Transplant Medications: What You Need to Know About Immunosuppressants and Side Effects
When you get a new organ, your body doesn’t know it’s supposed to accept it. That’s where transplant medications, drugs designed to suppress the immune system after organ transplantation to prevent rejection. Also known as immunosuppressants, they’re not optional—they’re life-saving. Without them, your body treats the new kidney, heart, or liver like an invader and tries to destroy it. This isn’t just theory. Studies show that without proper immunosuppression, over half of transplanted organs fail within the first year.
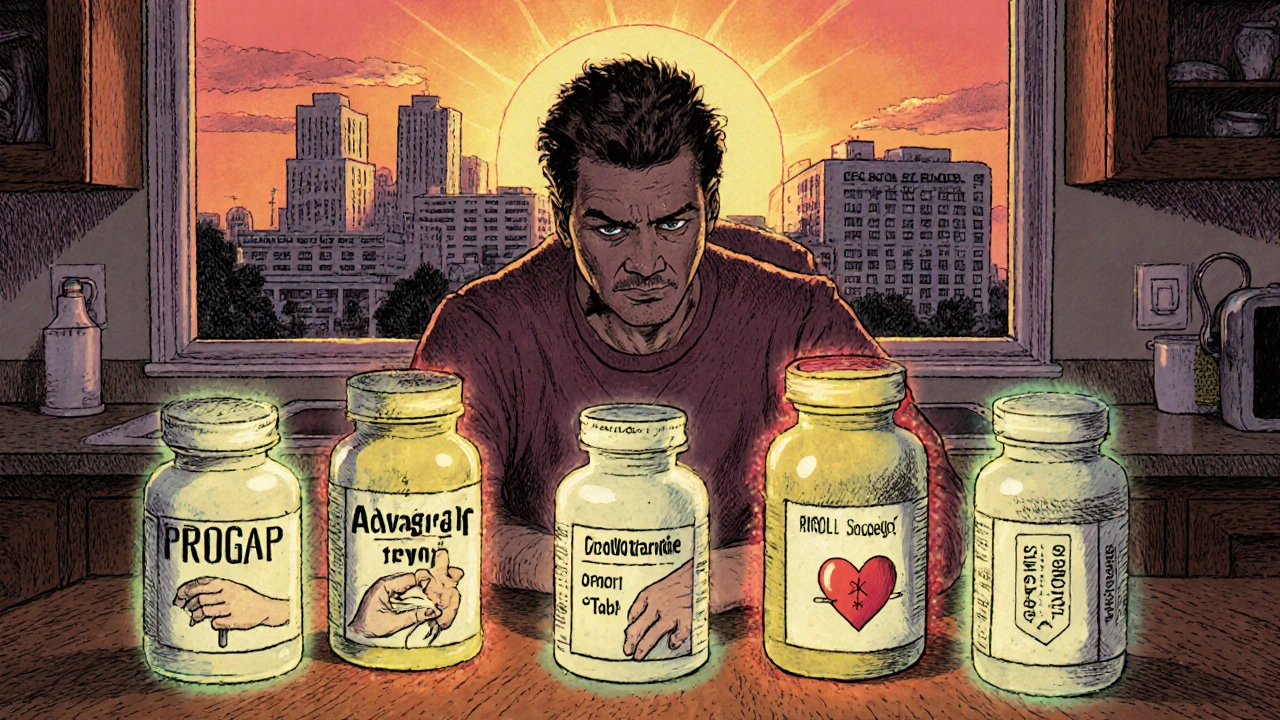
These drugs don’t work the same way. Some block signals between immune cells, others kill off aggressive cells, and a few stop the body from making new ones. Common ones include tacrolimus, a powerful calcineurin inhibitor used in kidney, liver, and heart transplants, cyclosporine, an older but still widely used drug that requires regular blood testing, and mycophenolate, a medication that stops immune cells from multiplying. Each has its own risks: kidney damage, high blood pressure, tremors, or increased infection risk. You’ll need blood tests every few weeks at first to make sure the dose is just right—not too high, not too low.
It’s not just about taking pills. These drugs interact with foods, other meds, and even herbal supplements. Grapefruit juice can make tacrolimus levels spike dangerously. Some antibiotics can make cyclosporine harder for your body to clear. Even something as simple as St. John’s wort can drop your drug levels enough to trigger rejection. That’s why every transplant patient gets a personalized plan—not just a list of drugs, but a full strategy for managing side effects, monitoring lab values, and spotting early warning signs like fever, swelling, or unexplained fatigue.
And it’s not just about the first year. Transplant medications are a lifelong commitment. Many people worry about long-term risks like cancer or diabetes, and rightly so. But skipping a dose or stopping cold turkey is far more dangerous. The goal isn’t to eliminate the immune system—it’s to balance it. Enough to protect the new organ, not so much that you’re always sick. The best outcomes come from people who stick with their plan, track their symptoms, and talk openly with their care team—even when it feels overwhelming.
Below, you’ll find real-world guides on how these drugs affect daily life, what to do when side effects hit, how to avoid dangerous interactions, and what alternatives exist when one drug stops working. These aren’t theoretical tips—they’re from people who’ve been there, and the doctors who help them stay healthy long after the surgery.
Compare Prograf (Tacrolimus) with alternatives like Advagraf, cyclosporine, sirolimus, and belatacept. Learn which drugs work best for transplant patients based on side effects, cost, and long-term outcomes.