More than 70% of people with asthma or COPD are using their inhalers wrong. Not because they don’t want to get better, but because no one ever showed them how to do it right. You might be one of them. You’ve been using your inhaler for years, maybe even decades. You press the canister. You breathe in. You feel like it’s working. But here’s the truth: if you’re not doing it exactly right, less than a third of your medicine is actually reaching your lungs. The rest? It’s stuck in your mouth, throat, or wasted in the air. That’s why your symptoms don’t improve - not because the drug doesn’t work, but because you’re not delivering it where it needs to go.
Why Technique Matters More Than the Device
It doesn’t matter if you’re using a fancy new inhaler or the same one your doctor gave you ten years ago. What matters is how you use it. Studies show that when people use their inhalers correctly, 40-60% of the medicine reaches the lungs. When technique is off, that number drops to 8-30%. That’s not a small difference. That’s the difference between controlling your symptoms and ending up in the emergency room.
There are three main types of inhalers: metered-dose inhalers (MDIs), dry powder inhalers (DPIs), and soft mist inhalers. Each works differently. MDIs use a pressurized canister that sprays medicine when you press it. DPIs rely on your own strong, fast breath to pull the powder into your lungs. Soft mist inhalers release a slow cloud you breathe in gently. You can’t use them the same way. Using a DPI like an MDI - pressing and puffing slowly - will give you almost nothing. Using an MDI without a spacer? You’re losing most of your dose.
Doctors often pick an inhaler based on cost, availability, or habit. But the best device is the one you can use correctly. If you’re older, have weak lungs from COPD, or struggle to coordinate your breath with a button press, a DPI might be useless. If you can’t breathe in hard and fast, an MDI with a spacer is your best bet. Technique isn’t just important - it’s the deciding factor in whether your treatment works at all.
How to Use a Metered-Dose Inhaler (MDI) Right
MDIs are the most common. Brands like ProAir HFA, Ventolin HFA, and Flovent HFA all work the same way. Here’s the correct sequence - and yes, every step matters:
- Remove the cap and shake the inhaler well for 5 seconds. If you skip this, the medicine settles at the bottom and you’ll get uneven doses.
- Hold the inhaler upright, with the mouthpiece at the bottom. Point it toward the back of your throat, not straight into your mouth.
- Breathe out fully - away from the inhaler. Don’t exhale into it.
- Place the mouthpiece between your lips and seal your lips tightly around it.
- Start breathing in slowly and deeply through your mouth. As soon as you begin inhaling, press the canister down once. This is the hardest part. Too early or too late, and the medicine hits your throat instead of your lungs.
- Keep breathing in slowly for 3-5 seconds until your lungs feel full.
- Hold your breath for 10 seconds. This lets the medicine settle into your airways. If you exhale right away, you lose up to 30% of the dose.
- Breathe out slowly through your nose.
If you’re using an inhaled corticosteroid - like fluticasone or budesonide - rinse your mouth with water and spit it out after. This cuts your risk of oral thrush by 75%. Don’t swallow the water. Just rinse and spit.
Now, here’s the game-changer: use a spacer. A spacer is a plastic tube that attaches to your MDI. It holds the medicine after you press it, giving you time to breathe in slowly. Studies show spacers boost lung delivery by 70-100%. They’re especially crucial for kids, older adults, and anyone who struggles with timing. You don’t need a fancy one. Even a basic plastic spacer works. And no, you can’t use a spacer with a DPI. That’s a common mistake.
How to Use a Dry Powder Inhaler (DPI) Right
DPIs like Diskus, Turbuhaler, and Ellipta don’t use propellant. Instead, they rely on your breath to pull the powder into your lungs. That means you need to inhale fast and hard - not slow and gentle. If you breathe too slowly, the powder won’t scatter. It just sticks in your throat and you taste it. That’s not just annoying - it’s ineffective.
Here’s how to use a DPI correctly:
- Load the dose as instructed. For Diskus, slide the lever until you hear a click. For Turbuhaler, twist the base until it clicks. Never remove the capsule - that’s a mistake 15% of users make, and it ruins the dose.
- Hold the inhaler level. Don’t tilt it up or down.
- Breathe out fully - away from the device. Don’t exhale into it.
- Put the mouthpiece in your mouth and seal your lips tightly.
- Inhale quickly and deeply - like you’re trying to suck a thick milkshake through a straw. You should hear a slight whirring sound.
- Hold your breath for 10 seconds.
- Breathe out slowly.
DPIs are great if you can breathe in hard. But if you have severe COPD, or if you’re older and your lungs are weak, you might not generate enough airflow. The European Respiratory Journal found that 62% of patients over 65 couldn’t use DPIs properly because they couldn’t inhale fast enough. If your inhaler isn’t working and you’re over 65, ask your doctor about switching to an MDI with a spacer.
Also, don’t use a spacer with a DPI. It doesn’t help - it makes things worse. Studies show it cuts delivery by 50-70%. The powder needs that strong rush of air to become airborne. A spacer blocks it.

Soft Mist Inhalers and Other Devices
Soft mist inhalers like Respimat are newer and designed to be easier to use. They release a slow, fine mist over 1.5 seconds - no need to coordinate your breath with a button press. You just breathe in slowly and steadily.
Here’s how to use one:
- Prime it as instructed (usually once before first use or after 2 weeks without use).
- Hold it upright and point it toward the back of your throat.
- Breathe out slowly - away from the device.
- Place the mouthpiece in your mouth and close your lips around it.
- Start breathing in slowly and deeply. The device releases the mist automatically as you inhale.
- Hold your breath for 10 seconds.
- Breathe out slowly.
These are good for people who struggle with timing or strength. But they’re more expensive, and not all insurance plans cover them. If you’re having trouble with MDIs or DPIs, ask your doctor if a soft mist inhaler is an option.
Common Mistakes (And How to Fix Them)
Here are the top mistakes people make - and how to avoid them:
- Not shaking the MDI - 45% of users skip this. Shake it for 5 seconds before every puff. It’s not optional.
- Exhaling into the inhaler - 27% do this. Always breathe out away from the device. Moisture ruins the dose.
- Not holding your breath - 63% don’t hold for 10 seconds. This is the biggest waste. Hold it. Even if it feels awkward.
- Using multiple inhalers without training - If you have two different types, you’re at higher risk of mixing up technique. The European Respiratory Society says this cuts effectiveness by 35-50%.
- Storing inhalers in hot places - Don’t leave them in your car or near a heater. Temperatures above 30°C reduce potency by 15-20%. Keep them at room temperature.
And one more thing: never try to clean a DPI with water. Don’t wash the mouthpiece. Don’t rinse the capsule. Just wipe it gently with a dry cloth. Moisture turns the powder into a clump - and you won’t get your dose.

When to Ask for Help
You shouldn’t have to guess how to use your inhaler. Every doctor visit is a chance to check your technique. The American Lung Association and the National Asthma Council Australia both recommend that your technique be assessed at every appointment. If your doctor doesn’t ask, ask them.
Bring your inhaler to your next visit. Ask: "Can you watch me use this?" Show them how you do it. They’ll spot mistakes you didn’t even know you were making. Some clinics even have inhaler trainers - devices that light up or beep if you’re not breathing right. Ask if yours has one.
YouTube has great videos. So do the American Lung Association and Asthma UK. But videos aren’t enough. Watching isn’t the same as doing. You need feedback. If you’re still having trouble after watching a few videos, schedule a session with a respiratory therapist. They’re trained to teach this stuff. And they’re often overlooked.
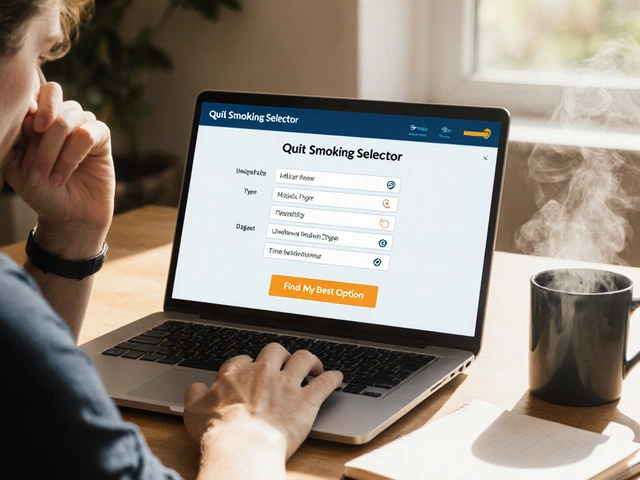
What’s Changing - and What’s Coming
Technology is catching up. Smart inhalers with built-in sensors - like Propeller Health - now track when and how you use your device. They connect to your phone and tell you if you’re breathing too slowly, missing doses, or not holding your breath. In 2022, a study in Annals of Internal Medicine found these sensors are 92% accurate. They’re not magic, but they’re helping people get better.
By 2025, nearly half of all inhalers are expected to have some kind of digital tracking. The goal? Cut improper use from 70-90% down to 30-40%. That’s huge. But for now, the best tool you have is still your own breath - and knowing how to use it right.
Final Takeaway
Your inhaler isn’t broken. You’re not failing. You just weren’t taught how to use it. And that’s not your fault. But now you know. The medicine works. The devices work. But only if you do your part. Shake, breathe in slow and deep, hold your breath for 10 seconds, rinse your mouth, and never skip the spacer if you’re using an MDI. Do those things, and you’ll get the full benefit of your treatment. No more guessing. No more wasted doses. Just better breathing - day after day.


Isaac Jules
70% of people use inhalers wrong? That’s not a healthcare failure-that’s a systemic lie. Doctors hand out devices like candy and never check technique. You think they care? They get paid for prescriptions, not outcomes. This post is right, but the system is rigged. 🤡
Lily Lilyy
You are not alone. You are not failing. You are just waiting for someone to show you the way. And now you know. Breathe slow. Hold it. Rinse. You’ve got this. 💪🌸
Susan Arlene
i always just pressed and breathed. never thought about holding my breath for 10 sec. guess thats why i still wheeze after my puff. oops
Tom Swinton
I’ve been using my MDI for 18 years, and I never knew about the spacer. I thought it was just for kids. I’ve been wasting 70% of my medication this whole time. I feel like an idiot. But now I know. I’m ordering a spacer today. I’m going to start holding my breath. I’m going to rinse. I’m going to shake. I’m going to do it right. I’m not giving up on my lungs. Not anymore.
Leonard Shit
lol i used my dpi like an mdi for 5 years. my doctor never said anything. i just thought i was bad at breathing. turns out i was just using the wrong technique. also, why do people think spacers work on dpis? that’s like putting a funnel on a vacuum. 🤦♂️
Gabrielle Panchev
This is all just corporate propaganda. The real reason your inhaler doesn’t work is because Big Pharma doesn’t want you to breathe well-they want you to buy more. They design inhalers to be confusing so you keep coming back. Spacers? That’s just a way to upsell you on plastic tubes. They don’t care if you live or die-they care about quarterly profits.
Melanie Clark
You think this is about technique? No. You think it’s about education? No. It’s about control. They don’t want you to master your inhaler. They want you dependent. They want you afraid. They want you thinking you need the next prescription, the next device, the next ‘upgrade.’ Your lungs are being weaponized against you. And you’re still reading this like it’s advice. Wake up.
Harshit Kansal
bro i just use my inhaler like a vape. puff puff. no shaking no holding no nothing. still alive. maybe the medicine is just strong enough to survive my dumbass technique lol
Brian Anaz
Americans can’t even use a simple inhaler right? We’re falling behind. In my country, we learn this in middle school. You don’t get a driver’s license until you can use a medical device properly. Maybe we need to start testing people before they get prescriptions. This is embarrassing.
Vinayak Naik
i work in pharmacy and i see this every day. old folks using dpi like mdis. teens using mdis without spacer. everyone thinks its just press and breathe. i tell them, they nod, then go home and do the same thing. its sad. but hey, at least they come back for refills
Saylor Frye
The real issue here is that the medical-industrial complex has commodified breathing. A spacer? How quaint. I use a nebulizer. It’s 2025. You’re still using analog devices? If you can’t afford a smart inhaler with Bluetooth sync, you’re already behind. This post is charmingly archaic.
Kiran Plaha
i never knew you had to shake it. i just thought you had to press it. i’ve been using my inhaler for 12 years. i guess i was lucky. but now i’ll try it right. thanks for the info. i appreciate it
Matt Beck
Breath is the original AI. The body knows. The lungs remember. The spacer? Just a bridge between the mechanical and the metaphysical. We’ve forgotten how to inhale with intention. This isn’t about technique-it’s about alignment. 🌬️🌀
Kelly Beck
You’re doing better than you think. Even reading this means you care. That’s half the battle. Now go get a spacer. Practice the 10-second hold. Rinse your mouth. You’re not broken-you’re just learning. And every time you do it right, you’re giving your future self a gift. I believe in you. 💙
Isaac Jules
You think a spacer is the solution? Try getting one covered by insurance. Try getting your doctor to even mention it. Try not being treated like a dumb patient who doesn’t know how to breathe. This whole thing is a joke. The system doesn’t want you to succeed. It wants you to keep buying.