Cardiac Effects: How Medications Impact Your Heart and What You Need to Know
When you take a pill for diabetes, infection, or high blood pressure, you might not think about your heart, the muscle that pumps blood through your body and is sensitive to chemical changes from drugs. Also known as the cardiovascular system, your heart doesn’t just beat on its own—it reacts to what you swallow. Many drugs, even ones you think are harmless, can cause cardiac effects, changes in heart rhythm, rate, or function caused by medications. These aren’t rare side effects—they’re documented, measurable, and sometimes deadly.
Take loperamide, an over-the-counter anti-diarrhea drug that, when misused, can trigger fatal heart rhythm problems. Or doxycycline, an antibiotic that doesn’t just make you sun-sensitive—it can also stress your heart by lowering potassium levels. Even common drugs like indapamide, a diuretic used for high blood pressure, can throw off your electrolytes and lead to irregular beats. These aren’t hypothetical risks. Studies show that drug-induced arrhythmias send tens of thousands to the ER every year. And it’s not just about overdoses. Sometimes, it’s just the combo of two pills you’ve been taking for months.
The biggest danger? You won’t always feel it coming. A slow heartbeat, skipped beats, or sudden dizziness might seem minor—until they’re not. That’s why knowing which drugs carry cardiac risks matters. If you’re on multiple medications, especially for diabetes, heart disease, or mental health, your heart is likely being affected in ways you don’t see. Some drugs lengthen the QT interval—a hidden timer in your heart’s electrical cycle. Stretch it too far, and you risk torsades de pointes, a type of rhythm that can stop your heart. Others, like certain antibiotics or antifungals, interfere with potassium channels. And herbal supplements? Goldenseal, berberine, and others can mess with how your body processes heart meds, raising blood sugar or lowering potassium without warning.
This isn’t about scaring you off your prescriptions. It’s about awareness. Many of the posts here focus on exactly these hidden connections: how a diabetes drug interacts with an herb, how a common painkiller can raise blood pressure, how a simple antibiotic can cause dangerous sunburns and heart strain at the same time. You’ll find real examples of what happens when meds collide, how to spot early warning signs, and what questions to ask your pharmacist before you take that next pill. The goal isn’t to stop treatment—it’s to make sure your treatment doesn’t accidentally harm the very organ you’re trying to protect.
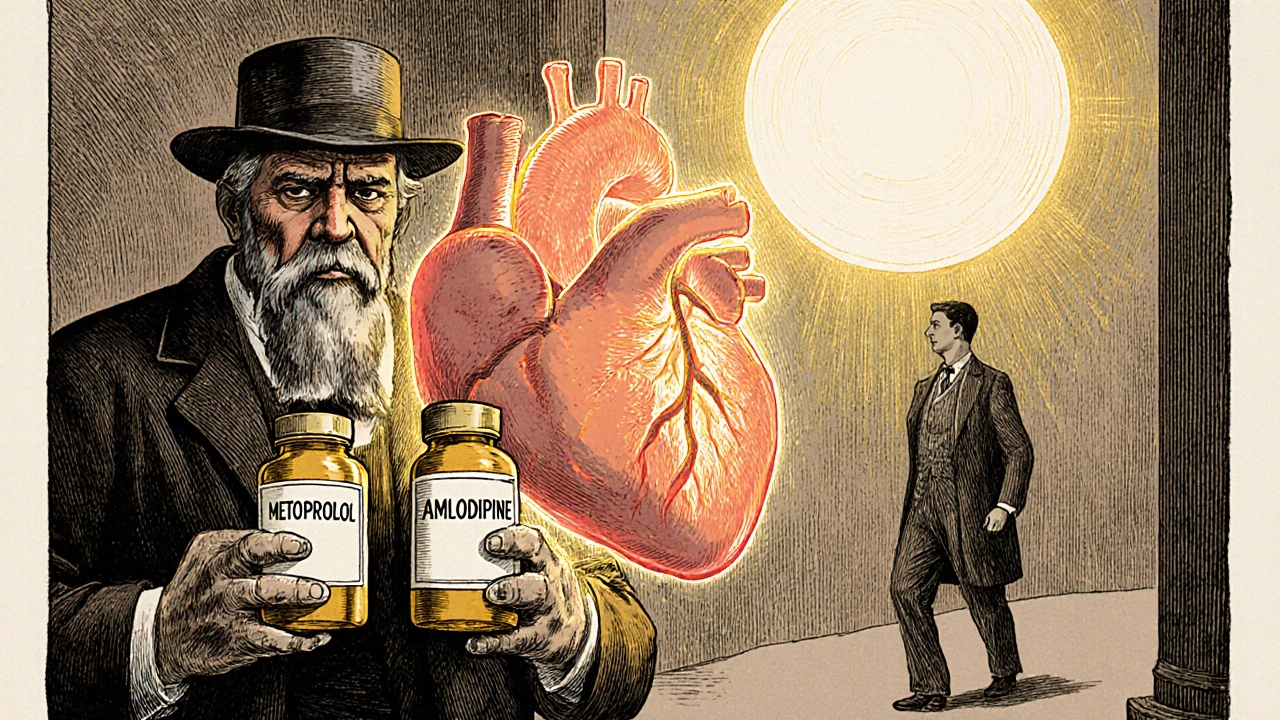
Beta-blockers and calcium channel blockers can be effective together for high blood pressure and angina, but only if the right types are used. Combining certain versions can cause dangerous heart slowdowns-here's what you need to know.