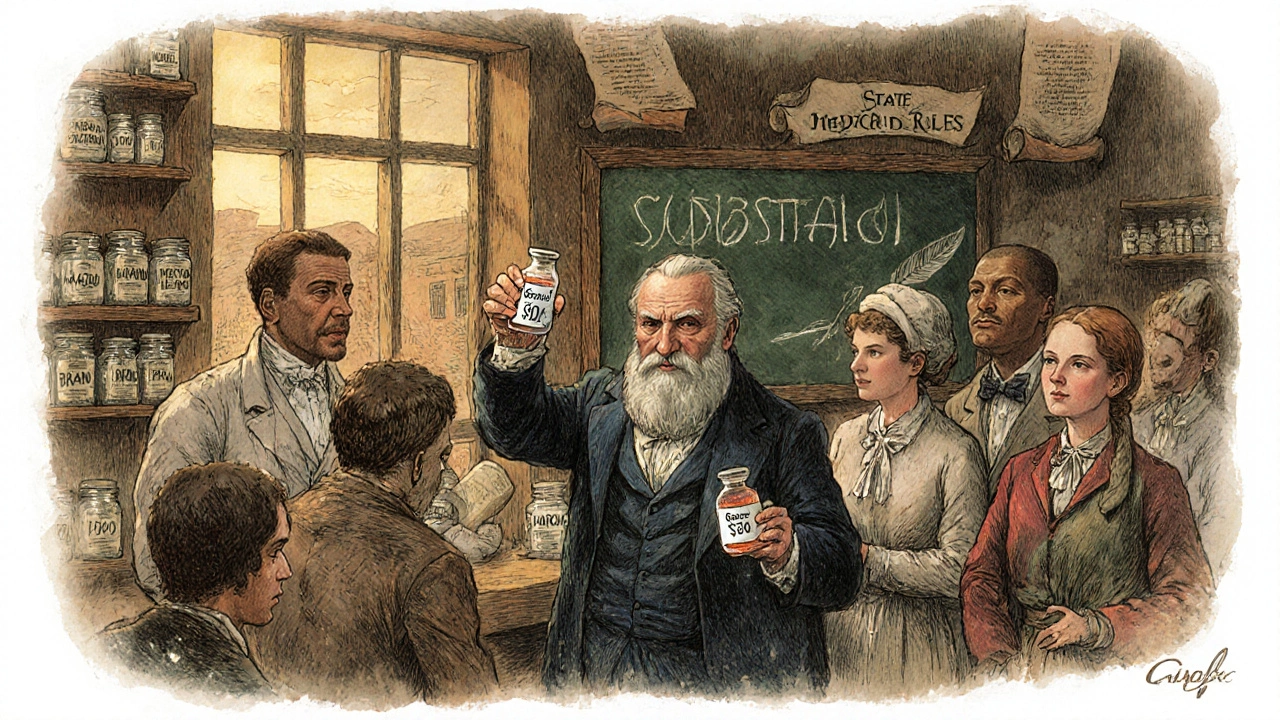
Medicaid PDLs: What You Need to Know About Covered Drugs and Restrictions
When you're on Medicaid PDLs, Preferred Drug Lists used by state Medicaid programs to control costs and guide prescribing. Also known as formularies, these are the official lists of medications that Medicaid will pay for — and which ones it won’t, unless your doctor jumps through extra hoops. If you’ve ever been told your prescription isn’t covered, or that you need prior authorization, you’re dealing with a Medicaid PDL.
Each state runs its own Medicaid program, and that means Medicaid PDLs, state-specific lists of approved medications. Also known as preferred drug lists, they vary widely across the U.S.. One state might cover a generic version of a drug while another only approves the brand name. Some states require you to try cheaper options first — a process called step therapy. Others block certain drugs entirely unless you have a rare diagnosis or your doctor proves it’s medically necessary. These rules aren’t random. They’re based on cost, clinical evidence, and sometimes political pressure. And while they’re meant to save money, they often create delays, confusion, and even health risks for patients who need timely care.
Related to this are state drug laws, rules governing how pharmacists can substitute generic drugs for brand-name ones. Also known as generic substitution rules, they work hand-in-hand with PDLs to control spending. If your drug isn’t on the PDL, your pharmacist might still be able to swap it for a cheaper generic — but only if state law allows it. Some states ban substitutions for drugs like seizure meds or blood thinners, even if they’re technically equivalent. That’s why knowing your state’s rules matters just as much as knowing your PDL. And if you’re on multiple medications — say, for diabetes, high blood pressure, or autoimmune disease — the interaction between these lists and your prescriptions can get messy fast.
Medicaid PDLs don’t just affect patients. They shape how doctors write prescriptions, how pharmacies stock shelves, and even how drug companies price their products. If a drug isn’t on the list, manufacturers often lower prices or offer rebates just to get included. That’s why you’ll see some drugs suddenly become available after a year-long wait — it’s not a medical breakthrough, it’s a financial deal.
Below, you’ll find real stories and guides from people who’ve dealt with these restrictions firsthand. From fighting a denied claim for a diabetes drug to understanding why your arthritis med got pulled from coverage, these posts give you the tools to navigate the system — not just accept it. Whether you’re a patient, caregiver, or healthcare worker, knowing how Medicaid PDLs work can save you time, money, and stress.
States are using copay differentials, preferred drug lists, and pharmacist substitution rules to push patients toward cheaper generic drugs. These policies save billions-but can also cause shortages if manufacturers pull out due to rebate rules.