Medication Reconciliation: What It Is and Why It Saves Lives
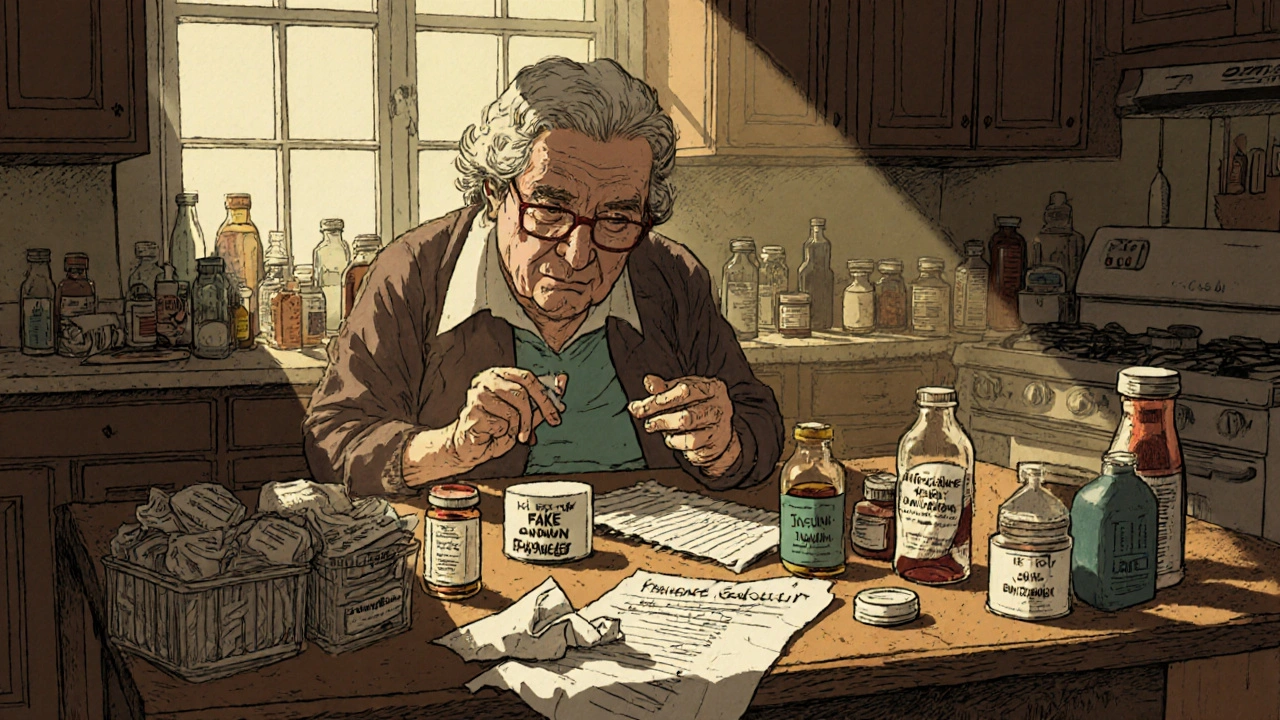
When you’re taking multiple drugs, medication reconciliation, the process of comparing a patient’s medication orders to all of the medications they’ve been taking. It’s not just paperwork—it’s a safety net that stops deadly mix-ups before they happen. Think of it like checking your bank statement against your receipts. If you’re on five pills, but your doctor only knows about three, something’s wrong. That gap is where accidents happen—overdoses, bad interactions, missed treatments. And it’s not rare. One in five hospital admissions for older adults is tied to medication errors, and half of those could’ve been caught with proper reconciliation.
Drug interactions, when two or more medications affect each other’s behavior in the body are a big part of the problem. Take someone on metformin for diabetes who also grabs goldenseal from the supplement aisle. That herb can block metformin’s effect, spiking blood sugar. Or someone on beta-blockers and calcium channel blockers—both for blood pressure—might get a dangerously slow heart rate if the wrong combo is used. Medication list, a real-time, updated record of every drug, dose, and reason for taking it is the tool that makes reconciliation work. It’s not a sticky note on the fridge. It’s a living document you carry to every doctor visit, ER trip, or pharmacy stop.
Pharmacists are often the ones who catch these errors, but they can’t do it alone. You have to bring the full picture. That means including vitamins, herbal stuff, over-the-counter painkillers, even eye drops. If you don’t mention it, they won’t know it’s there. And it’s not just about pills—some drugs like doxycycline make your skin burn in the sun. If your doctor doesn’t know you’re taking it, they might send you hiking without warning. Same with antibiotics that mess with birth control, or decongestants that lock up your bladder if you have an enlarged prostate. These aren’t edge cases. They’re everyday risks.
Medication reconciliation isn’t a one-time thing. It happens every time you switch providers, get discharged from the hospital, or fill a new prescription. That’s why pharmacy safety, the system of checks and communication that keeps medications accurate and safe depends on you being active in the process. Don’t assume your doctor remembers what you told them last month. Don’t let the pharmacy guess what’s new. Bring your list. Update it. Ask questions.
And if you’ve ever been confused about why your generic pill looks different than last time, or worried you’re taking too many pills, you’re already in the right place. The posts below cover real stories and real fixes—from how to spot counterfeit pharmacies to why generic drugs look different, how to test for true antibiotic allergies, and what to do when your meds stop working. This isn’t theory. It’s what keeps people alive. And you don’t need to be a doctor to make it work. You just need to know what to ask, what to track, and when to speak up.
Sharing your full medical history-including prescriptions, OTC drugs, and supplements-is essential to avoid dangerous medication errors. Learn how to create an accurate list and communicate it effectively to your healthcare team.
Medication errors harm millions each year-but most are preventable. Learn how hospitals and homes can stop wrong doses, fake drugs, and dangerous mix-ups with proven strategies that actually work.