Generic Prescribing Incentives: How Policies Shape Your Medication Choices
When your doctor writes a prescription, generic prescribing incentives, financial or policy-driven motivations that encourage the use of lower-cost generic drugs over brand-name versions. Also known as generic substitution incentives, these are built into insurance plans, hospital budgets, and state laws to reduce overall drug spending without lowering treatment quality. This isn’t about cutting corners—it’s about using the same active ingredients at a fraction of the price. For example, generic lisinopril works just like Prinivil, but costs 90% less. In many cases, the only difference is the color of the pill or the name on the label.
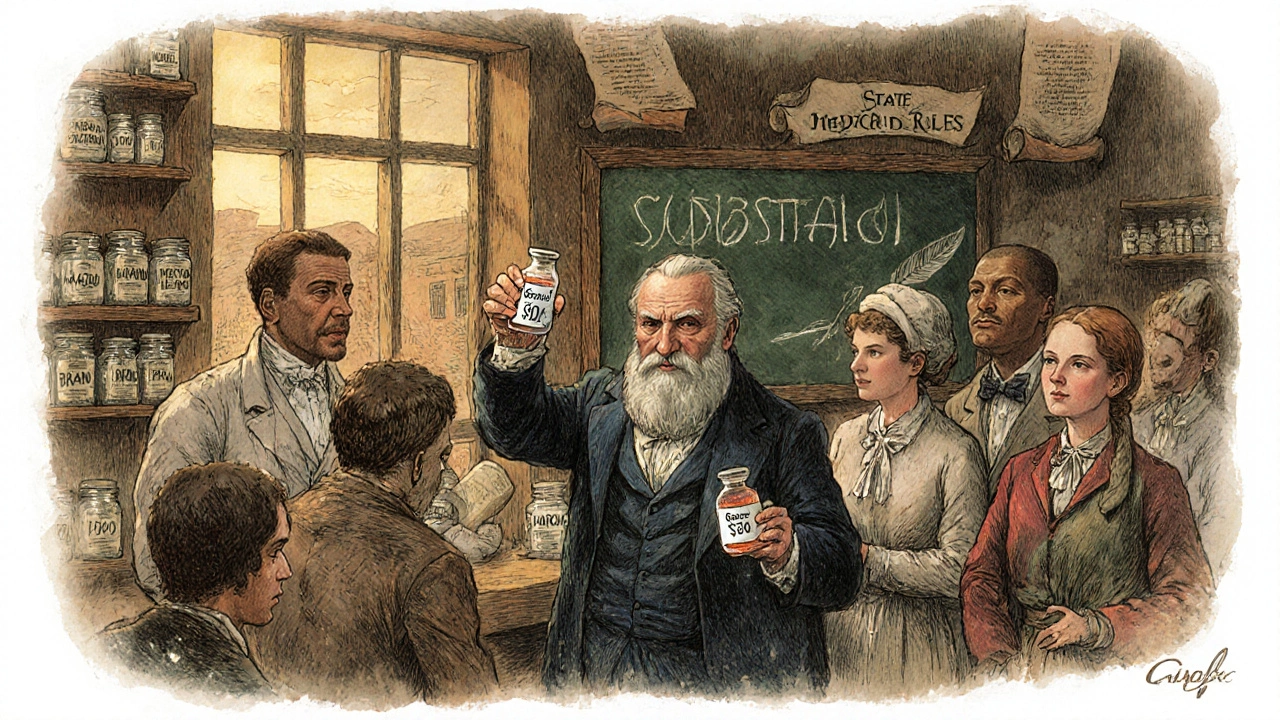
These incentives don’t happen in a vacuum. They’re tied to generic drugs, medications approved by the FDA as bioequivalent to brand-name versions, with identical active ingredients, dosage, and effectiveness, and the rules around how pharmacists can swap them. In some states, pharmacists can automatically substitute generics unless the doctor says "dispense as written." In others, they must ask the patient first. That’s why pharmacist substitution rules, state-specific regulations governing when and how a pharmacist can replace a brand-name drug with a generic vary so much across the U.S. One person might get a generic version without even knowing it; another might be handed the brand name simply because the pharmacist wasn’t allowed to switch.
These policies also connect to therapeutic equivalence, the scientific standard that confirms two drugs—brand and generic—produce the same clinical effect and safety profile. Not all generics are treated the same. For drugs with narrow therapeutic windows—like warfarin or levothyroxine—even tiny differences in absorption can matter. That’s why some doctors avoid switching, and why state laws sometimes restrict substitutions for these meds. But for most common conditions—high blood pressure, cholesterol, depression—generic drugs are just as safe and effective. The real question isn’t whether they work. It’s whether you’re being given the best option for your budget and health.
Behind the scenes, hospitals and insurers push these incentives because they work. A single switch from brand to generic can save a patient hundreds a year—and the system thousands. But that doesn’t mean every patient gets the same experience. Some are never told they’re on a generic. Others are pressured to switch, even when their current brand is working fine. And sometimes, the pharmacy runs out of the generic and gives you the brand without asking—costing you more. It’s not always transparent, and it shouldn’t be left to chance.
What you’ll find in the posts below are real stories and clear explanations about how these systems play out. From state laws forcing or blocking substitutions, to how pharmacists navigate the gray areas, to what happens when a patient gets the wrong drug because of a policy loophole. You’ll see how generic prescribing incentives touch everything—from the cost of your monthly script to whether your insurance covers it at all. These aren’t abstract policies. They’re decisions that land right in your hands when you pick up your medicine.
States are using copay differentials, preferred drug lists, and pharmacist substitution rules to push patients toward cheaper generic drugs. These policies save billions-but can also cause shortages if manufacturers pull out due to rebate rules.