Common Medical Myths: Debunking False Beliefs About Drugs, Treatments, and Health
When it comes to your health, common medical myths, widespread false beliefs about how drugs and treatments work. Also known as health misconceptions, these ideas spread fast because they sound reasonable—but they’re often wrong, dangerous, or both. You’ve probably heard that generic drugs aren’t as good as brand-name ones, or that antibiotics can treat a cold. Maybe you think if a little pill helps, a lot must help more. These aren’t just harmless rumors—they lead to wrong dosing, missed diagnoses, and even hospital visits.
Generic drugs, medications that contain the same active ingredient as brand-name versions at a fraction of the cost. Also known as generic medications, they’re held to the same strict FDA standards for safety and effectiveness. The only difference? Color, shape, or filler ingredients—none of which change how the drug works. Yet people still avoid them out of fear. Meanwhile, antibiotic use, the treatment of infections with drugs that kill bacteria. Also known as antibacterial therapy, it’s one of the most misunderstood areas in medicine. Millions take antibiotics for viral infections like the flu or sore throat, not realizing it does nothing—and makes future infections harder to treat. This isn’t just wasteful; it’s fueling drug-resistant superbugs.
Another myth? That natural supplements are always safe. Goldenseal might sound harmless, but it can interfere with metformin and spike blood sugar in diabetics. Ginger helps with morning sickness, but that doesn’t mean all herbal remedies are fine during pregnancy. Even something as simple as OTC cold medicine can be deadly if you’re on warfarin. These aren’t edge cases—they’re everyday risks hiding in plain sight.
And what about those scary side effects? Some people stop taking meds because they read about a rare reaction online. But side effects don’t happen the same way for everyone. Loperamide overdose? It’s rare—but it happens when people take 20 pills thinking it’ll stop diarrhea faster. Theophylline toxicity? It creeps up slowly if blood levels aren’t checked. Timing matters. Dose matters. Your health history matters. One-size-fits-all advice gets people hurt.
There’s also the myth that if you feel fine, you don’t need monitoring. Silent gallstones? They’re common and harmless—unless they suddenly block a duct. QT prolongation from azithromycin? Most people are fine, but if you have heart issues or take other drugs, it’s a real risk. ECGs aren’t just paperwork—they’re lifesavers for the right people.
These myths persist because they’re simple. Real medicine? It’s messy. It depends on your age, weight, other meds, liver function, genetics. That’s why you can’t trust a TikTok video or a friend’s story. You need facts—not folklore.
Below, you’ll find real stories from real patients and real science. We cover how generics look different but work the same. Why you shouldn’t mix cold meds with blood thinners. When antibiotics actually need an ECG. How to spot a fake pharmacy. What to do when side effects show up weeks later. No fluff. No hype. Just what you need to know to stay safe.
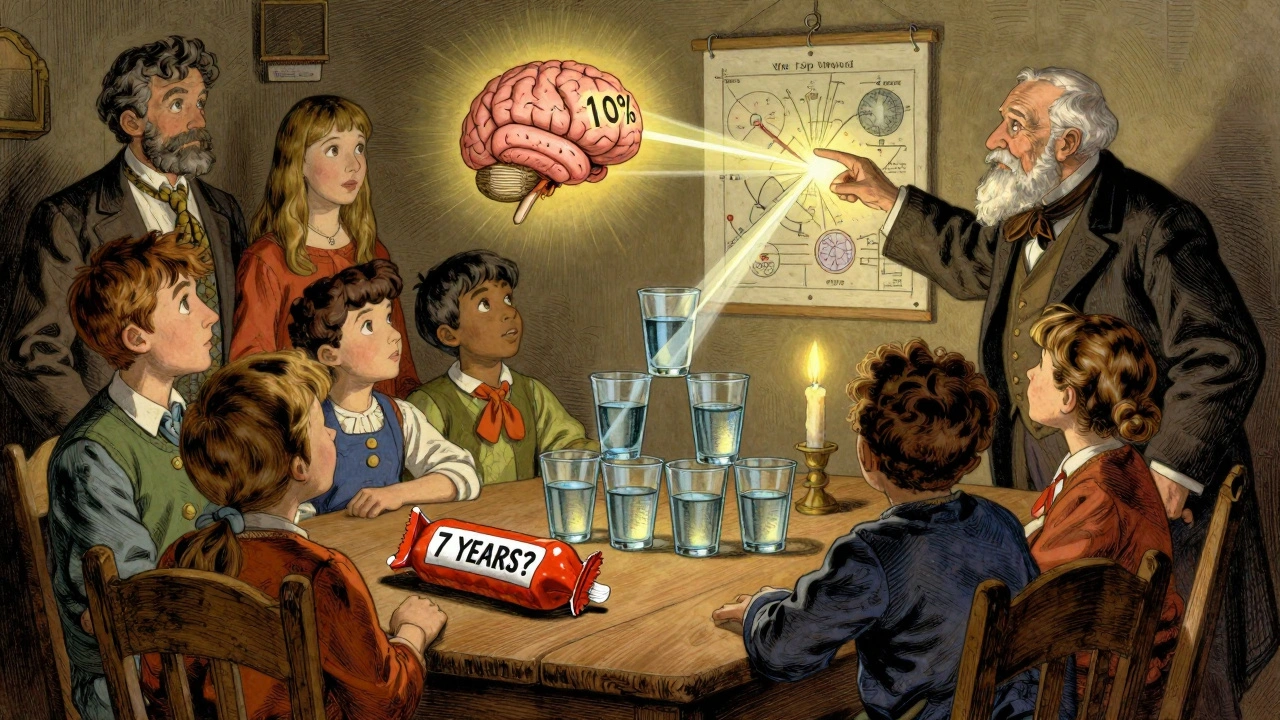
Debunking common health myths like drinking eight glasses of water, sugar causing hyperactivity, and only using 10% of your brain. Learn the facts behind the myths and how to spot false health claims.