Pharmacist Substitution Rules: What You Can and Can't Swap at the Pharmacy
When you pick up a prescription, you might notice the pharmacist hands you a different brand than what your doctor wrote. That’s not a mistake—it’s pharmacist substitution rules, the legal framework allowing pharmacists to swap prescribed medications with FDA-approved generic or therapeutically equivalent alternatives. Also known as drug interchangeability, it’s designed to cut costs without reducing effectiveness. In Canada, these rules are set by provincial pharmacy colleges, but they all follow the same basic principle: if a generic version exists and is approved, the pharmacist can switch it unless the doctor says "dispense as written" or "no substitution." You don’t need to ask—unless you want to.
But not all drugs are up for swap. generic drug substitution, the most common form of pharmacist substitution. Also known as prescription switching, it works for things like statins, blood pressure meds, and antibiotics—drugs where bioequivalence is proven and well-documented. You won’t see it happen with thyroid meds like levothyroxine, where tiny differences in absorption can throw off your entire treatment. Same goes for narrow therapeutic index drugs like warfarin or lithium. Pharmacists are trained to know which switches are safe and which aren’t. If you’re unsure, ask. A good pharmacist will explain why they switched—or why they didn’t.
Some people worry switching brands means lower quality. That’s not true. Generic drugs must meet the same standards as brand-name versions. The only differences are in color, shape, or inactive ingredients—nothing that changes how the drug works in your body. What changes is the price. A generic version of a cholesterol drug might cost $15 instead of $150. That’s why pharmacy laws, the rules that govern how pharmacists handle substitutions. Also known as prescription switching, it’s built to protect your wallet and your health at the same time. These laws vary by province, but they all require pharmacists to document substitutions and notify you when they happen. You have the right to refuse a substitution. If you prefer the brand, say so. If you’re cost-sensitive, ask if there’s a generic available. It’s your prescription—and your money.
What you’ll find in the posts below are real-life examples of how these rules play out. You’ll see how a switch from Prograf to a generic tacrolimus affects transplant patients, why certain antibiotics can’t be swapped without risk, and how drug interactions with birth control or diabetes meds make substitution more complex than it looks. You’ll also learn what to do if your pharmacist refuses to switch a drug, how to check if a generic is truly equivalent, and why some people get different results after a switch—even when it’s supposed to be safe. These aren’t theoretical discussions. They’re based on real cases, real patients, and real pharmacy practice.
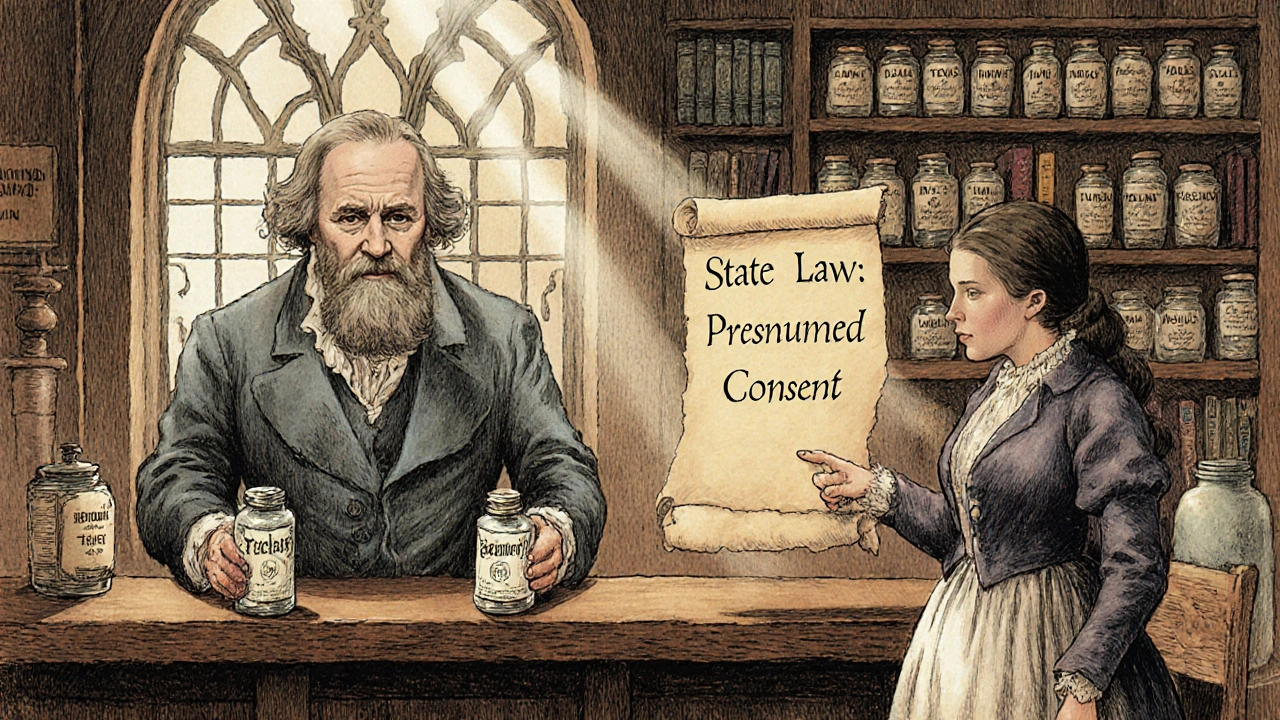
State laws on generic drug substitution vary widely across the U.S., affecting how and when pharmacists can swap brand-name drugs for cheaper generics. Learn how rules differ by state, what risks exist for critical medications, and what patients and pharmacists need to know.