Hospital Medication Safety: Protecting Patients from Errors and Interactions
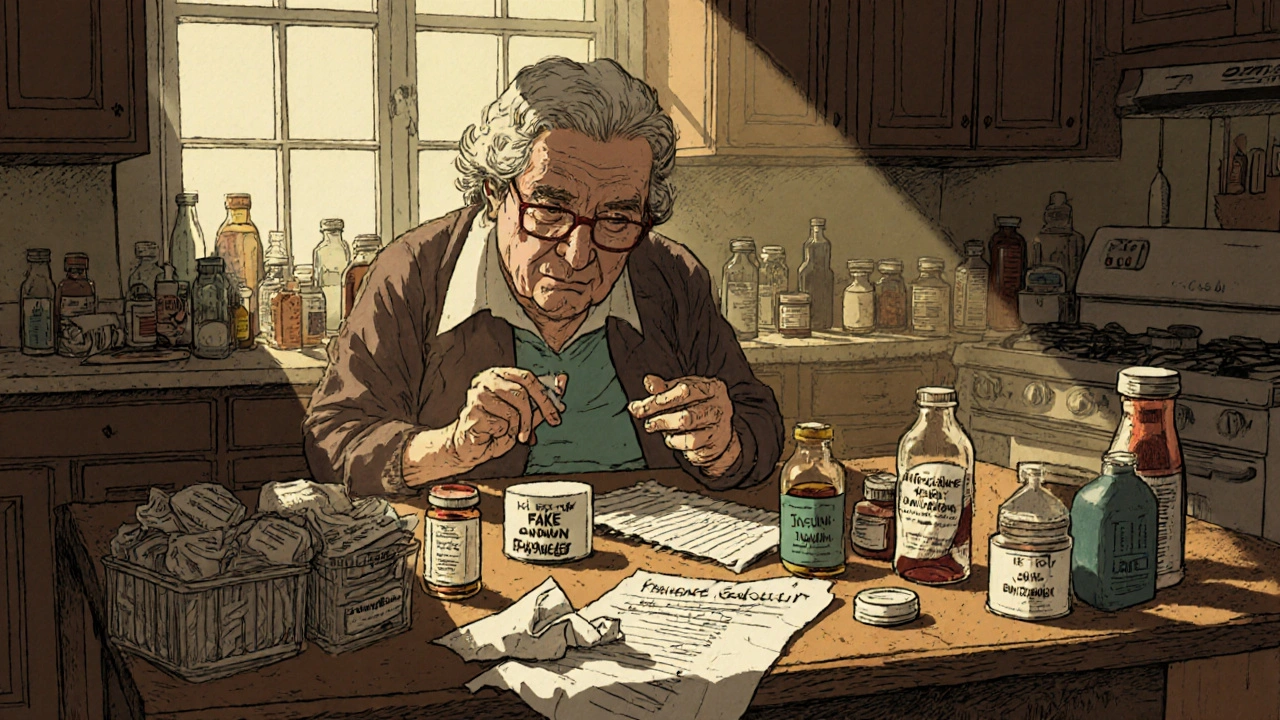
When you’re in the hospital, hospital medication safety, the system of checks, training, and protocols designed to prevent harmful drug mistakes in clinical settings. Also known as inpatient drug safety, it’s not just about giving the right pill—it’s about making sure the right person gets it, at the right time, in the right way, without dangerous clashes with other drugs or conditions. Every year, thousands of patients suffer because of simple oversights: a nurse misreads a label, a doctor doesn’t check for allergies, or two medications interact in a way no one warned about. These aren’t rare accidents—they’re preventable failures in a system that’s supposed to protect you.
drug interactions, when two or more medications affect each other’s behavior in the body, often leading to reduced effectiveness or dangerous side effects are one of the biggest threats. Take beta-blockers and calcium channel blockers: used together for high blood pressure, they can slow your heart too much if the wrong types are mixed. Or goldenseal and metformin—herbal supplements you might think are harmless can tank your blood sugar control if you’re diabetic. Even something as common as doxycycline can turn a sunny day into a painful burn if you don’t know about its photosensitivity, an increased risk of severe sunburn caused by certain medications. These aren’t theoretical risks. They show up in real hospital reports, ER visits, and patient stories.
medication errors, mistakes in prescribing, dispensing, or administering drugs that lead to patient harm happen at every step. A pharmacist might swap a brand for a generic because of state rules—and if you’re on a critical drug like tacrolimus, that change can be risky if not monitored. A nurse might miss a warning because the system is overloaded. A patient might not speak up because they’re scared or confused. That’s why tools like a personal medication list, double-checking labels, and asking questions aren’t optional—they’re survival skills. And it’s not just about the drugs themselves. It’s about the people behind them: understaffed hospitals, overworked pharmacists, and patients who don’t know how to advocate for themselves.
Some of these problems are being fixed. States are pushing for generic substitution laws to cut costs, but those same laws can cause shortages if manufacturers stop making cheap versions. Pharmacies are getting certified to fight counterfeit drugs, and new tech helps track dosing in real time. But none of it replaces the human element: a nurse pausing to confirm a name, a doctor asking about herbal supplements, a patient saying, "Wait, this pill looks different." That’s where real safety starts.
Below, you’ll find real, practical guides on exactly what to watch for—whether you’re taking diabetes meds, antibiotics, heart drugs, or pain relievers. No theory. No fluff. Just what works, what doesn’t, and how to keep yourself safe when you’re most vulnerable.
Medication errors harm millions each year-but most are preventable. Learn how hospitals and homes can stop wrong doses, fake drugs, and dangerous mix-ups with proven strategies that actually work.