Rosuvastatin Side Effect Risk Calculator
Dose Summary
LDL Reduction
Clinical studies show 20mg typically reduces LDL-C by 45-63%.
Risk Indicators
Monitoring Recommendations
| Test | When to Test | Abnormal Value Threshold |
|---|---|---|
| ALT/AST | Baseline + 3 months, then annually | 1.5x ULN |
| CK | Only with symptoms | 5x ULN |
| eGFR | Baseline + every 6-12 months | eGFR < 60 |
| HbA1c | Baseline for at-risk patients | 5.7%+ |
Rosuvastatin is a synthetic HMG‑CoA reductase inhibitor marketed as Crestor, approved in 2003 for dyslipidemia and cardiovascular risk reduction. It boasts roughly 15‑ to 20‑fold greater rosuvastatin potency than atorvastatin on a milligram‑to‑milligram basis, delivering 45‑63% LDL‑cholesterol cuts at doses from 5 mg to 40 mg. Because of its high‑intensity classification, clinicians must pair its efficacy with a clear monitoring plan to catch liver, muscle, renal, and metabolic issues early.
How Rosuvastatin Works and Why It’s Considered Highly Potent
Rosuvastatin competitively blocks the HMG‑CoA reductase enzyme, the rate‑limiting step in cholesterol synthesis. Its hydrophilic structure limits passage across the blood‑brain barrier, which reduces central nervous system exposure compared with lipophilic statins like simvastatin. Only about 10% of the dose is metabolized by CYP2C9, giving it a cleaner drug‑interaction profile than statins heavily processed by CYP3A4.
Key pharmacokinetic facts:
- Molecular formula: C22H28FN3O6S (MW 481.54 g/mol)
- Half‑life ≈ 19 hours - supports once‑daily dosing
- Absolute bioavailability 50‑60%
- Peak plasma 3‑5 hours after oral intake
Typical Lipid‑Lowering Results
Clinical trials consistently show that 20 mg of rosuvastatin reduces LDL‑C by ~55%, outperforming atorvastatin (≈ 39‑41% at 20‑40 mg) and simvastatin (≈ 25‑35%). The JUPITER and METEOR studies linked these reductions to a 44% drop in major cardiovascular events among high‑risk patients.
Guideline‑driven dosing (ACC/AHA 2018) defines high‑intensity therapy as 20‑40 mg daily, which is where you see the greatest LDL‑C impact.
Side‑Effect Profile You Need to Know
While overall tolerability is good, certain adverse effects appear more often with higher doses:
- Myalgia and muscle cramps - reported by ~9‑10% of users; severe rhabdomyolysis is rare (<0.02%).
- Elevated liver enzymes (ALT/AST) - monitoring needed at baseline; discontinuation if >3× ULN.
- Proteinuria - risk rises 2.3‑fold at 40 mg versus 10 mg.
- New‑onset diabetes - 9‑12% increased incidence; HbA1c should be checked in at‑risk patients.
- Rare cognitive complaints (1‑2%); usually reversible after stopping the drug.
Patient‑reported data from Drugs.com and Reddit echo these trends: muscle pain spikes at 20‑40 mg, while many tolerate 5‑10 mg without trouble.

Laboratory Monitoring - What to Order and When
Start with a baseline panel before the first dose:
- ALT and AST (liver enzymes)
- Creatine kinase (CK) - only if there’s a history of muscle issues
- Estimated glomerular filtration rate (eGFR)
- HbA1c (if diabetic risk factors exist)
Follow‑up schedule:
- ALT/AST: re‑check at 3 months, then yearly if stable.
- CK: test only when the patient reports unexplained muscle pain, weakness, or dark urine. Stop the drug if CK >5× ULN (≈ 1,000 U/L).
- eGFR: repeat every 6‑12 months; dose‑adjust or avoid 40 mg if eGFR <60 mL/min/1.73 m², and contraindicated if <30 mL/min/1.73 m².
- HbA1c: check annually, or sooner if fasting glucose rises.
These checkpoints align with the Specialist Pharmacy Service (2022) and Mayo Clinic guidelines.
Renal Considerations - Dose Adjustments
Because rosuvastatin is eliminated primarily via the kidneys, impaired renal function amplifies exposure. Recommended doses:
- eGFR ≥ 60 mL/min: full range 5‑40 mg.
- eGFR 30‑59 mL/min: max 10 mg; avoid 20‑40 mg.
- eGFR < 30 mL/min: rosuvastatin is contraindicated.
Clinicians should document renal function before each dose escalation.
How Rosuvastatin Stacks Up Against Other Statins
| Statin | Typical High‑Intensity Dose | LDL‑C Reduction (%) | Key Metabolism Pathway | Renal Dose Adjustment |
|---|---|---|---|---|
| Rosuvastatin | 20‑40 mg | 55‑63 | CYP2C9 (≈10% metabolism) | Reduce to ≤10 mg if eGFR 30‑59; avoid ≥20 mg if <30 |
| Atorvastatin | 40‑80 mg | 39‑41 | CYP3A4 (major metabolism) | No specific renal limit, but watch for accumulation |
| Simvastatin | 20‑40 mg | 25‑35 | CYP3A4 (highly metabolized) | Standard dosing; avoid in severe renal disease due to active metabolites |
The table highlights why rosuvastatin is the go‑to high‑intensity option when maximal LDL‑C reduction is needed and drug‑interaction risk must stay low.
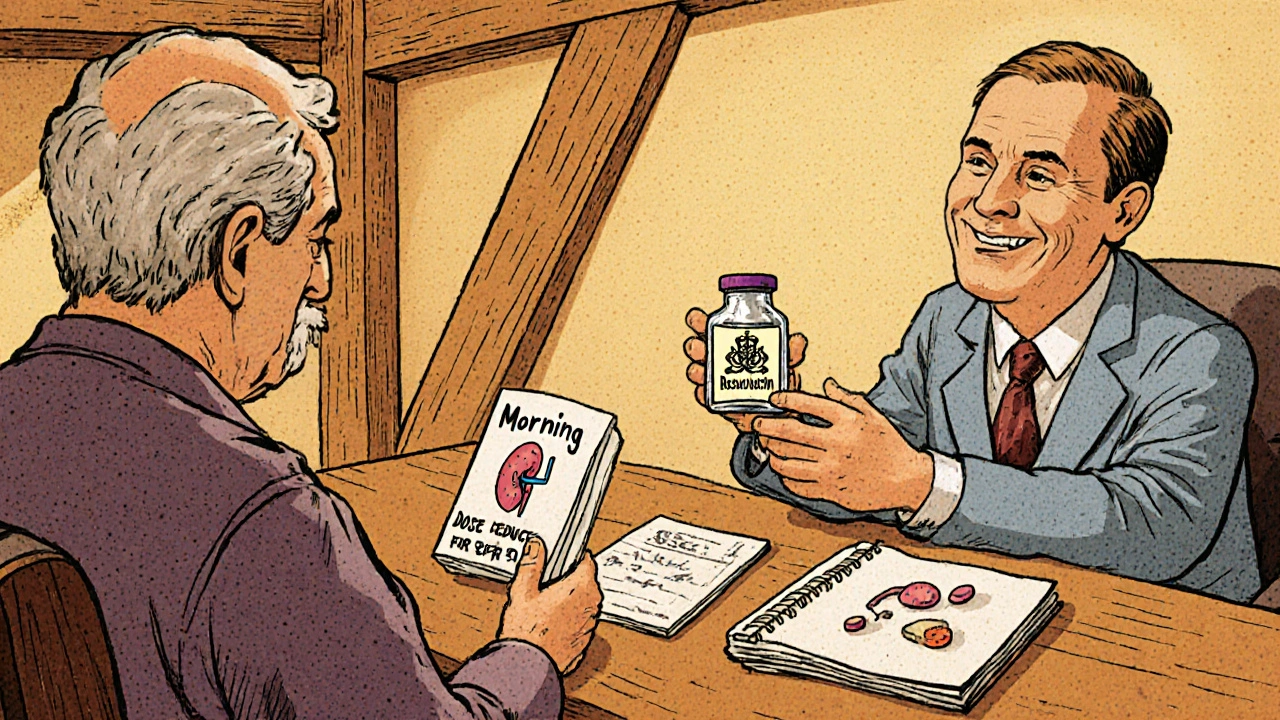
Practical Tips for Clinicians and Patients
For clinicians:
- Start low (5‑10 mg) in patients with prior muscle complaints; titrate up only if LDL goals aren’t met.
- Use electronic health record alerts for eGFR checks before each refill.
- Educate patients: mild aches are common and often self‑limited; severe pain, dark urine, or unexplained weakness = immediate CK test.
- Consider genetic testing for SLCO1B1 variants in patients with recurrent myopathy.
For patients:
- Take the tablet at the same time each day, with or without food.
- Report any new muscle soreness, especially if it’s accompanied by fever or urine that looks tea‑colored.
- Maintain a healthy diet and regular exercise; these amplify statin benefits.
- Keep a log of your latest labs (ALT, AST, CK, eGFR) and share it at each visit.
Key Takeaways
- Rosuvastatin is one of the most potent statins, dropping LDL‑C by up to 63% at high doses.
- Major side effects include muscle pain, liver enzyme elevation, proteinuria, and modest diabetes risk.
- Baseline and periodic labs (ALT/AST, CK when symptomatic, eGFR, HbA1c) are essential to safe use.
- Renal impairment demands dose reduction; avoid 40 mg if eGFR <60 mL/min/1.73 m².
- Compared with atorvastatin and simvastatin, rosuvastatin offers stronger LDL reduction and fewer CYP‑mediated interactions, but watch for renal dosing and proteinuria.
Frequently Asked Questions
How quickly does rosuvastatin lower LDL cholesterol?
Most patients see a 30‑40% drop within 2‑4 weeks; full effect (45‑63% reduction) is typically reached by 8‑12 weeks at high‑intensity doses.
Do I need routine liver tests if I feel fine?
Current ACC/AHA guidance says routine tests aren’t required for asymptomatic patients, but a baseline ALT/AST is still recommended and repeat if symptoms arise.
What dose is safe for someone with mild kidney disease?
If eGFR is 30‑59 mL/min/1.73 m², limit rosuvastatin to 10 mg daily. Avoid 20‑40 mg and never use 40 mg when eGFR falls below 60.
Can rosuvastatin cause diabetes?
Statins increase fasting glucose modestly (5‑10 mg/dL) and HbA1c by 0.1‑0.3%. Patients with pre‑diabetes should be monitored with HbA1c every 6‑12 months.
When should I stop rosuvastatin immediately?
Stop if ALT/AST rise >3× ULN, CK >5× ULN with symptoms, or if severe proteinuria or rhabdomyolysis is confirmed.





Nic Floyd
Rosuvastatin’s hydrophilic moiety grants it a distinct distribution profile compared with lipophilic statins.
The molecule’s affinity for HMG‑CoA reductase is roughly fifteenfold higher than that of atorvastatin, which translates into superior LDL‑C reductions per milligram.
Clinical pharmacology literature cites a half‑life of about 19 hours, supporting a convenient once‑daily dosing schedule.
Because only ten percent undergoes CYP2C9 metabolism, the drug‑interaction burden is markedly lower than that of simvastatin which relies heavily on CYP3A4.
The bioavailability hovering around fifty to sixty percent ensures consistent systemic exposure across patient populations.
When titrated to 20 mg, rosuvastatin typically drives LDL‑C down by fifty‑five percent, outpacing many high‑intensity regimens.
This potency, however, is accompanied by a dose‑related increase in myalgia incidence, reported in roughly nine to ten percent of users.
Healthcare providers should therefore schedule baseline CK measurements in patients with a history of muscle disorders.
Renal function monitoring via eGFR is advisable, especially when prescribing the 40 mg strength, as proteinuria risk escalates two‑fold.
Emerging data also suggest a modest elevation in new‑onset diabetes risk, warranting periodic HbA1c assessments in susceptible individuals.
Liver enzyme surveillance remains essential; ALT and AST should be rechecked at three months post‑initiation and annually thereafter if stable.
In rare instances, reversible cognitive complaints have been documented, prompting clinicians to counsel patients on potential central effects.
Patient adherence can be bolstered by clear communication of the benefit‑risk balance, emphasizing that the absolute reduction in cardiovascular events approaches forty‑four percent in high‑risk cohorts.
From a formulary perspective, rosuvastatin’s once‑daily dosing and modest drug‑interaction profile often make it a cost‑effective choice despite its higher acquisition price.
🩺💊✨ Ultimately, the key to maximizing therapeutic outcomes lies in individualized dosing, vigilant monitoring, and patient education.
Erik Redli
This hype is overblown, rosuvastatin isn’t a miracle drug.
Tim Waghorn
The pharmacodynamic profile of rosuvastatin is well‑characterized and warrants rigorous adherence to monitoring protocols.
Baseline assessments should include hepatic transaminases, creatine kinase, estimated glomerular filtration rate, and glycated hemoglobin where indicated.
Subsequent re‑evaluation of ALT and AST at three months aligns with current ACC/AHA recommendations.
It is imperative to document any muscle‑related symptoms and obtain CK values only upon clinical indication.
Brady Johnson
The shadow of muscle toxicity looms larger than most clinicians admit, turning a routine prescription into a ticking time‑bomb.
Patients often dismiss subtle myalgias until the damage becomes irreversible, a tragedy that the medical community seems content to overlook.
Such negligence transforms a life‑saving drug into a silent predator.
Paul Luxford
While the potency of rosuvastatin is undeniable, the emphasis on patient education can mitigate many of the reported adverse events.
A collaborative approach between prescriber and patient fosters adherence and early detection of side effects.
By sharing monitoring schedules transparently, we empower individuals to take charge of their cardiovascular health.
Johnae Council
Oh great, another “miracle pill” that needs a lab work marathon to stay safe.
Who has time between work, family, and now endless blood draws?
Guess we’ll just trust the pharma giants and hope for the best.
Manoj Kumar
In the grand theater of medicine, rosuvastatin plays the role of the diligent protagonist, quietly reshaping lipid landscapes.
Yet we must remember that every drug is but a fleeting actor on the stage of human biology, subject to the whims of genetics and lifestyle.
Embracing this perspective, we can view monitoring not as a chore but as an ongoing dialogue with our own physiology.
Ultimately, the journey toward cardiovascular wellness is a collaborative narrative, and rosuvastatin is merely one chapter in a much larger story.
Hershel Lilly
The recommendation to repeat eGFR every six to twelve months aligns well with the drug’s renal clearance considerations.
It is reassuring to see the guideline emphasize CK testing only when clinically indicated, reducing unnecessary interventions.
Such nuanced recommendations reflect a mature understanding of risk‑benefit stratification.
Carla Smalls
Great summary! Your clear outline of baseline labs and follow‑up intervals makes it easy for clinicians to implement.
Keep up the excellent work in demystifying complex medication regimens.
Your effort will undoubtedly improve patient outcomes.
Monika Pardon
One cannot help but notice the subtle choreography orchestrated by pharmaceutical conglomerates, wherein “monitoring protocols” conveniently generate a steady stream of laboratory revenue.
While the data appear robust, the timing of market releases often coincides with strategic lobbying efforts, a pattern that merits scrutiny.
In an era of transparency, it is prudent to question whether such intensive surveillance serves patient welfare or corporate profit.
Rhea Lesandra
Remember, consistency in monitoring is the cornerstone of safe statin therapy.
By integrating routine labs into the patient’s overall wellness plan, we not only track efficacy but also reinforce the therapeutic partnership, fostering trust and accountability across the care continuum.