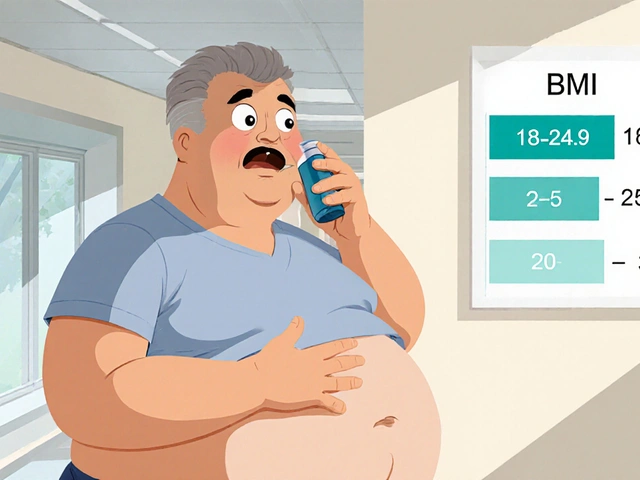
BMI-to-Asthma-Risk Estimator
Understand Your Asthma Risk
Based on research from the Journal of Allergy and Clinical Immunology, adults with BMI ≥30 kg/m² are up to 50% more likely to develop asthma.
Key Insight: Your BMI category shows how excess weight may affect your respiratory health through inflammation, mechanical restriction, and medication response.
Source: Journal of Allergy and Clinical Immunology research
When you hear the terms Obesity is a chronic condition characterized by excess body fat that raises the risk of many diseases. Asthma is a respiratory disorder marked by airway narrowing, inflammation, and episodic breathlessness. These two health challenges often appear together, and understanding why can help you take smarter steps toward better breathing and weight control.
Why the Link Matters
Studies published in the Journal of Allergy and Clinical Immunology show that adults with a body mass index (BMI) of 30kg/m² or higher are up to 50% more likely to develop asthma than people with a normal BMI. The connection isn’t just a coincidence; it’s rooted in biology, lifestyle, and treatment responses.
Key Biological Mechanisms
Several pathways explain how excess weight fuels airway problems:
- Systemic inflammation: Fat cells release cytokines such as Leptin and other adipokines that keep the immune system on high alert. Chronic low‑grade inflammation can spill over into the lungs, making airways more reactive.
- Mechanical load: Extra abdominal and chest fat restricts diaphragmatic movement, reducing lung volume and increasing the work of breathing.
- Hormonal shifts: Higher levels of estrogen and insulin resistance in obesity can alter airway smooth‑muscle tone, contributing to airway hyperresponsiveness.
- Medication efficacy: Obese patients often need higher doses of inhaled corticosteroids, yet the drugs may be less effective due to altered distribution in fatty tissue.
Statistical Snapshot
| BMI Category | Asthma Rate (%) | Relative Risk |
|---|---|---|
| Underweight (<18.5) | 5.2 | 0.9 |
| Normal (18.5‑24.9) | 7.8 | 1.0 |
| Overweight (25‑29.9) | 10.4 | 1.3 |
| Obese (≥30) | 12.9 | 1.5 |
The table highlights a clear trend: as BMI rises, so does the likelihood of having asthma. While the numbers vary by age, gender, and ethnicity, the pattern holds across most large‑scale surveys.
Risk Factors Beyond Weight
Obesity doesn’t act alone. Other contributors can amplify the asthma risk:
- Physical inactivity - sedentary habits limit lung capacity and worsen weight gain.
- Dietary patterns - high‑sugar, low‑fiber meals promote inflammation.
- Sleep apnea - common in obese individuals, it can trigger nocturnal asthma attacks.
- Genetic predisposition - families with a history of either condition may see a compounded effect.
Managing Asthma When You’re Overweight
Effective control requires a two‑pronged approach: treating the airway and addressing weight.
- Medication adjustment: Work with a pulmonologist to optimize inhaler technique and consider adding long‑acting bronchodilators if symptoms persist.
- Weight‑loss programs: Even a 5‑10% reduction in body weight can lower asthma medication use by 30% according to a 2022 randomized trial.
- Exercise prescription: Low‑impact activities such as walking, swimming, or stationary cycling improve cardiovascular fitness without triggering bronchospasm.
- Nutritional focus: Emphasize omega‑3 rich foods, antioxidants, and fiber; these nutrients can dampen systemic inflammation.
- Behavioral support: Cognitive‑behavioral therapy or group coaching helps sustain lifestyle changes and reduces stress‑related asthma flare‑ups.
Prevention Strategies for At‑Risk Populations
Public‑health programs that target childhood obesity have the added benefit of lowering future asthma rates. Schools that integrate daily activity breaks and offer healthier meals see a 15% drop in asthma‑related school absences.
For adults, regular screening of BMI during primary‑care visits allows early counseling. When a clinician spots a rising BMI, they can intervene with a brief motivational interview and a referral to a dietitian.

Common Myths Debunked
Myth 1: “Asthma always gets better after weight loss.”
Reality: Most patients experience improvement, but some retain airway hyperresponsiveness due to genetic factors.
Myth 2: “Inhalers cause weight gain.”
Reality: Inhaled corticosteroids have minimal systemic effects; weight gain is mainly driven by lifestyle and metabolic changes.
Myth 3: “You can’t exercise if you have asthma.”
Reality: Proper warm‑up, using a rescue inhaler beforehand, and choosing the right activity make exercise safe and beneficial.
Quick Takeaways
- Higher BMI increases asthma risk and can worsen existing symptoms.
- Inflammatory molecules from fat tissue, mechanical breathing limits, and hormone shifts are the main biological links.
- Even modest weight loss improves lung function and reduces medication needs.
- Combining asthma‑specific treatment with lifestyle changes yields the best outcomes.
- Early prevention-through diet, activity, and regular BMI checks-cuts long‑term disease burden.
Frequently Asked Questions
Can losing weight cure asthma?
Weight loss often reduces the frequency and severity of asthma attacks, but it rarely eliminates the condition entirely. Genetics, environmental triggers, and pre‑existing airway changes still play a role.
Which type of exercise is safest for someone with asthma and obesity?
Low‑impact, rhythmic activities like walking, swimming, and stationary cycling are ideal. They raise heart rate without causing rapid, cold‑air inhalation that can provoke bronchospasm.
Do inhaled steroids affect weight?
Inhaled steroids act locally in the lungs and have a negligible impact on body weight. Systemic steroids taken orally or intravenously are more likely to cause weight gain.
How quickly can I expect asthma improvement after losing weight?
Patients often notice better symptom control within 3-6 months of a 5‑10% weight reduction, especially when combined with optimized medication.
Is there a specific BMI target for asthma patients?
A BMI below 25kg/m² is generally considered optimal for reducing asthma‑related complications, but individualized goals should consider overall health, muscle mass, and comorbidities.




John Blas
Wow, this article just threw a mountain of data at us like a drama queen at a red carpet event. I can almost hear the sighs of every lazy critic scrolling past. The connection between obesity and asthma is certainly a hot topic, but the write‑up feels like it’s trying too hard to be epic.
Matthew Marshall
Actually, the link isn’t that dramatic – it’s just a straightforward metabolic correlation.
Lexi Benson
Oh great, another “must‑read” piece about weight and breathing – because that’s exactly what I was hoping for on a lazy Sunday. If sarcasm burned calories, we’d all be fit by now.
Vera REA
The statistical snapshot provided aligns well with the CDC’s recent findings. It’s helpful that the article lists specific BMI categories and corresponding asthma rates. The clarity makes it easier for clinicians to discuss risk with patients.
John Moore
I appreciate the balanced tone here – it acknowledges the problem without shaming anyone. Encouraging lifestyle changes alongside proper asthma management can really make a difference. Let’s keep the conversation supportive and fact‑based.
Adam Craddock
From a clinical perspective, the mechanistic pathways described are consistent with current immunological models. Systemic inflammation and mechanical load both contribute to airway hyper‑responsiveness. Further research into pharmacokinetic alterations in obese patients would be valuable.
SHIVA DALAI
Picture this: a world where every breath feels like trying to draw air through a thick, unyielding blanket. That is the daily reality for countless individuals who juggle the twin burdens of obesity and asthma. The article does a commendable job of outlining the physiological culprits – from leptin‑driven cytokine storms to the suffocating mechanical pressure of excess abdominal fat. Yet, the narrative often glosses over the emotional toll of navigating a healthcare system that often blames the patient. Imagine the frustration of stepping into a clinic, inhaler in hand, only to be told the solution is “just lose weight.” It’s a message that can feel both patronizing and dismissive. Moreover, the interplay between insulin resistance and airway smooth‑muscle tone adds another layer of complexity that many patients are unaware of. When medication efficacy wanes because fatty tissue sequesters inhaled corticosteroids, dosage adjustments become a maze of trial and error. The article wisely highlights the need for higher steroid doses, but it stops short of exploring alternative delivery mechanisms such as spacer devices or nebulized therapy, which can sometimes bypass the adipose barrier. Additionally, the sociocultural dimensions are barely touched upon – socioeconomic status, food deserts, and limited access to fitness resources all exacerbate the obesity‑asthma cycle. The risk calculator is a nifty tool, but without proper context, users might misinterpret a “high risk” label as a fatal verdict rather than a call to proactive management. Lifestyle interventions, like incorporating interval training or adopting anti‑inflammatory diets rich in omega‑3 fatty acids, can shift the balance in favor of better lung function. Finally, the article could benefit from a deeper dive into emerging therapies, such as biologics targeting IL‑5 or IL‑13, which show promise in phenotypes linked to obesity‑related inflammation. In sum, while the piece offers a solid foundation, a more holistic approach that weaves together physiological, psychological, and socioeconomic strands would paint a truer picture of the battle these patients face each day.
Vikas Kale
Leveraging the mechanistic lexicon, one must consider adipokine‑mediated eosinophilic modulation as a pivotal node in the pathobiology. The pharmacodynamic attenuation observed aligns with volume of distribution shifts inherent to lipophilic drug reservoirs. Integrating precision‑medicine algorithms could stratify patients based on BMI‑adjusted dose‑response curves. Ultimately, therapeutic optimization demands a multimodal framework.
Mr. Zadé Moore
Honestly, this is just fear‑mongering dressed up as science.
Brooke Bevins
I feel for anyone battling both conditions; the daily struggle is real. But let’s be clear: we need more actionable guidance, not just statistics.
Vandita Shukla
Speaking from experience, the article overlooks the cultural dietary patterns that drive obesity in certain communities. Ignoring these factors only widens the health gap.
Susan Hayes
As an American, I can’t help but notice how foreign research gets front‑page treatment while our own health policies lag. We need home‑grown solutions, not imported hype.
Deepak Bhatia
Stay hopeful, every small step counts!
Samantha Gavrin
One can’t ignore the hidden agenda behind the obesity‑asthma narrative; it conveniently fuels pharmaceutical profit motives. While the data looks solid, the framing raises red flags about industry influence. Stay vigilant when interpreting such health claims.