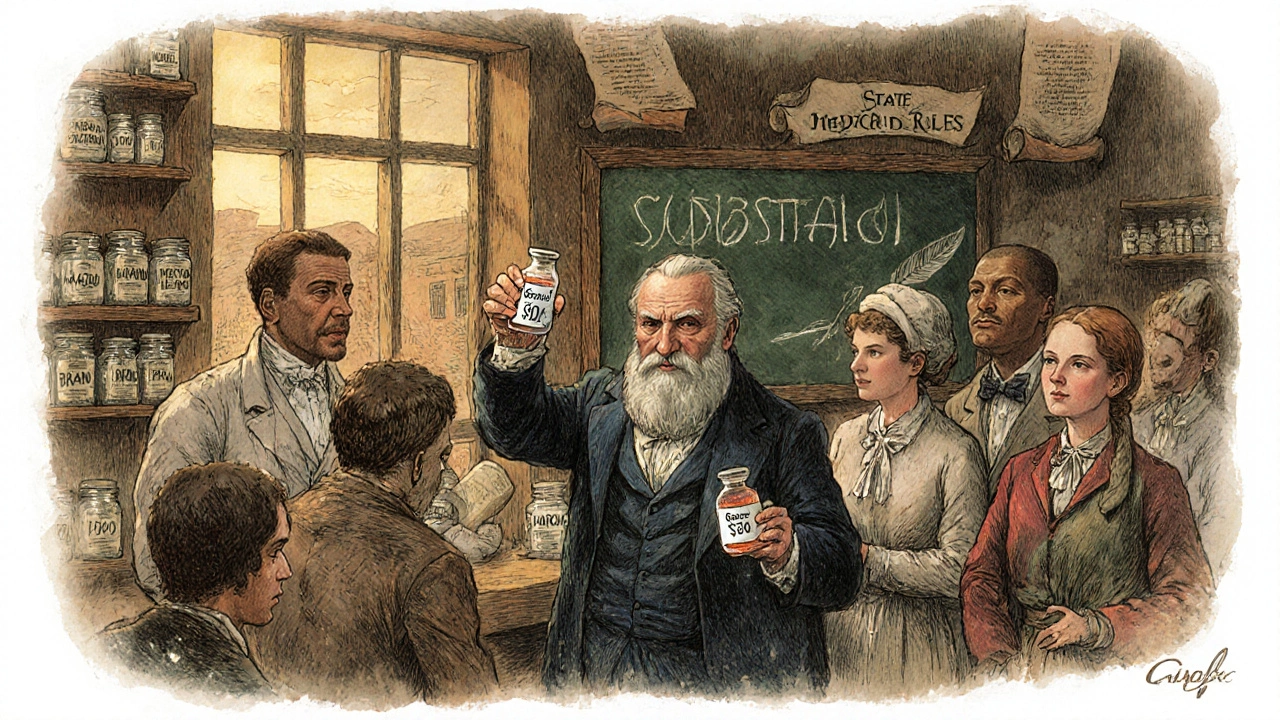
State Drug Policies: What You Need to Know About Generic Substitution, Prescribing Rules, and Patient Rights
When you pick up a prescription, state drug policies, the laws that govern how medications are dispensed, priced, and substituted at the pharmacy level across each U.S. state. Also known as pharmaceutical regulation laws, these rules decide whether your brand-name drug gets swapped for a cheaper generic — and when that swap is allowed, blocked, or requires your doctor’s approval. These aren’t federal rules. They vary wildly from state to state, and they directly impact how much you pay, what drugs you get, and even whether a pharmacist can make a change without calling your doctor.
One of the biggest pieces of generic substitution, the practice of replacing a brand-name drug with a chemically identical generic version. Also known as therapeutic equivalence, it’s a cost-saving tool built into most state laws. But not all drugs are treated the same. For example, some states require pharmacists to substitute generics for blood pressure meds like lisinopril — but block substitutions for epilepsy drugs like carbamazepine, where even tiny differences in absorption can cause seizures. Then there’s pharmacist substitution rules, the legal framework that tells pharmacists when they can switch meds, when they must notify the patient, and when they need a prescriber’s OK. In some states, you have to sign a form before a generic is given. In others, the pharmacist just does it and tells you afterward. And in a few, they can’t substitute at all for certain high-risk drugs.
These policies also cover drug pricing laws, how states set price caps, require transparency from manufacturers, or limit what pharmacies can charge for cash-paying patients. Some states now require pharmacies to show you the cash price before you pay — so you can compare it to your insurance copay. Others force manufacturers to justify price hikes over 10% in a year. And then there’s prescription regulations, the limits states place on how much of a drug you can get at once, how often you can refill, and whether controlled substances need special paperwork. These rules affect everything from painkillers to ADHD meds to insulin.
None of this is random. These policies exist because of real problems: patients skipping doses because they can’t afford their meds, pharmacists being forced to follow confusing or conflicting rules, and insurance companies pushing for cheaper options that don’t always fit the patient’s needs. That’s why the posts below dive into the real-world impact — like how a pharmacist in Texas can’t swap a transplant drug without a doctor’s note, but one in New York can. Or how a patient in Ohio got stuck paying $300 for a generic because state law didn’t require the pharmacy to disclose the cash price. These aren’t theoretical debates. They’re daily decisions that affect your health, your wallet, and your trust in the system.
What you’ll find here are clear, no-fluff explanations of the laws that actually touch your medicine cabinet — from the fine print on your prescription label to the hidden rules that determine whether you get the drug you need, when you need it, and at a price you can afford.
States are using copay differentials, preferred drug lists, and pharmacist substitution rules to push patients toward cheaper generic drugs. These policies save billions-but can also cause shortages if manufacturers pull out due to rebate rules.