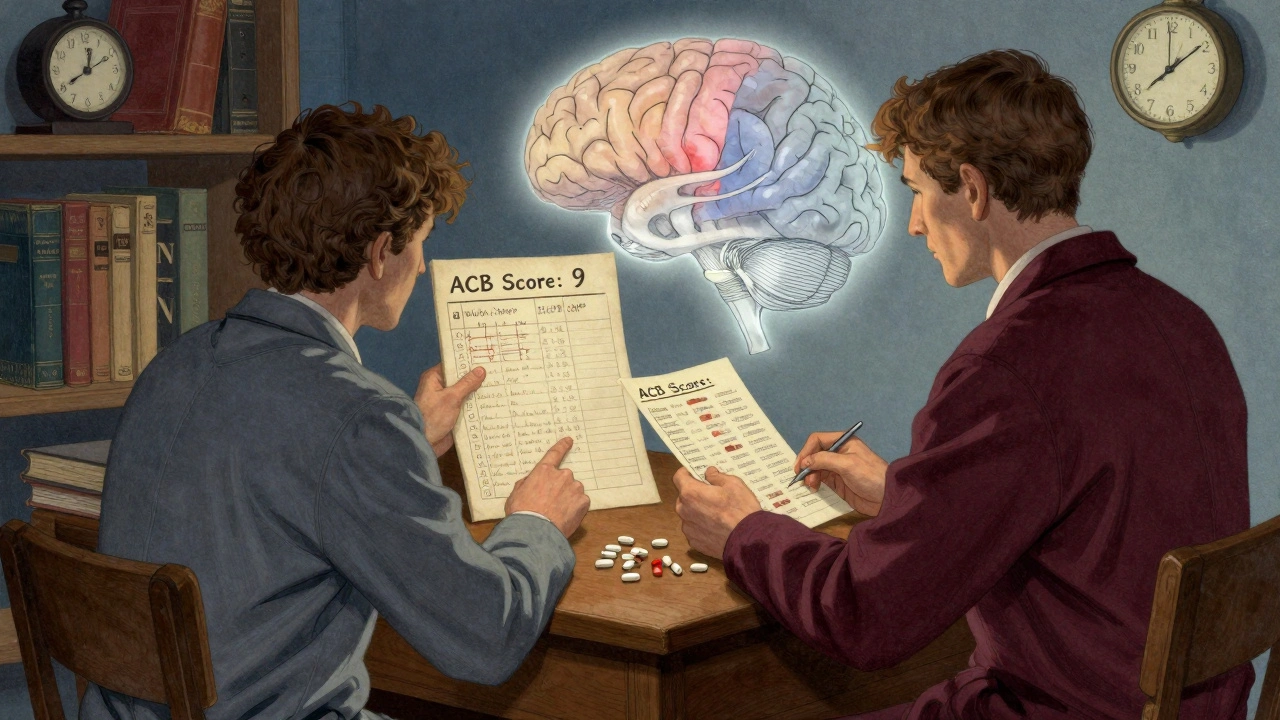
Anticholinergic burden (ACB) is the total effect of all the medications you’re taking that block acetylcholine. This chemical is essential for memory, attention, and clear thinking. When it’s blocked, your brain struggles to send signals properly. Think of it like turning down the volume on your brain’s communication system. The more drugs you take that do this, the louder the static gets. There are three main scales doctors use to measure this burden: the Anticholinergic Cognitive Burden (ACB) scale, the Anticholinergic Risk Scale (ARS), and the Drug Burden Index (DBI). The ACB scale is the most widely used today. It ranks drugs from Level 1 (mild effect) to Level 3 (strong effect). A single Level 3 drug, like amitriptyline or oxybutynin, can add 3 points to your total burden. If you’re taking three Level 2 drugs, that’s another 6 points. Suddenly, you’re at a score of 9-far above the threshold where cognitive risks start rising.Which Medications Carry the Highest Risk?
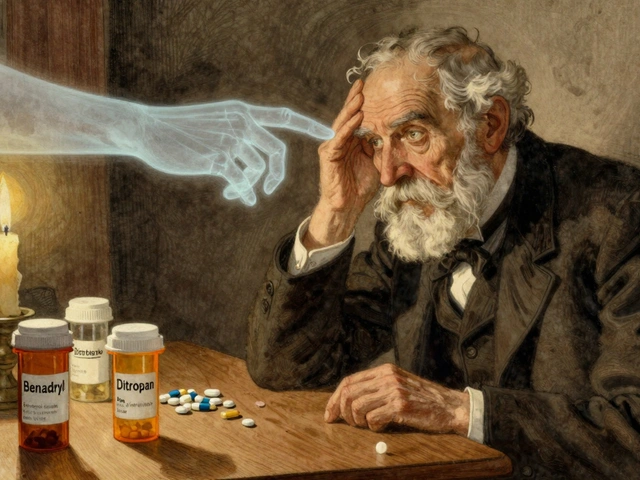
Not all anticholinergics are created equal. Some are obvious. Others sneak in under the radar. Here are the top offenders:- First-generation antihistamines: Diphenhydramine (Benadryl), chlorpheniramine. These are in many sleep aids and cold medicines. Even one pill a night adds up.
- Overactive bladder drugs: Oxybutynin (Ditropan), tolterodine, solifenacin. These are among the most commonly prescribed anticholinergics in seniors.
- Tricyclic antidepressants: Amitriptyline, nortriptyline. Still used for depression and nerve pain, despite better alternatives.
- Some Parkinson’s drugs: Trihexyphenidyl, benztropine.
- Anti-nausea meds: Promethazine, dimenhydrinate.
How Much Damage Can These Drugs Really Do?
The numbers are startling. A 2015 study in JAMA Internal Medicine found that taking anticholinergic drugs for three years or more increased dementia risk by 54% compared to short-term use. That’s not a small bump-it’s a major jump. Brain scans show real physical changes. A 2016 JAMA Neurology study found that people on medium-to-high ACB medications had 4% less glucose metabolism in the temporal lobe-the same area that shuts down early in Alzheimer’s. Another study tracking 451 older adults over three years found they lost brain volume 0.24% faster per year than those not on these drugs. That’s like losing a teaspoon of brain tissue every few months, just from medication. Cognitive tests show clear patterns. Each extra point on the ACB scale is linked to:- 0.15-point greater annual decline on tests of word fluency (executive function)
- 0.08-point greater decline on memory recall tests
- Minimal impact on processing speed

Real People, Real Results
Behind the data are real stories. On AgingCare.com, a caregiver wrote: “My mom’s confusion cleared within two weeks after stopping oxybutynin. Her doctor didn’t even know it was causing this.” That’s not an outlier. The FDA recorded over 1,200 cognitive-related adverse events in seniors between 2018 and 2022-confusion, memory loss, delirium-all tied to these drugs. A 2021 survey of 312 older adults found that 63% were never told about the cognitive risks when prescribed these medications. Forty-one percent said they’d have chosen a different treatment if they’d known. That’s not just a gap in communication-it’s a failure in patient safety.Can the Damage Be Reversed?
Yes. And that’s the most important part. The DICE trial in 2019 followed 286 older adults who gradually stopped or switched anticholinergic medications. After 12 weeks, their Mini-Mental State Exam (MMSE) scores improved by 0.82 points on average. That’s not a cure, but it’s meaningful-enough to help someone remember names again, manage their medications, or drive safely. Reversal doesn’t happen overnight. It takes 4 to 8 weeks for the brain to start recovering. But the improvement is real. People report clearer thinking, less brain fog, and better sleep-without the grogginess that often comes with these drugs.What Should You Do?
If you or a loved one is over 65 and taking any of these medications, here’s what to do:- Make a full list: Write down every prescription, OTC pill, and supplement. Include what you take and how often.
- Check the ACB score: Use the free ACB Calculator app from the American Geriatrics Society. It’s quick, free, and updated to version 3.0.
- Ask your doctor: “Is this drug necessary? Is there a non-anticholinergic alternative?” Don’t be afraid to push. For example:
- Instead of diphenhydramine for sleep: try melatonin or cognitive behavioral therapy for insomnia.
- Instead of oxybutynin for bladder issues: consider pelvic floor therapy or mirabegron (a non-anticholinergic option).
- Instead of amitriptyline for pain or depression: try SSRIs like sertraline or duloxetine.
- Don’t quit cold turkey: Some drugs need to be tapered slowly to avoid withdrawal or worsening symptoms.
- Recheck every 6 months: Medication needs change. What was safe last year might not be this year.
Why Is This Still Happening?
You’d think with all this evidence, doctors would stop prescribing these drugs. But here’s the problem: it’s complicated. A 2022 study found only 38.7% of nursing home residents with high ACB scores had their meds reviewed within three months of being flagged. Primary care doctors say they need 23 minutes per patient to do a proper review-but most appointments are 15 minutes or less. Also, some doctors still believe these drugs are “harmless” or “the only option.” But that’s outdated. In 2023, the American Geriatrics Society’s Beers Criteria explicitly says to avoid strong anticholinergics in older adults. The European Medicines Agency restricted dimenhydrinate in dementia patients. The FDA now requires updated warning labels. And pharmaceutical companies are responding. Johnson & Johnson pulled its long-acting oxybutynin in 2021. Pfizer pushed solifenacin, which has less brain penetration. But many older versions are still widely prescribed.The Bigger Picture
The Lancet Healthy Longevity Commission now lists anticholinergic burden as one of the top 10 modifiable risk factors for dementia. That means if we fix this, we could prevent 10-15% of dementia cases in older adults. It’s not about fear. It’s about awareness. You don’t need to stop every medication. You just need to know which ones are doing more harm than good-and ask for better options. A 2024 analysis in JAMA Internal Medicine found that 78.4% of high-ACB prescriptions in Medicare patients were for conditions with equally effective, non-anticholinergic alternatives. That’s not a coincidence. It’s a missed opportunity.Final Thought
Your brain doesn’t get a do-over. Once memory declines, it’s hard to get back. But the good news? You have more control than you think. Many of the pills that fog your thinking aren’t necessary. They’re just old habits dressed up as medicine. Ask the questions. Check the list. Demand alternatives. Your future self will thank you.Can anticholinergic medications cause permanent brain damage?
There’s no clear evidence that anticholinergic drugs cause permanent structural damage in most cases. But long-term use can accelerate brain shrinkage and reduce brain activity in memory areas, which may increase dementia risk. The good news? Many cognitive effects are reversible. Studies show improvements in memory and thinking within weeks to months after stopping these drugs. The longer you take them, the longer recovery may take-but it’s still possible.
Are all antihistamines dangerous for seniors?
No. Only first-generation antihistamines like diphenhydramine (Benadryl) and chlorpheniramine have strong anticholinergic effects. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are much safer for older adults. They don’t cross the blood-brain barrier as easily, so they don’t affect thinking. Always check the active ingredient-not just the brand name.
Is it safe to stop anticholinergic meds on my own?
No. Stopping suddenly can cause withdrawal symptoms or make your original condition worse. For example, stopping an overactive bladder medication abruptly might lead to urinary retention. Always work with your doctor to create a tapering plan. Most safe reductions take 4 to 8 weeks, sometimes longer depending on the drug and your health.
What’s the difference between ACB score and Drug Burden Index?
The ACB scale focuses only on anticholinergic strength (Level 1-3) and counts how many drugs you’re taking. The Drug Burden Index (DBI) measures total anticholinergic and sedative load based on daily dose and potency. DBI is more precise for drugs like benzodiazepines or sleep aids that aren’t purely anticholinergic. ACB is simpler and more widely used in research. Both are useful, but ACB is the go-to for identifying dementia-linked risks.
Can I use the ACB Calculator if I’m not in the U.S.?
Yes. The ACB Calculator app from the American Geriatrics Society works globally. It’s based on drug mechanisms, not country-specific formularies. As long as you know the generic name of your medication, you can look it up. Many international pharmacies list anticholinergic ratings on their websites. If you’re unsure, ask your pharmacist to check the ACB level for each drug.
Why do doctors still prescribe these drugs if they’re risky?
Several reasons: time pressure, lack of awareness, or belief that the drug is the only option. Many doctors weren’t trained on anticholinergic burden. Others assume patients won’t tolerate alternatives. But evidence shows non-anticholinergic options work just as well-for bladder issues, depression, insomnia, and pain. The real barrier isn’t medical-it’s systemic. Better tools, more training, and patient advocacy are changing that.


Marvin Gordon
I had no idea Benadryl was this bad for the brain. My grandma took it every night for years. She started forgetting where she put her glasses, then her keys, then my name. We switched her to melatonin last year and her clarity came back like a switch flipped. No more midnight confusion.
Doctors act like it's harmless because it's OTC, but it's not. It's like giving someone a daily dose of brain fog and calling it a sleep aid.
Norene Fulwiler
My mom’s doctor prescribed her oxybutynin for ‘bladder issues’ and never mentioned the dementia risk. She started zoning out during conversations, forgetting appointments, even mistaking the TV for a window. We pulled the pill after reading this - and within three weeks, she was herself again. Why isn’t this common knowledge?
It’s not just about pills. It’s about who gets informed - and who gets left in the dark.
Ada Maklagina
I took amitriptyline for 8 years for nerve pain. Felt like my thoughts were underwater. Stopped cold turkey because I was tired of being a zombie. Brain fog lifted after 6 weeks. No regrets. Doctors don’t warn you because they’re not trained to care.
Harry Nguyen
Oh here we go. Another fear-mongering article from the geriatric witch hunt brigade. Next they’ll ban aspirin because it might ‘slow your thinking’ if you’re 70. Wake up. People aren’t idiots. If you’re old enough to need meds, you’re old enough to decide if you want brain fog or a decent night’s sleep.
And no, I’m not taking melatonin. I’m taking what works. Your ‘non-anticholinergic alternatives’ are just expensive placebos with more side effects.
James Moore
Consider, for a moment, the metaphysical implications of acetylcholine as a neurotransmitter - not merely a biochemical actor, but a metaphysical conduit of consciousness itself. When we pharmacologically suppress it, are we not, in essence, silencing the soul’s whisper? The modern medical-industrial complex, driven by profit and convenience, has turned the human brain into a disposable circuit board - replace the part, don’t question the system.
And yet, the irony: we treat dementia like an inevitability, while ignoring the very pills we prescribe that accelerate it. Is this not the ultimate tragedy of late-stage capitalism? We optimize for function, not for being.
Ask yourself: when your mind dims, is it the aging - or the pharmacy?
Kylee Gregory
I appreciate how thorough this is. It’s easy to panic about meds, but this doesn’t just scare - it empowers. The ACB calculator alone could save so many people from unnecessary decline.
I’ve seen friends stop meds cold turkey and crash. The tapering advice is crucial. And the fact that improvement is possible? That’s hope. Not magic. Just science. And it’s worth fighting for.
Lucy Kavanagh
Did you know the FDA and Big Pharma have been hiding this since the 80s? They knew anticholinergics cause dementia - but they didn’t want to scare seniors away from their profits. That’s why the warnings are buried in tiny print. And why your doctor hasn’t heard of it - because they’re paid to not know.
They’re also using these drugs to control nursing home residents. You think it’s for ‘bladder issues’? No. It’s to keep them docile. Look up the 2017 whistleblower report. It’s all connected.
Chris Brown
It’s irresponsible to suggest people stop their medications without professional oversight. These are not candy. You don’t just ‘quit’ antidepressants or bladder meds because some blog post scared you.
And who authorized this ACB calculator? A non-profit with no regulatory authority? That’s not medicine - that’s internet quackery dressed in clinical language. If your doctor hasn’t flagged your meds, they’re doing their job. You’re not smarter than your physician.
Stephanie Fiero
OMG this is so important!! I just found out my dad’s sleeping pill is diphenhydramine and he’s been on it for 5 years!! I’m gonna print this out and take it to his next appt. He’s 72 and has been so forgetful lately - I thought it was just aging. NOPE. It’s the meds.
Also why do doctors keep prescribing this stuff?? I’m so mad right now. My mom’s doctor said ‘it’s fine’ when I asked about it. I’m calling them tomorrow. This needs to change.
Someone please make a poster for pharmacies: ‘THIS PILLS MAKE YOU DUMB’.
Michael Dioso
They call it ‘burden’ like it’s a weight. It’s not. It’s a betrayal. We were told these were safe. We were told to trust the system. We were told the pills were helping. Turns out they were just quietly turning our brains to mush so we’d stop asking questions.
And now you want us to switch to ‘alternatives’? What’s next? A placebo with a higher price tag and a new FDA-approved acronym? We’re not patients. We’re test subjects with credit cards.
sean whitfield
The real problem? People still think doctors know what they’re doing. Newsflash: they’re just following scripts written by drug reps who got free dinners. You think they care about your brain? They care about your refill rate.
Carole Nkosi
As a woman of African descent who has watched my grandmother lose her mind to pills she didn’t understand, this resonates deeply. In many cultures, elders are given medicine without explanation. We call it ‘care.’ It’s often just neglect with a prescription pad.
But we are waking up. We are asking. We are refusing. And we are reclaiming our minds - one pill at a time.
Manish Shankar
It is with profound respect for the scientific rigor presented in this article that I acknowledge the gravity of the issue at hand. The accumulation of anticholinergic agents in elderly populations constitutes a significant public health concern, particularly in light of the robust longitudinal data cited from peer-reviewed journals such as JAMA.
I would respectfully suggest that further research be directed toward cross-cultural pharmacokinetic variations, as metabolic pathways may differ significantly among global populations, thereby influencing the true burden of these medications beyond Western clinical norms.
luke newton
So now I’m supposed to feel guilty because I took a Benadryl once a week for 10 years? You know what? My brain is fine. My memory is sharp. My kids are grown. I’m not some fragile old person you need to protect from my own choices.
And if you think I’m going to switch to melatonin because some blogger says so, you’ve got another thing coming. I’ve earned the right to sleep how I want.
Ali Bradshaw
I’ve been a GP for 28 years. I used to prescribe these drugs without a second thought. Then I saw a patient - 74, sharp as a tack - start forgetting her grandkids’ names after starting oxybutynin. We switched her to mirabegron. Three months later, she brought me cookies and said, ‘I remembered my husband’s birthday again.’
It’s not about fear. It’s about awareness. And sometimes, it’s about listening to the people you’re supposed to be helping.