Naloxone Dose Calculator
Naloxone Dosage Calculator
Enter information about the opioid scenario to determine how many doses of naloxone you may need.
Recommended Doses
When someone is taking opioids - whether for chronic pain, after surgery, or as part of addiction treatment - there’s a real risk they could overdose. And when that happens, time isn’t just important. It’s everything. A person can stop breathing in under two minutes. Brain damage starts soon after. Death follows quickly. But there’s a tool that can reverse this in minutes: naloxone.
What Naloxone Does - And What It Doesn’t
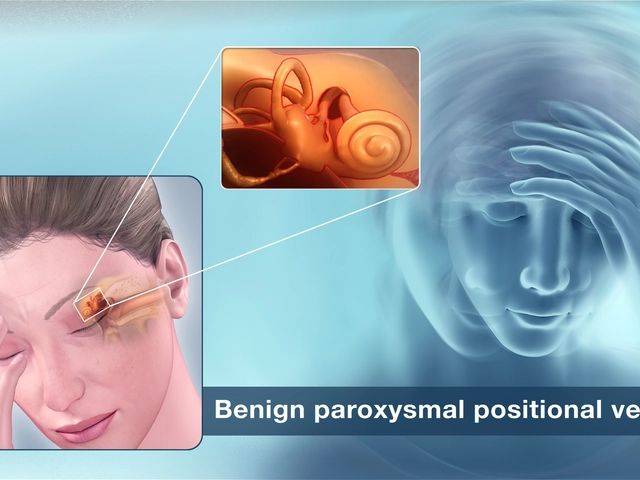
Naloxone is not a cure for addiction. It doesn’t make you feel good. It doesn’t treat pain. It’s not a sedative or a stimulant. It’s a simple, targeted drug that kicks opioids off the brain’s receptors. When someone overdoses, opioids flood those receptors and shut down breathing. Naloxone pushes them out. In 2 to 5 minutes, the person starts breathing again. That’s it. No magic. No side effects if given to someone who hasn’t taken opioids. It won’t harm them if they’re clean.
But here’s the catch: naloxone wears off in 30 to 90 minutes. Many opioids - especially fentanyl and carfentanil - last much longer. That means the person can stop breathing again after naloxone wears off. That’s called renarcotization. It’s why you can’t just give one dose and walk away. You need to call 911, stay with them, and be ready to give a second or even third dose. The CDC says up to 10mg of naloxone may be needed for fentanyl overdoses. That’s two to five nasal sprays.
Who Needs a Naloxone Readiness Plan?
It’s not just people with opioid use disorder. In fact, 86.7% of opioid overdose deaths happen to people who weren’t even prescribed opioids. But if someone is on opioids - even for a week after surgery - they’re at risk. The CDC recommends naloxone be offered to anyone prescribed more than 50 morphine milligram equivalents (MME) per day. That’s about 10 pills of 5mg oxycodone daily. But doctors are still missing the mark. Only 32.4% of primary care providers routinely talk about naloxone with high-risk patients.
And it’s not just patients. Family members, caregivers, coworkers, even teachers and bus drivers should know where naloxone is and how to use it. Workplace overdose deaths have jumped 619% since 2011. OSHA now recommends naloxone kits in any workplace with more than 15 employees. That’s not just for drug users - it’s for anyone who might be accidentally exposed, or who takes medication without telling anyone.
The Four Pillars of a Naloxone Readiness Plan
A good plan isn’t just about having the drug. It’s about having a system. Here’s what works:
- Access: Keep naloxone where it’s needed - not locked in a cabinet, not in the car, not in a drawer. In clinics, keep at least two doses in an emergency kit. In homes, keep one near the bed or in the bathroom. In workplaces, place kits within 100 feet of high-risk areas. The Wisconsin Department of Health Services says it must be reachable in under 30 seconds.
- Form: Nasal spray is easiest for non-medical people. NARCAN® 4mg spray is now available over the counter in pharmacies. No prescription needed. One spray goes in one nostril. Push the plunger all the way. That’s it. No training required. Intramuscular shots work too, but they need needles and more skill. Auto-injectors like Evzio are reliable but expensive - and getting harder to find.
- Training: You don’t need to be a nurse. But you do need to know the steps. The National Safety Council found that just 20 minutes of hands-on practice leads to 92.4% correct use. Practice on a training kit. Learn to recognize the signs: unresponsive, blue lips, slow or gasping breaths, pinpoint pupils. Then, call 911. Then, give naloxone. Then, do rescue breathing - one breath every five seconds. Don’t stop until help arrives.
- Follow-up: After naloxone, the person needs to be monitored for at least two hours. They might wake up angry, confused, or in withdrawal. That’s normal. But they could also relapse into overdose. Never leave them alone. Even if they seem fine, call 911. Always. Naloxone doesn’t fix everything. It doesn’t stop aspiration, heart problems, or muscle breakdown. Those can still kill.

Cost, Access, and the Real Barriers
People think naloxone is expensive. It’s not - if you know where to look. The nasal spray costs $130-$150 without insurance. But in 47 states, you can walk into a pharmacy and get it for free or $0 with a standing order. Pennsylvania, Georgia, South Carolina, and Oklahoma run programs that give away kits for free. Many community health centers, harm reduction groups, and even churches hand them out. You don’t need ID. You don’t need to explain why.
But awareness is still low. Only 53.2% of Americans know where to get naloxone. In the South, it’s as low as 41.6%. That’s not a medical problem. It’s a communication problem. Pharmacies still don’t always know how to dispense it. A 2022 Pennsylvania study found 68.3% of pharmacy staff needed training before they felt confident giving it out. And stigma? It’s still real. People think if you carry naloxone, you’re a drug user. That’s false. Carrying naloxone makes you a lifesaver.
What Happens When It Works - And When It Doesn’t
In Washington State, over 28,000 overdoses were reversed with naloxone in 2022. In South Carolina, 1,869 reversals came from just 12,457 kits given out in one quarter. These aren’t statistics. These are people who went home. People who hugged their kids. People who got another chance.
But it doesn’t always work. In 29% of Reddit user stories, people struggled to get the nasal spray in during a real overdose - because the person was unconscious, or the spray was too cold, or they panicked. In 78% of successful cases, rescue breathing made the difference. That’s why practice matters. And why you need to keep the kit in a warm place. Cold sprays don’t work as well.
And here’s the hard truth: naloxone can’t fix the opioid crisis. It can’t replace mental health care, housing, or treatment. Only 18.5% of people with opioid use disorder get medication-assisted treatment. That’s the real crisis. But until that changes, naloxone is the best tool we have to stop people from dying right now.

How to Build Your Own Naloxone Readiness Plan
Here’s how to get started - whether you’re a patient, a caregiver, or a workplace manager:
- Get a kit: Walk into any pharmacy. Ask for NARCAN® nasal spray. No ID, no prescription. Pay with cash if needed. Or find a local harm reduction group. Many offer free kits by mail.
- Store it right: Keep it at room temperature. Don’t leave it in the car. Don’t freeze it. Check the expiration date. Replace every 18-24 months.
- Teach someone: Show your partner, your kid, your coworker how to use it. Practice with a trainer kit. Watch a 5-minute video on the CDC website.
- Know the signs: Unresponsive. Slow breathing. Blue lips. Pinpoint pupils. If you’re unsure - give naloxone anyway. It won’t hurt.
- Call 911 first: Always. Even if they wake up. Even if they seem fine. They need medical care.
- Stay with them: Monitor for at least two hours. Be ready to give another dose if they stop breathing again.
There’s no shame in having naloxone. There’s no guilt in carrying it. It’s like having a fire extinguisher. You hope you never need it. But if you do - you’ll be glad it was there.
Can anyone use naloxone, even without training?
Yes. Naloxone nasal spray is designed for anyone to use. No medical background needed. Just follow the instructions on the box: remove the cap, insert into one nostril, press the plunger firmly. It’s simple. Training improves confidence and success rate, but it’s not required. The FDA approved over-the-counter naloxone specifically because it’s safe and easy enough for bystanders to use in an emergency.
Does naloxone work on fentanyl overdoses?
Yes - but it often takes more than one dose. Fentanyl and its analogs are 50 to 100 times stronger than morphine. A single 4mg nasal spray may not be enough. The CDC recommends giving a second dose after 2-3 minutes if breathing hasn’t returned. In severe cases, up to three or four doses may be needed. Always call 911 - even if you give multiple doses.
Is naloxone safe for children and elderly people?
Yes. Naloxone works the same way in all ages. It doesn’t matter if the person is 18 or 80. The dose doesn’t change based on weight or age. One nasal spray (4mg) is the standard dose for adults and children. If the person is unresponsive and suspected of opioid overdose, give naloxone. It won’t harm them if they didn’t take opioids.
How long does naloxone last in the body?
Naloxone lasts about 30 to 90 minutes. Many opioids - especially long-acting ones like methadone or synthetic ones like fentanyl - stay in the body much longer. This means the person can slip back into overdose after naloxone wears off. That’s why monitoring for at least two hours is critical. Always call 911 and stay with the person until help arrives.
Can I get naloxone for free?
Yes. In 47 states, you can get naloxone for free through standing order programs at pharmacies, community health centers, or harm reduction organizations. Many programs offer mail delivery. Search for your state’s naloxone program online or call your local health department. No insurance, ID, or prescription is needed. Free kits are widely available - if you know where to ask.
What if I’m afraid to call 911?
Fear of legal trouble is common, but it shouldn’t stop you. All 50 states and D.C. have Good Samaritan laws that protect people who call 911 during an overdose. You won’t be arrested for possession if you’re seeking help. Emergency responders are trained to help - not punish. Calling 911 saves lives. And if you’re unsure, just say: “I’m calling because someone stopped breathing.” That’s enough.
What Comes Next?
Having naloxone ready is the first step. The next step is to talk about it. Ask your doctor if you need it. Tell your family where it is. Train your coworkers. Push for kits in schools, gyms, libraries. The opioid crisis didn’t start with pills - it grew because no one talked about it. Naloxone changes that. It turns silence into action. And action saves lives.





Jerry Rodrigues
Naloxone should be as common as fire extinguishers in every home and workplace. No stigma, no questions asked. Just keep one handy.
Kelly McRainey Moore
I keep a kit in my glovebox and one by my bed. My sister’s a nurse and she showed me how to use it. Best 15 bucks I ever spent.
Amber Lane
My cousin overdosed last year. Naloxone saved him. He’s clean now. But he wouldn’t be here if we hadn’t had the kit.
Stephen Rock
Of course naloxone works. But why are we treating symptoms instead of fixing the root cause? People are dying because we let the pharmaceutical industry run wild and then acted surprised when people got hooked. Now we hand out nasal sprays like candy and call it progress. Pathetic.
michelle Brownsea
Let’s be clear: naloxone is not a moral license to use opioids. It’s a medical tool. But the way it’s being pushed-as if every person who takes a pill deserves a rescue kit-is deeply problematic. We’re not saving lives by enabling addiction. We’re delaying consequences. And that’s not compassion. It’s negligence dressed up as kindness.
Barbara Mahone
My brother works in a high school in rural Ohio. They’ve had three overdoses in the last two years. All were reversed with naloxone. One student is now in recovery. The school keeps kits in the nurse’s office, the gym, and the cafeteria. No one bats an eye anymore. It’s just part of the routine.
It’s not about judging. It’s about preparing.
Ashok Sakra
why dont u just let them die if they r dumb enough to do drugs? why waste money on them? they choose it. let nature take its course. save the money for real people.
Roisin Kelly
So now we’re giving free narcan to everyone? Great. Next they’ll hand out free fentanyl so we don’t have to pay for it. This is all a government scam to make people dependent. Who’s really behind these programs? Big Pharma? The DEA? Someone’s making bank off this panic.
lokesh prasanth
naloxone is good but what about the mental health part? no one talks about that. people dont overdose just cause they like drugs. its because they are in pain. no one cares.
MAHENDRA MEGHWAL
As a healthcare professional in India, I have witnessed the tragic consequences of opioid misuse in both urban and rural settings. While naloxone is a vital intervention, its accessibility remains a challenge in low-resource environments. The principles outlined in this article-access, form, training, and follow-up-are universally applicable, yet implementation requires systemic support. In many regions, cultural stigma and lack of medical infrastructure hinder even basic distribution. We must not only advocate for naloxone but also invest in community education and harm reduction frameworks tailored to local contexts. The goal is not merely to reverse overdoses, but to restore dignity and hope.
Malvina Tomja
Let’s be honest-this isn’t about saving lives. It’s about making people feel better about doing nothing else. You hand out a nasal spray and pat yourself on the back. Meanwhile, treatment centers are overcrowded, therapists are underpaid, and housing is nonexistent. You’re not solving the crisis-you’re just making it less messy. And that’s not progress. That’s performance.
Real compassion? That’s funding MAT programs. That’s building sober housing. That’s training counselors. Not giving out Narcan like party favors and calling it a day.