Systemic Exposure: What It Means and Why It Matters for Your Medications
When you take a pill, it doesn’t just sit in your stomach—it travels through your body, gets absorbed into your blood, and reaches your organs. That journey is called systemic exposure, the total amount of a drug that enters your bloodstream and becomes available to affect your body. Also known as bioavailability, it’s not just about how much you swallow—it’s about how much actually does something inside you. Two people taking the same dose of the same drug can have wildly different levels in their blood. Why? Because of how their bodies process it: digestion, liver function, kidney health, even what they ate that day.
Therapeutic drug monitoring, the practice of measuring drug levels in the blood to ensure they’re in the safe and effective range exists because systemic exposure isn’t predictable for everyone. Take theophylline, used for asthma. A tiny change in dose or a new antibiotic can spike levels into the toxic range. That’s why doctors check blood levels—it’s not about the pill you took, it’s about what your body actually absorbed. The same goes for pharmacokinetics, how your body moves a drug through absorption, distribution, metabolism, and elimination. If your liver breaks down a drug too fast, you won’t get enough benefit. Too slow? You risk overdose. This is why some drugs need strict dosing rules, while others can be taken more freely.
Systemic exposure also explains why some medications cause side effects you didn’t expect. A drug might be meant for your lungs, but if too much gets into your bloodstream, it can affect your heart, your nerves, or your kidneys. That’s why ECG monitoring is required for certain antibiotics like azithromycin—they can mess with heart rhythm if systemic exposure is too high. Or why goldenseal can interfere with metformin: it changes how your body absorbs the drug, lowering its effectiveness. Even something as simple as a cold medicine can be dangerous for someone on warfarin, because the interaction changes how much of either drug stays in your system.
Understanding systemic exposure isn’t just for doctors. It’s why generic drugs look different but work the same—they deliver the same amount of active ingredient into your blood. It’s why you need to tell your pharmacist about every supplement you take. It’s why some people need blood tests, and others don’t. It’s the hidden reason some medications work wonders for you but fail for someone else. If you’re on a drug with a narrow therapeutic window, or if you’ve ever wondered why your doctor ordered a lab test after you started a new pill, this is why.
Below, you’ll find real-world examples of how systemic exposure affects everything from diabetes meds to antibiotics, heart drugs to pregnancy-safe options. These aren’t theoretical discussions—they’re stories of people who got sick, got better, or nearly didn’t make it because of how their body handled what they swallowed. You’ll learn what to watch for, when to ask for a test, and how to avoid hidden risks you didn’t even know existed.
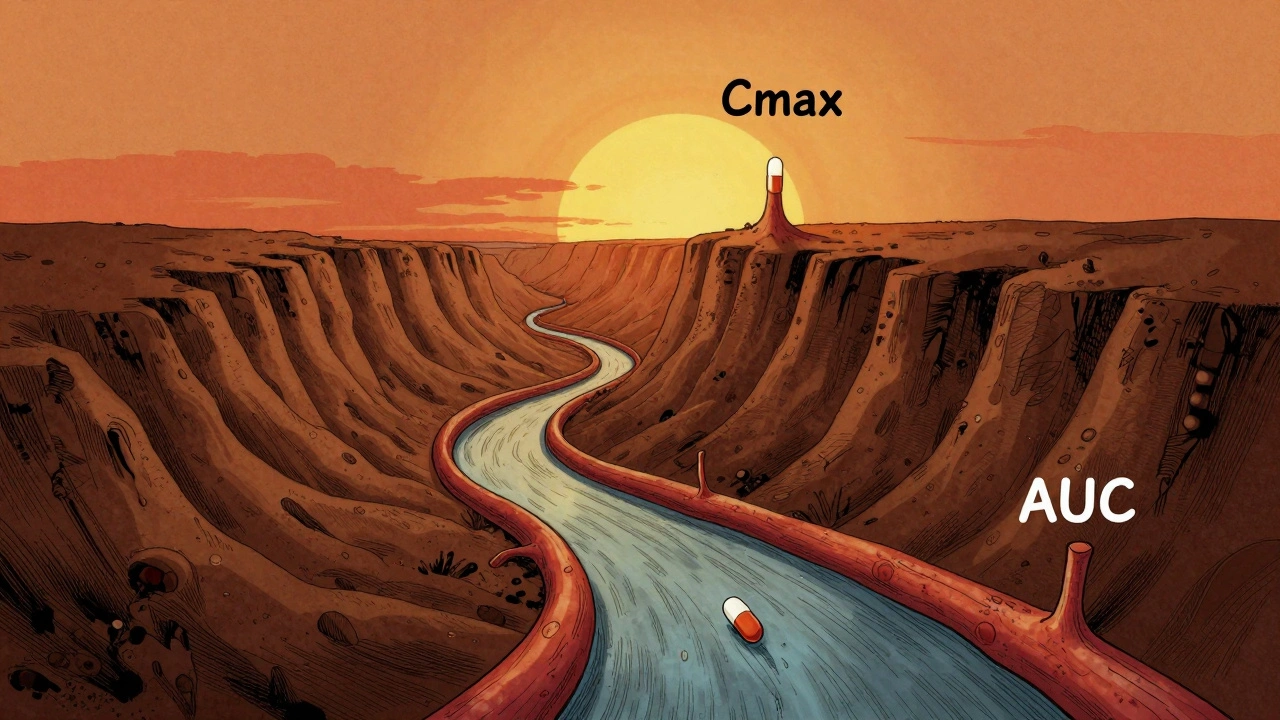
Cmax and AUC are the two key measurements used to prove generic drugs work the same as brand-name versions. Cmax shows peak concentration, while AUC measures total exposure. Both must fall within 80%-125% to be approved.