SSLR vs. Antibiotic Allergy Calculator
Diagnose Your Child's Antibiotic Reaction
This tool helps determine if your child's symptoms are likely a serum sickness-like reaction (SSLR) or a true antibiotic allergy. SSLR is common and treatable, but misdiagnosis can lead to unnecessary antibiotic restrictions.
Results will appear here
When a child develops a rash, fever, and swollen joints a week after taking an antibiotic, it’s natural to panic. Many parents assume it’s a severe allergy-maybe even a life-threatening one. But what if it’s not an allergy at all? What if it’s something called a serum sickness-like reaction (SSLR)? This condition is far more common than most people realize, especially in young kids, and misdiagnosing it can lead to unnecessary restrictions on antibiotics for years-even decades.
What Exactly Is a Serum Sickness-Like Reaction?
SSLR isn’t true serum sickness. That’s an old condition from the 1900s, caused by immune reactions to animal-derived antiserums used to treat things like snake bites or rabies. Modern SSLR has nothing to do with animal proteins. Instead, it’s a delayed immune response triggered by certain antibiotics-most often cefaclor, but also amoxicillin and a few others. It shows up 1 to 21 days after taking the drug, usually around day 7 or 8. The classic signs? A rash that looks like hives, fever, and joint pain. The rash moves. One moment it’s on the arms, then it disappears and reappears on the legs or torso. It itches badly, but it doesn’t leave marks. Fever is usually mild-between 38°C and 39°C. Joints, especially knees, wrists, and ankles, feel stiff and sore. Some kids get swollen lymph nodes or feel tired. But here’s the key: no kidneys, lungs, or heart problems. No blood in the urine. No dangerous swelling of the throat or tongue. That’s what separates SSLR from true allergic reactions or systemic illness.Why It’s Not a True Allergy
True allergies involve IgE antibodies and can cause anaphylaxis within minutes. SSLR? It’s a different kind of immune response-likely driven by T-cells, not IgE. Blood tests show no immune complexes, no drop in complement levels, no signs of vasculitis. That’s why doctors used to confuse it with true serum sickness. But since the 1980s, research has shown it’s a separate condition. This matters because if a child is labeled as “allergic to penicillin” after an SSLR, they might be denied safe, effective antibiotics for the rest of their life. Instead, they get broader-spectrum drugs like vancomycin or azithromycin-drugs that are more expensive, more likely to cause side effects, and worse for gut health. Studies show that 42% of kids with SSLR are wrongly labeled as penicillin-allergic. That leads to 18% more cases of antibiotic-resistant infections down the line.Which Antibiotics Cause It?
Cefaclor is the biggest offender. It’s responsible for 65% to 80% of pediatric SSLR cases. That’s because some children have a genetic variation in their liver enzyme CYP2C9, which causes the body to build up a specific metabolite of cefaclor. This metabolite seems to trigger the immune response. Amoxicillin is next, especially in younger kids. Other cephalosporins can cause it too, but far less often. The good news? If your child had SSLR from cefaclor, they can almost always safely take other cephalosporins later. About 89% of kids tolerate them without issue. The same goes for penicillins-unless the reaction was directly to amoxicillin. You don’t need to avoid the whole class. Only the specific drug that caused the reaction.How Is It Diagnosed?
There’s no single blood test for SSLR. Diagnosis is based on timing, symptoms, and ruling out other causes. Doctors look for:- Rash appearing 7-10 days after starting the antibiotic
- Classic triad: urticarial rash, fever, joint pain
- No kidney involvement (normal urine test)
- No signs of infection like strep throat or mono

What Happens After the Reaction?
The first step is simple: stop the antibiotic. Most kids start feeling better within 24 to 48 hours. The rash fades over 3 to 7 days. Joint pain and fever go away too. In 92% of cases, the problem is completely gone within a week. For symptom relief:- Antihistamines like cetirizine help with itching. They’re safe for kids and don’t cause drowsiness.
- NSAIDs like ibuprofen reduce fever and joint pain.
- Corticosteroids (like prednisone) are only used if symptoms are severe-like when a child can’t walk or sleep because of the pain.
What About Future Antibiotics?
Don’t avoid all penicillins or cephalosporins. Only avoid the one that caused the reaction. If it was cefaclor, your child can likely take amoxicillin, cephalexin, or cefdinir without issue. If it was amoxicillin, avoid that one, but other cephalosporins are usually fine. A 2023 study from Cincinnati Children’s Hospital followed 120 kids with SSLR. They did oral challenges 12 months after the reaction. Only 8% had any reaction-and those were mild. The rest tolerated the drug without a problem. The bottom line: SSLR doesn’t mean your child is allergic to a whole class of antibiotics. It means they reacted to one specific molecule. That’s a big difference.Why Misdiagnosis Costs Money-and Health
Mislabeling SSLR as a penicillin allergy leads to real harm. Hospitals use broader antibiotics, which are more expensive and increase the risk of C. diff infections and antibiotic resistance. A 2022 study estimated that in the U.S. alone, this mistake costs $187 million a year. It also affects future care. Kids labeled “penicillin-allergic” are more likely to get IV antibiotics, longer hospital stays, and more side effects. They’re also less likely to get the right treatment for ear infections, sinus infections, or pneumonia. One parent on Reddit shared: “My daughter had SSLR after amoxicillin. The ER called it a penicillin allergy. Now she gets vancomycin for every infection. She’s had three C. diff infections already.”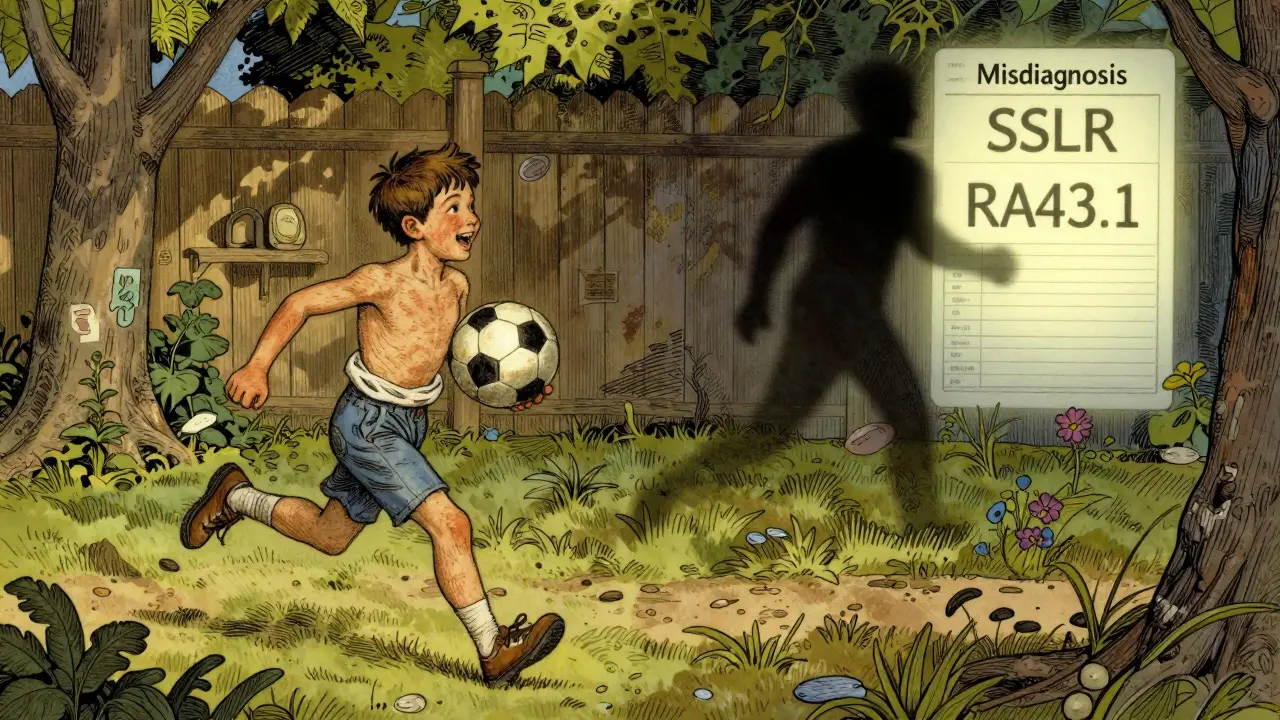
What’s Changing Now?
In 2024, the World Health Organization and major allergy societies officially recognized SSLR as its own diagnosis with its own ICD-11 code: RA43.1. That means doctors can now code it correctly in medical records instead of just writing “allergy.” New research is also helping. Scientists at the University of California are testing a urine test that can detect the specific metabolite linked to cefaclor-triggered SSLR. Early results show 94% accuracy. If it’s approved, it could make diagnosis as simple as a pee sample. Hospitals like Boston Children’s are testing AI tools that flag SSLR patterns in electronic health records. In trials, the system spotted SSLR with 88% sensitivity and 91% specificity. That means fewer kids get mislabeled.What Should Parents Do?
If your child develops a rash, fever, or joint pain after an antibiotic:- Stop the antibiotic and call your pediatrician.
- Don’t assume it’s an allergy. Ask: “Could this be a serum sickness-like reaction?”
- Request an allergist consult before labeling your child “allergic.”
- Keep a record: what drug, when it started, what symptoms appeared, how long they lasted.
- Ask about a future oral challenge-don’t let your child miss out on safe, effective antibiotics.
Final Thoughts
SSLR isn’t scary. It’s uncomfortable, yes. But it’s not life-threatening. And it’s not a life sentence to avoid penicillin. With the right diagnosis, kids can go back to getting the best, safest, cheapest antibiotics when they need them. The problem isn’t the reaction. It’s the misunderstanding. Too many doctors still think “rash + antibiotic = allergy.” But science says otherwise. And parents who ask the right questions can protect their kids from years of unnecessary risk.Is serum sickness-like reaction the same as a penicillin allergy?
No. A penicillin allergy is an IgE-mediated reaction that can cause anaphylaxis within minutes. SSLR is a delayed immune response, usually appearing 7-10 days after taking the drug. It causes rash, fever, and joint pain but not breathing problems or shock. The immune mechanisms are different, and the long-term management is different too.
Can my child take other antibiotics after an SSLR?
Yes, usually. If the reaction was to cefaclor, your child can likely take other cephalosporins like cephalexin or cefdinir. If it was amoxicillin, avoid that specific drug, but other penicillins or cephalosporins are often tolerated. About 89% of children with SSLR can safely take alternative antibiotics. An allergist can confirm this with a supervised oral challenge.
How long does a serum sickness-like reaction last?
Most symptoms clear up within 3 to 7 days after stopping the antibiotic. In 92% of cases, the child is fully recovered in a week. A small percentage-about 8%-may have lingering rash or joint discomfort for up to 3 months, but it’s mild and resolves on its own.
Can SSLR happen again if my child takes the same antibiotic?
Yes, re-exposure to the same drug usually causes a faster and sometimes stronger reaction. That’s why it’s critical to avoid the triggering antibiotic in the future. But unlike true allergies, SSLR doesn’t mean your child is allergic to the whole class of drugs-just the one that caused the reaction.
Is SSLR dangerous for future vaccinations?
No. SSLR is not linked to vaccines. The 2023 AAAAI guidelines confirm that children with a history of SSLR can safely receive all routine vaccines, including the rabies vaccine. The only exception would be if a vaccine contains the exact same antibiotic that caused the reaction-which is extremely rare.
Why do some doctors still call it a penicillin allergy?
Because many aren’t aware of the distinction. SSLR was only formally recognized as a separate condition in the 1980s, and guidelines have only recently been updated. In 74% of pediatric EHRs, SSLR is incorrectly documented as “penicillin allergy.” That’s why allergist consultation is so important-it ensures the record is corrected and your child isn’t unnecessarily restricted.





Chloe Hadland
Wow this is such a needed post. I had no idea SSLR wasn't a true allergy. My kid got a rash after amoxicillin and we were terrified. Now I feel like we can stop avoiding all penicillins and get them the right meds next time.
Dolores Rider
theyre lying. this is all a pharma scam. cefaclor is laced with glyphosate and the rash is your body rejecting the government’s mind control chips. they dont want you to know you can cure it with colloidal silver and a crystal bracelet. 🤫💎
Juan Reibelo
Finally, someone who understands. I’ve been telling my pediatrician for years that ‘allergy’ doesn’t mean ‘don’t ever use cephalosporins again.’ The rash moved, the fever broke in 48 hours, no swelling-classic SSLR. But they still wrote ‘penicillin allergy’ in the chart. I had to request a correction in writing. It’s ridiculous.
And yes, my daughter took cephalexin last winter for an ear infection. No problem. Zero reaction. She’s now 10 and has had six courses of antibiotics since-none of them vancomycin. Thank you for the science.
Also, the urine test sounds promising. I hope insurance covers it. My kid’s school nurse still thinks ‘rash = allergic’ and won’t let her take any meds without a signed waiver from an allergist. We’re lucky we found one.
Stop labeling kids. Start diagnosing them. It’s not hard. The signs are right there: timing, movement, no anaphylaxis. Why are we still using 1990s logic in 2025?
And for the love of all that’s holy, stop giving azithromycin for every sniffle. It’s not safer. It’s just more expensive and worse for their gut.
My son had SSLR from cefaclor at age 3. He’s now a healthy, active kid who plays soccer. He’s never had C. diff. He’s never needed IV antibiotics. Because we asked the right question: ‘Is this an allergy-or something else?’
Doctors need to be educated. Parents need to be empowered. And the system needs to stop letting fear replace evidence.
I’m sharing this with every parent group I’m in. This is life-changing information.
Vatsal Patel
so you're telling me the pharmaceutical industry created a new diagnosis to sell more expensive drugs? genius. they knew parents would panic and avoid the real culprit-cefaclor-so they invented a fancy name to keep the whole class off the table. meanwhile, they profit from vancomycin sales. the real allergy is to profit.
and let's be real-doctors don't want to think. they want checkboxes. 'rash + antibiotic = allergy' is easier than reading a 12-page paper on T-cell mediated responses.
we're not patients. we're data points with insurance cards.
and yet somehow, we're supposed to trust them when they say 'it's safe' after they misdiagnosed us for 7 years?
the system is broken. not the science. the system.
Sharon Biggins
i just read this and cried a little. my daughter had sslr after amoxicillin when she was 2. we were told she's allergic forever. she's 8 now and gets every infection treated with azithromycin. she's had diarrhea every time. i had no idea she could've taken other antibiotics. thank you for this. i'm calling her allergist tomorrow.
John McGuirk
you think this is new? they've been doing this since the 80s. they don't want you to know you can take cephalexin. they want you to take the expensive ones. watch. next year they'll say 'oh wait, cephalexin causes sslr too' and then we'll be back to square one. it's all controlled. the labs, the docs, the codes. you think that icd-11 code is for patients? no. it's for billing.
Michael Camilleri
if your kid gets a rash after antibiotics you're a bad parent for not knowing this. why didn't you google it? why didn't you read the side effects? now your kid is on vancomycin and you're blaming the system? stop being lazy. this is basic medical literacy. if you can't read a pamphlet, don't have kids
lorraine england
thank you for writing this. i'm a nurse and i see this all the time. parents come in terrified, doctors write 'penicillin allergy' without thinking. we need more posts like this. i'm printing this out for my unit.
also-can someone explain why the urine test isn't available yet? i'd pay out of pocket for my patient.
Phil Maxwell
interesting. i didn't know sslr was that common. my cousin had it after cefaclor. they just said 'allergy' and moved on. never thought to question it. guess i'll tell her about this.
Shelby Marcel
wait so if my kid had sslr from amoxicillin can they still take amox clav? or is that the same thing? i'm so confused lol
Luke Davidson
bro this is wild. i had no idea the rash just… moved? like it had its own agenda? that’s insane. my daughter got one after amoxicillin and we thought it was chickenpox. turns out it was sslr. we were so scared we avoided every antibiotic for 4 years. she missed out on so many treatments. now i’m telling everyone. this is legit life-changing info.
also-why isn’t this in every pediatric office? why do we still have posters saying ‘penicillin allergy = no cephalosporins’? that’s like saying ‘if you’re allergic to apples you can’t eat oranges’.
and the urine test? that’s the future. i hope they roll it out fast. i’d take a pee test over a 3-hour oral challenge any day.
thank you for sharing. i’m sending this to my sister. her kid had the same thing.
Josh McEvoy
OMG i just realized my son had sslr 😭 i thought he was dying. rash everywhere, fever, crying because his knees hurt. they gave him steroids and said 'allergy'. now he's on azithromycin for everything. he's had 3 stomach bugs since. i'm calling the allergist tomorrow. thank you for this. i'm not alone 🥹
Heather McCubbin
they're not telling you the truth. sslr is just the first step. next they'll say 'oh wait, it's actually a sign of autism spectrum disorder triggered by antibiotics' and then they'll start pushing neurofeedback and special diets. this is how they control the narrative. you think they care about your kid? they care about the data. they're building a profile. every rash, every antibiotic, every diagnosis-it's all feeding the algorithm. don't trust the system. question everything.