Older Adult Medications: Safe Use, Interactions, and What You Need to Know
When you’re over 65, your body processes older adult medications, drugs taken by seniors that often require adjusted dosing due to reduced kidney or liver function. Also known as geriatric medications, these are not just weaker versions of adult drugs—they need careful handling because small changes can lead to big problems. Many seniors take five or more prescriptions at once, and that’s where things get risky. A drug that’s fine on its own can turn dangerous when mixed with another, especially if one affects the liver or kidneys. That’s why medication interactions, harmful reactions between two or more drugs that alter how they work in the body are one of the top causes of hospital visits in older adults.
It’s not just about what’s in the bottle. drug safety, the practice of using medications correctly to avoid harm, including proper dosing, storage, and monitoring matters more than ever. For example, theophylline, used for asthma and COPD, has a narrow window between helping and harming. Too little won’t work. Too much can cause seizures or heart failure. That’s why therapeutic drug monitoring, regular blood tests to check if a drug is at the right level in your system is critical for some older adult medications. Even common over-the-counter cold meds can interfere with blood thinners like warfarin, raising the risk of bleeding. And let’s not forget that many seniors take supplements—like goldenseal or berberine—that can quietly mess with diabetes drugs or blood pressure pills.
Most medication errors happen at home, not in hospitals. A pill gets mixed up. A dose is skipped. A new drug is added without telling the doctor. These aren’t mistakes from carelessness—they’re often caused by cluttered pill organizers, poor lighting, or confusing labels. That’s why keeping a simple, updated list of everything you take—including vitamins and herbs—is one of the best things you can do. It’s not just for your doctor. It’s for your pharmacist, your family, and even your emergency responders.
There’s no one-size-fits-all when it comes to older adult medications. What works for one person might be dangerous for another. That’s why the posts below cover real situations: how to check REMS requirements before starting a new drug, why ECGs matter before taking certain antibiotics, how to spot dangerous side effects before they become emergencies, and what to do when generics look different than what you’re used to. You’ll find practical advice on avoiding interactions, understanding test results like Cmax and AUC, and recognizing when a medication might be doing more harm than good. This isn’t theory. These are the things that keep people out of the ER and help them stay independent longer.
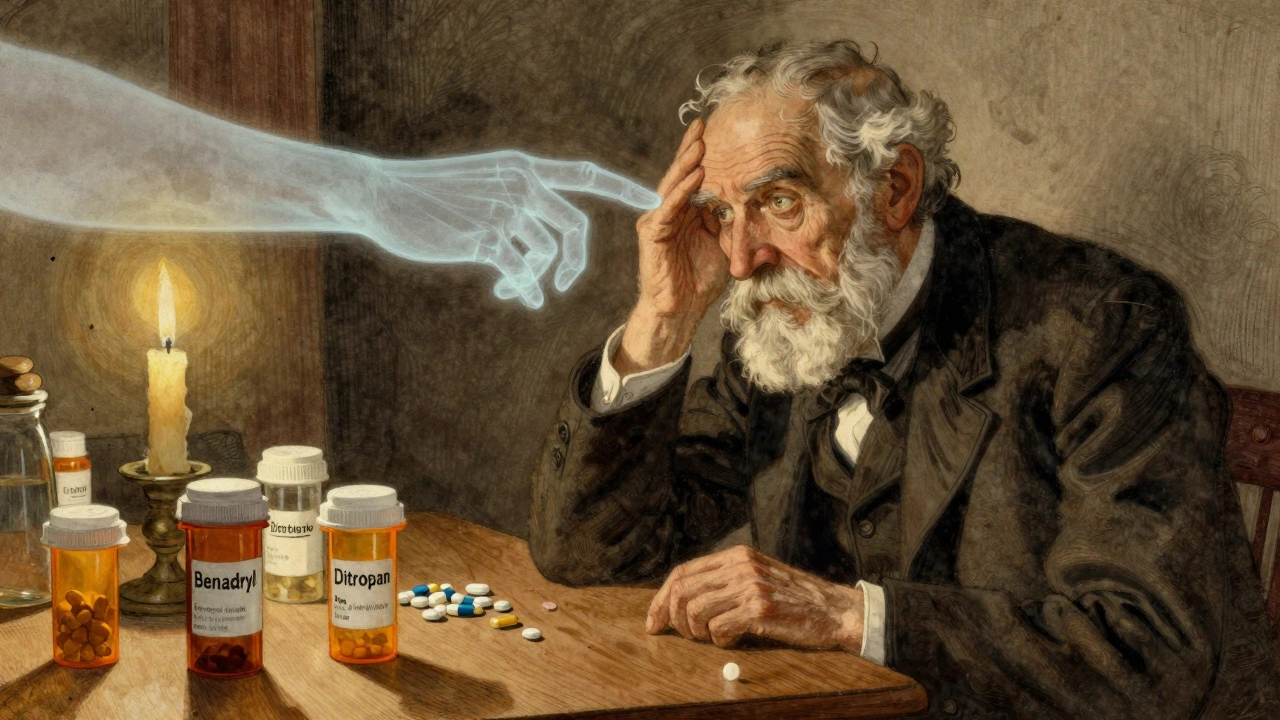
Anticholinergic burden from common medications like Benadryl and oxybutynin can accelerate memory loss and increase dementia risk in older adults. Learn which drugs to avoid and how to safely reduce cognitive harm.