Pharmaceutical Patents: How They Shape Drug Access, Costs, and Generic Options
When you buy a medicine, what you’re really paying for isn’t just the pill—it’s the pharmaceutical patents, legal protections that give drug companies exclusive rights to sell a medicine for a set time. Also known as drug exclusivity, these patents are the reason brand-name drugs like Prograf or Rosuvastatin cost so much at first. Once they expire, cheaper versions can enter the market—but until then, you’re stuck with the high price tag.
That’s why generic drugs, medicines with the same active ingredients as brand-name versions but sold after patents expire. Also known as generic medications, they’re not cheaper because they’re weaker—they’re cheaper because the patent protection has ended. The FDA requires generics to work the same way, look different only because of trademark rules, and meet the same safety standards. But here’s the catch: patent laws aren’t always straightforward. Companies sometimes file new patents on tiny changes—like a new coating or dosage form—to delay generics. This is called evergreening, and it keeps prices high even when the original patent should’ve expired.
Meanwhile, drug pricing, the cost of medicines to patients and insurers, is tightly tied to patent status. Also known as pharmaceutical cost structures, it’s why some people pay hundreds for a brand-name drug while others pay $10 for the generic. States are starting to push back with laws that reward pharmacists for switching to generics—but if manufacturers can’t make enough profit, they pull out, causing shortages. That’s what happened with some essential antibiotics and heart meds: patents expired, but no one made the generic because the price was too low.
And then there’s patent expiration, the moment when other companies can legally make and sell the same drug. Also known as patent cliff, it’s when prices drop fast—sometimes by 80% or more. But not all patents expire at the same time. A drug might have multiple patents covering its formula, delivery method, and even how it’s used. That’s why you might see a new version of a drug pop up right before the old patent runs out—it’s a legal trick to keep the monopoly going.
What you’ll find in these posts isn’t just theory. It’s real-world stuff: how generic substitution laws vary by state, why your metformin might not work as well if you take goldenseal, how to spot a fake pharmacy selling expired or copied drugs, and why some antibiotics cause sunburns while others don’t. These aren’t random topics—they’re all connected to the same root issue: who controls access to medicine, and when? Whether you’re managing diabetes, on a blood thinner, or just trying to save money on prescriptions, understanding how patents work helps you make smarter choices. You’re not just reading about drugs—you’re learning how to navigate a system built on legal timelines, corporate profits, and patient needs.
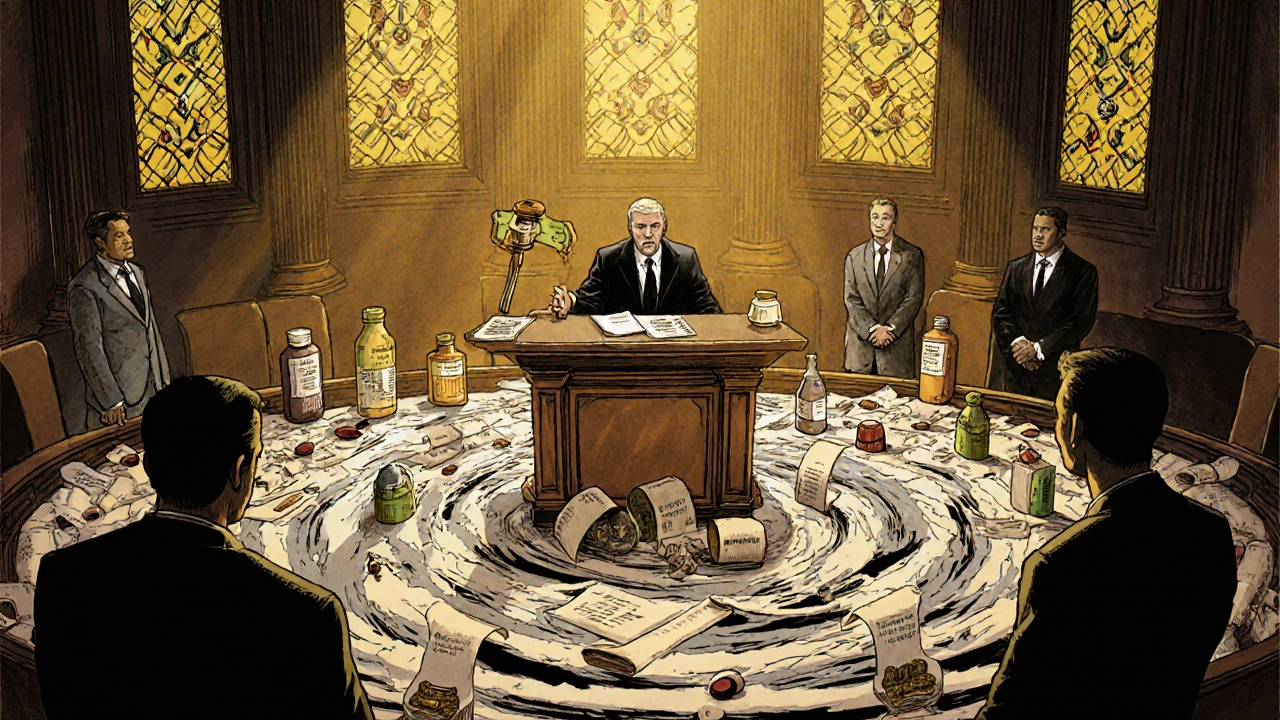
The Federal Circuit Court has exclusive authority over all U.S. pharmaceutical patent cases, shaping how generics enter the market, what dosing regimens can be patented, and where lawsuits can be filed. Its rulings directly impact drug prices and innovation.